Trusted by Healthcare ProfessionalsWeight Management Medications

Featured MedicationsExplore Weight Management products
WEIGHT MANAGEMENT CATEGORIESA patient-centered approach to weight management
Access patient specific medications for your clinic and patients or medications in large-scale for healthcare systems. Nationwide Shipping & Compliance Assurance – Serving clinics, hospitals, and wellness centers.
We follow the highest safety and quality standards in IV compounding. Our 503A and 503B IV medications are tested for sterility, potency, and endotoxins, ensuring compliance with cGMP, USP <797>, and FDA regulations.
Our streamlined operations and innovative manufacturing solutions enable efficient large-scale production, meeting the high demands of health systems, including pharmacies, clinics, and wellness centers nationwide.
FAQs
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
There are many ways to order at Empower Pharmacy, with an account. Here is a list of how you can order with us either through prescription or by office-use only.
For both Patient Specific and Office-Use Orders, if you would like to order online you can do so through our login page.
Patient Specific Prescription Orders (503A):
You may either use our portal (see link above), send a fax to (832) 678-4419, call in a prescription at (346) 229-5386, or send a prescription in through EMR.
Office-Use Orders (503B):
You may either use our portal (see link above), send a fax to (832) 678-4419, call in a prescription at (346) 229-5385, or email your order to officeuse@empowerpharmacy.com.
Yes, however, orders made in bulk for office-use only cannot be shipped to clinics in Alabama, and California. We can only provide patient-specific prescription products to these states.
A member from our Inbound team will reach out to you for each web form inquiry submitted. To ensure the quickest response time, please only submit one web form per inquiry. Submitting more than one may result in a longer response time. Currently, our turn around time is 3-7 business days depending on the request.
Yes. All of our medications require a prescription from a licensed prescriber. Your healthcare provider can call in your prescription at (877) 562-8577 or fax it to (832) 678-4419.
Yes. Interested healthcare providers will need to submit a completed questionnaire to Empower for approval to order controlled substances for office-use.

 Semaglutide / Methylcobalamin ODT
Semaglutide / Methylcobalamin ODT Semaglutide / Cyanocobalamin Injection
Semaglutide / Cyanocobalamin Injection Tirzepatide / Niacinamide Injection
Tirzepatide / Niacinamide Injection Tirzepatide ODT
Tirzepatide ODT Sermorelin Acetate Injection
Sermorelin Acetate Injection Vitamin B-Complex Injection
Vitamin B-Complex Injection Phentermine HCl Capsules
Phentermine HCl Capsules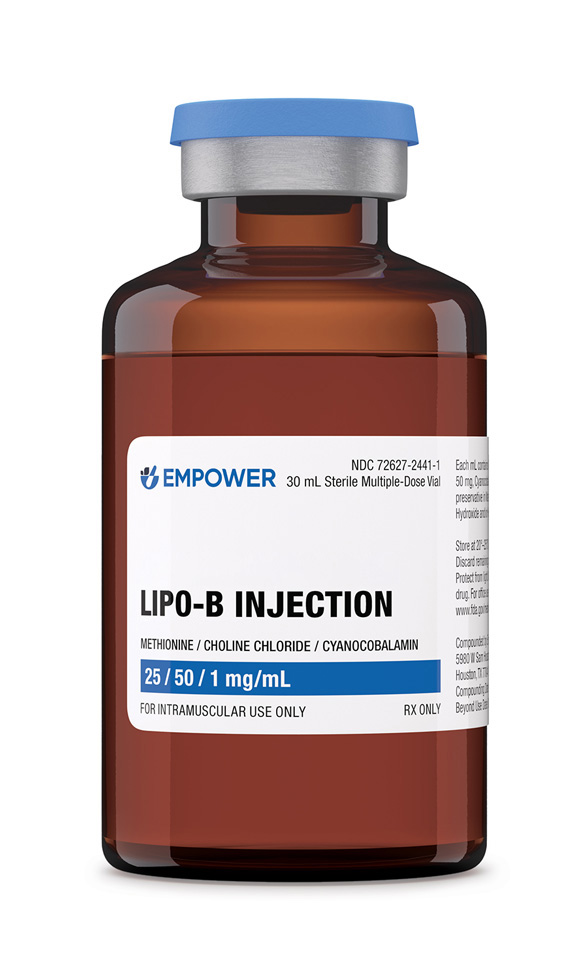 Lipo-B Injection
Lipo-B Injection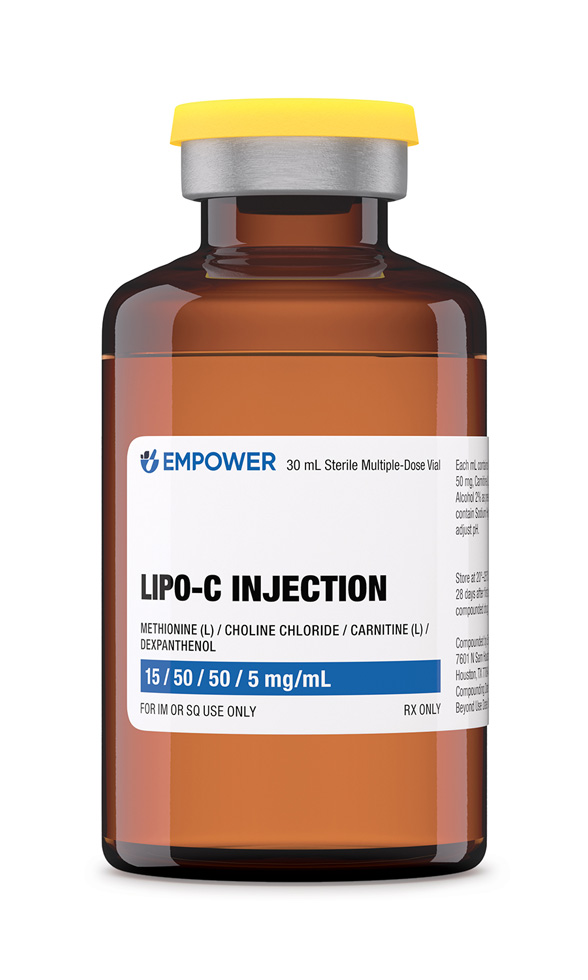 Lipo-C Injection
Lipo-C Injection Carnitine (L) Injection
Carnitine (L) Injection Thyroid Desiccated Porcine Capsules
Thyroid Desiccated Porcine Capsules







