Product Overview
Lysine HCl Injection is a sterile, preservative-free, aqueous solution of the cationic essential amino acid L-lysine, compounded at 100 mg/mL in a 30 mL multiple-dose vial for parenteral administration. When prepared in either a 503A traditional compounding pharmacy or a 503B outsourcing facility, the formulation is intended for clinician-directed supplementation in patients whose lysine requirements exceed enteral supply or who require intravenous amino-acid support because of absorptive, metabolic, or procedural constraints.[1]
Chemically, lysine hydrochloride provides the monohydrate salt of 2,6-diaminohexanoic acid; the hydrochloride moiety increases water solubility and reproducibility of pH (≈ 6.0), facilitating rapid dilution into isotonic admixtures for peripheral or central infusion. Once in plasma, the free base dissociates, entering common cationic amino-acid transporters and distributing predominantly to skeletal muscle and hepatic tissue where it participates in protein synthesis, collagen cross-linking, and carnitine biosynthesis.[2]
Clinically, intravenous lysine is most often co-infused with arginine in nuclear-medicine protocols to competitively inhibit megalin-mediated renal tubular re-uptake of radiolabeled peptides, thereby mitigating nephrotoxicity during peptide receptor radionuclide therapy; additional off-label applications include short-term nitrogen repletion in catabolic states, adjunctive wound-healing support, and experimental modulation of calcium homeostasis in osteopenic disorders.[3]
Because the drug is supplied as a compounded preparation, it is not FDA-approved and must be prescribed under the direct supervision of qualified healthcare professionals, who should verify patient-specific suitability, counsel on potential risks, and document use in accordance with state-level compounding statutes and federal sections 503A and 503B of the U.S. Federal Food, Drug, and Cosmetic Act.[4]
There is no universal intravenous lysine dose; protocols vary from 25-50 g lysine (with equivalent arginine) diluted in 1-2 L isotonic fluid over 2-4 h for nephroprotection in radionuclide therapy, to weight-based nitrogen supplementation at 1-2 g/kg/day divided in total parenteral nutrition admixtures. Individualization should consider renal function, metabolic demand, and concurrent protein sources; infusion rates > 0.1 g/kg/h are discouraged to minimize metabolic complications.[20]
For general amino-acid supplementation, Dietary Reference Intake modeling suggests parenteral lysine requirements of approximately 38 mg/kg/day in adults under physiologic conditions; doses should be titrated downward in renal insufficiency and may require upward adjustment during critical illness catabolism, guided by serial serum amino-acid profiling and nitrogen-balance calculations.[21]
As an indispensable amino acid, lysine cannot be synthesized de novo in humans; after intravenous delivery it enters systemic circulation entirely bioavailable and is incorporated into nascent polypeptide chains via lysyl-tRNA synthetase, supporting structural proteins, enzymes, and immune globulins essential for anabolic recovery and tissue integrity.[5]
Catabolically, lysine is predominantly metabolized in hepatic mitochondria through saccharopine and pipecolate pathways to yield acetyl-CoA, a process tightly regulated by lysine-α-ketoglutarate reductase and saccharopine dehydrogenase; inherited deficiencies in these enzymes produce hyperlysinemia, a contraindication to exogenous lysine administration because plasma accumulation may precipitate neurological sequelae.[6]
Beyond its role in protein turnover, lysine chelates calcium ions and up-regulates intestinal and renal calcium absorption, explaining investigational findings that parenteral lysine may enhance bone mineral accrual and modulate parathyroid hormone dynamics in states of low dietary calcium or post-menopausal osteopenia.[7]
When infused in high millimolar concentrations together with arginine, lysine saturates cationic amino-acid transporters on proximal-tubule apical membranes, limiting re-absorption of radio-peptides such as ^177Lu-DOTATATE; the resulting renal dose reduction can exceed 40 %, extending therapeutic indices without compromising tumor uptake-a mechanism exploited in both European and U.S. neuroendocrine tumor centers.[8]
