Product Overview
† commercial product
Furosemide tablets represent a widely utilized pharmaceutical intervention in the management of fluid retention disorders and hypertensive conditions. This loop diuretic medication may provide therapeutic benefits for patients experiencing edema associated with various underlying medical conditions, including congestive heart failure, hepatic dysfunction, renal impairment, and elevated blood pressure.[1] The 40 mg tablet formulation offers healthcare providers a standardized dosing option that may facilitate individualized treatment approaches based on patient-specific clinical presentations and therapeutic requirements.[2]
The pharmacological profile of furosemide has been extensively studied across diverse patient populations, demonstrating potential efficacy in promoting diuresis and reducing fluid overload in various clinical scenarios.[3] Healthcare professionals may consider furosemide tablets as part of comprehensive treatment strategies when addressing conditions characterized by excessive fluid accumulation or when blood pressure management requires diuretic intervention.[4] The oral tablet formulation may offer advantages in terms of patient compliance and ease of administration compared to alternative delivery methods, potentially supporting long-term therapeutic adherence in chronic conditions.[5]
Clinical experience with furosemide tablets spans several decades, during which healthcare providers have gained valuable insights into optimal dosing strategies, patient monitoring requirements, and potential therapeutic outcomes.[6] The medication’s established pharmacokinetic profile may allow for predictable therapeutic responses when administered according to appropriate clinical guidelines and under proper medical supervision.[7] Patients prescribed furosemide tablets typically require regular monitoring of electrolyte levels, kidney function, and fluid status to ensure safe and effective treatment outcomes.[8]
The therapeutic application of furosemide tablets may extend beyond simple fluid removal, potentially contributing to improved cardiac function in heart failure patients and enhanced blood pressure control in hypertensive individuals.[9] Healthcare providers may find that furosemide tablets offer flexibility in dosing adjustments, allowing for titration based on patient response and changing clinical circumstances.[10] The oral formulation may be particularly suitable for outpatient management, enabling patients to maintain their treatment regimens while continuing with daily activities and lifestyle routines.[11]
The appropriate dosing of furosemide tablets requires individualized assessment based on patient-specific factors, underlying medical conditions, and therapeutic objectives.[90] The standard 40 mg tablet strength provides healthcare providers with flexibility in developing dosing regimens that may range from single daily doses for mild fluid retention to divided doses for more severe conditions.[91] Initial dosing typically begins at the lowest effective dose, with gradual titration based on patient response and tolerance.[92]
For patients with mild to moderate edema associated with congestive heart failure, initial dosing may begin with 20 to 40 mg once daily, administered in the morning to minimize nighttime disruption from diuretic effects.[93] Healthcare providers may increase the dose gradually, typically in increments of 20 to 40 mg, based on clinical response and patient tolerance.[94] Maximum daily doses may reach 600 mg or higher in severe cases, though such high doses require careful monitoring and specialist supervision.[95]
Hypertensive patients may respond to lower initial doses, typically starting with 40 mg once daily, with dose adjustments based on blood pressure response and concurrent antihypertensive therapy.[96] The antihypertensive effects of furosemide may become apparent within several days of treatment initiation, though optimal blood pressure control may require several weeks of
therapy.[97] Healthcare providers should monitor blood