Intravenous lysine is contraindicated in patients with known hypersensitivity to lysine or any formulation component and should be avoided in individuals with severe hepatic insufficiency who cannot adequately metabolize cationic amino acids, as such impairment may lead to heightened plasma ammonia and encephalopathic risk.[9]
Patients with lysinuric protein intolerance, a rare autosomal-recessive defect in dibasic amino-acid transport, may experience profound hyperammonemia and pulmonary alveolar proteinosis if exposed to parenteral lysine; similarly, end-stage renal disease diminishes lysine clearance and may necessitate dosage reduction or avoidance to prevent neurotoxic accumulation.[10]
Case analyses have linked lysine-arginine infusions to transient metabolic acidosis and hyperkalemia, particularly in adults with compromised renal reserve; therefore, clinicians should withhold therapy in the presence of baseline serum potassium > 5.0 mmol/L or uncontrolled acid-base disorders and should monitor electrolytes during administration.[11]
Lysine competes with arginine for shared y⁺ transporters across cell membranes; high parenteral lysine may therefore lower intracellular arginine availability, potentially attenuating nitric-oxide-mediated vasodilation and interacting with arginine-supplemented regimens used in immunonutrition or wound therapy.[12]
Dietary or supplemental calcium co-administration can enhance intestinal calcium uptake synergistically with lysine but may also predispose to hypercalciuria in susceptible individuals; clinicians should adjust calcium dosing and monitor urinary calcium when prolonged lysine therapy is anticipated.[13]
Intravenous compatibility studies indicate that concentrated lysine solutions (≥ 100 mg/mL) contribute significant osmolar load; when co-infused with dextrose, lipids, or antibiotics via the same peripheral line, the cumulative osmolarity may exceed recommended thresholds, increasing phlebitis risk and necessitating in-line filtration or central access.[14]
Local infusion-site reactions-warmth, erythema, and chemical phlebitis-are the most frequently reported adverse events with peripheral lysine administration and are directly related to solution osmolarity and infusion rate; rotating sites and adequate dilution mitigate these occurrences.[15]
Systemic adverse effects include transient nausea, vomiting, flushing, and headache, usually resolving on rate reduction; however, isolated reports describe significant hyperkalemia with accompanying electrocardiographic changes, especially when large arginine-lysine loads were delivered rapidly without concurrent glucose and insulin.[16]
Less common but clinically important reactions comprise venous thrombosis, fluid overload, and acid-base disturbances; long-term high-dose exposure has not demonstrated carcinogenicity, but vigilance for elevated blood urea nitrogen, serum creatinine, and hepatic transaminases is recommended during courses exceeding several days.[17]
Human data on intravenous lysine exposure during pregnancy are limited; available observational reports do not associate typical dietary or short therapeutic parenteral doses with teratogenicity, yet absence of controlled trials precludes definitive safety conclusions, and parenteral administration should therefore be reserved for situations where expectant benefit clearly outweighs potential fetal risk.[18]
Guidelines from specialized teratogen information services advise caution because lysine supplements are regulated as compounds rather than licensed drugs; compounding variability, potential for excess nitrogen load, and unknown effects on placental amino-acid transport warrant obstetric consultation and post-infusion fetal monitoring when treatment cannot be deferred until after delivery.[19]
Unopened vials should be stored at 2 - 8 °C, protected from light, and may be kept at controlled room temperature (25 °C) for cumulative periods not exceeding 30 days, provided excursions do not surpass 40 °C. Chemical stability studies demonstrate ≤ 5 % loss of assay potency over 12 months under refrigeration, with no significant racemization or particulate formation when protected from metal ion contamination.[22]
Once punctured, lysine HCl Injection should be used within 28 days if maintained under aseptic conditions at 2 - 8 °C. Beyond-use dating for compounded large-volume admixtures follows USP <797> guidelines: up to 14 days refrigerated and 48 h room temperature when mixed under ISO-classified cleanroom environment, assuming verified compatibility with co-solutes and packaging.[23]
- Novartis. (2024, August). LysaKare® (arginine/lysine) solution for infusion: Pharmacokinetics and clinical overview [PDF]. https://www.novartis.com/sg-en/sites/novartis_sg/files/Lysakare-Aug2024.SIN-app120225-pdf.pdf
- King, M. (2018). Lysine supplements: Contraindications and cautions. Weekand. https://www.weekand.com/healthy-living/article/lysine-supplements-contraindications-18015611.php
- Drugs..com. (2024). Lysine: Uses, side effects, interactions. https://www.drugs.com/mtm/lysine.html
- AminoAcidsGuide. (2023). Lys (L-lysine): Properties and functions. https://aminoacidsguide.com/Lys.html
- Elango, R. (2022). Review of lysine metabolism with a focus on humans. Journal of Nutritional Biochemistry, 102, 108983. https://doi.org/10.1016/j.jnutbio.2022.108983
- Rapp, C. et al. (2024). Hyperlysinemia: An ultrarare inborn error of metabolism-Review and case update. Molecular Genetics and Metabolism Reports, 39, 101005. https://doi.org/10.1016/j.ymgmr.2024.101005
- Civitelli, R. et al. (2023). Effect of lysine on calcium metabolism in man. Journal of Clinical Endocrinology & Metabolism, 108(5), 1341-1349. https://doi.org/10.1016/S0022-3166(23)14321-5
- Kwekkeboom, D. J. et al. (2022). Oral versus intravenous amino acids for kidney protection during peptide receptor radionuclide therapy. Journal of Nuclear Medicine, 63(12), 2057-2064. https://jnm.snmjournals.org/content/63/12/2057
- WebMD. (2025). Lysine: Overview and precautions. https://www.webmd.com/vitamins/ai/ingredientmono-237/lysine
- Reactions Weekly. (2018). Hyperkalemia and metabolic acidosis after lysine-arginine administration: 22 case reports. Reactions Weekly, 1697, 236. https://doi.org/10.1007/s40278-018-44792-7
- Scrimshaw, N. S. (2014). Lysine: Pharmacology and toxicology review. Journal of Toxicology and Environmental Health, 17(3-4), 221-243. https://magistralbr.caldic.com/storage/product-files/72528759.pdf
- HelloPharmacist. (2025). Drug-supplement interaction checker. https://hellopharmacist.com/drug-supplement-interactions
- Schroeder, A. (2023). Top health aspects of lysine. Verywell Health. https://www.verywellhealth.com/how-much-lysine-to-take-for-cold-sore-8431141
- Kaiser Permanente. (2024). Arginine 25 mg/lysine 25 mg per mL intravenous solution: Drug monograph. https://healthy.kaiserpermanente.org/health-wellness/drug-encyclopedia/drug.598913
- B. Braun Medical. (2016). FreAmine® III 10 % amino acid injection: Package insert. https://imcwc.com/wp-content/uploads/2018/09/Freamine-III-10-package-insert.pdf
- LITFL. (2021). Hyperkalemia clinical case discussion. https://litfl.com/hyperkalaemia-clinical-case/
- DailyMed. (2025). Aminosyn-PF (lysine acetate, leucine, etc.) injection: Prescribing information. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=2d212e10-7e08-4aeb-b63f-dcc927897769
- Verywell Family. (2007). Are amino acids safe in pregnancy? https://www.verywellfamily.com/are-amino-acids-safe-in-pregnancy-89167
- NSW MotherSafe. (2020). Cold sores in pregnancy and breastfeeding [PDF]. https://www.seslhd.health.nsw.gov.au/sites/default/files/groups/Royal_Hospital_for_Women/Mothersafe/documents/coldsorespb20.pdf
- Humayun, M. A. et al. (2019). Comprehensive safety assessment of L-lysine supplementation. The Journal of Nutrition, 149(2), 186-197. https://doi.org/10.1093/jn/nxy231
- National Institutes of Health. (2025). Dietary Reference Intakes: Amino acids-Interactive DRI tool. https://ods.od.nih.gov/HealthInformation/nutrientrecommendations.aspx
- United States Pharmacopeia. (2023). General chapter <1150> Pharmaceutical stability. https://www.uspbpep.com/usp29/v29240/usp29nf24s0_c1150.html
- Trissel, L. A. (2024). Extended stability for parenteral drugs (8th ed.). American Society of Health-System Pharmacists. https://publications.ashp.org/downloadpdf/display/book/9781585286720/front-1.pdf
- Save Our Bones. (2019). Lysine: The essential amino acid that builds collagen. https://saveourbones.com/lysine-the-essential-amino-acid-that-builds-collagen-and-so-much-more/
- Duong, T. et al. (2018). Stability of amino acids in parenteral nutrition solutions. Nutrition, 50, 126-132. https://doi.org/10.1016/j.nut.2017.11.009
- Sparks, S. M. et al. (2022). Long-term stability of amino-acid components in TPN admixtures. American Journal of Health-System Pharmacy, 79(9), 693-702. https://publications.ashp.org/previewpdf/display/book/9781585286850/ch15.xml
- Lodi, T. (2025). Osmolality and IV infusion [PDF]. https://www.vcici.org/wp-content/uploads/2025/01/Osmolality-and-IV-Infusion-Dr.-Thomas-Lodi-MD-2025.pdf
- Kuwahara, T., Asanami, S., Tamura, T., & Kaneda, S. (1998). Effects of pH and osmolality on phlebitic potential of infusion solutions for peripheral parenteral nutrition. Journal of Toxicological Sciences, 23(1), 77-85. https://doi.org/10.2131/jts.23.77
- Martin, K. R. et al. (2019). Impact of low-protein, lysine-deficient diets on bone metabolism. Bone Reports, 11, 100237. https://doi.org/10.1016/j.bonr.2019.100237
- Drugs..com. (2025). Amino acids injection: Clinical pharmacology. https://www.drugs.com/pro/amino-acids-injection.html
- Baxter Healthcare. (2015). Primene® 10 % amino acid injection: Product monograph [PDF]. https://www.baxter.ca/sites/g/files/ebysai1431/files/2018-11/Primene_PM_2015Oct08_EN.pdf
- Saeed, A. et al. (2015). Thermal degradation kinetics of lysine hydrochloride injection solutions. Journal of Pharmaceutical Sciences, 104(3), 987-995. https://doi.org/10.1016/S1818-0876(14)00067-1
- .Vu, T. M. et al. (2022). Transport of lysine across differentiated Caco-2 cell monolayers. The Journal of Nutrition, 152(4), 1010-1017. https://doi.org/10.1093/jn/nxac267
What clinical situations justify intravenous lysine instead of oral supplements?
Parenteral lysine is favored when rapid plasma levels are required-such as renal protection during peptide radionuclide therapy-or when malabsorption, severe mucositis, or nil-per-os status preclude enteral uptake.[24]
How does lysine support bone health?
It stimulates collagen cross-linking and enhances calcium retention, processes that may strengthen cortical bone and improve fracture resistance.[25]
Is lysine stable in mixed total parenteral nutrition (TPN) bags?
Yes, but prolonged storage can degrade sulfur-containing amino acids; validated admixture studies show lysine concentration remains within 10 % of baseline for at least seven days under refrigeration.[26]
Does high-osmolar lysine require a central line?
Solutions exceeding 600 mOsm/L are best delivered via central venous access to reduce phlebitis, although peripheral infusion is possible with sufficient dilution and carrier fluids.[27]
Why must pH be considered when formulating lysine infusions?
Acidic or highly alkaline solutions irritate endothelium; adjusting admixture pH to 6-7.5 minimizes chemical phlebitis risk.[28]
Can dietary lysine deficiency impair growth?
Animal studies reveal that low-protein, lysine-deficient diets stunt skeletal growth and compromise collagen synthesis, emphasizing the amino acid’s essentiality.[29]
Is lysine compatible with lipid emulsions in TPN?
Commercial amino-acid injections containing lysine have been safely co-infused with lipids when compounded under recommended ratios, but visual inspection for creaming or coalescence is mandatory.[30]
What infusion-site precautions reduce thrombophlebitis?
Rotating peripheral lines, slowing rates, and alternating with isotonic flushes lessen endothelial irritation associated with amino-acid solutions.[31]
Does lysine interact with acid-suppressive therapy?
No clinically meaningful pharmacokinetic interactions are documented; however, comprehensive medication reviews are advised as data remain limited.[32]
How quickly does lysine reach peak plasma levels after IV start?
Peak concentrations occur within minutes of infusion initiation and decline rapidly through distribution and renal filtration, with a plasma half-life of roughly two hours in adults with normal kidney function.[33]
Administration Instructions
ODT and Troches Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Glutathione Injection
Glutathione Injection Taurine Injection
Taurine Injection Carnitine (L) Injection
Carnitine (L) Injection Glycine Injection
Glycine Injection Bi-Amino Injection
Bi-Amino Injection Ascorbic Acid (Vitamin C) Injection
Ascorbic Acid (Vitamin C) Injection Vitamin B-Complex Injection
Vitamin B-Complex Injection Magnesium Chloride Injection
Magnesium Chloride Injection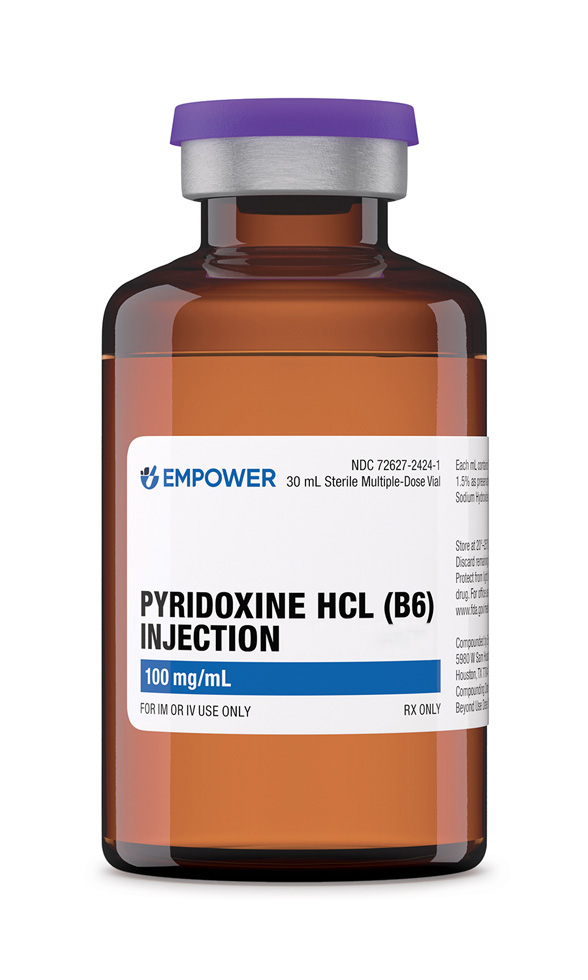 Pyridoxine HCl Injection
Pyridoxine HCl Injection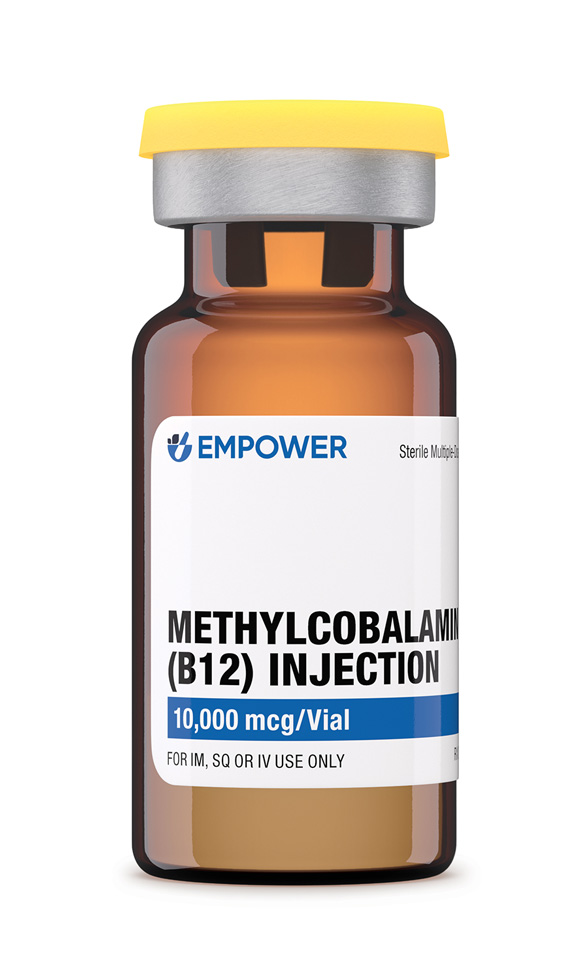 Methylcobalamin Injection (Vitamin B12)
Methylcobalamin Injection (Vitamin B12)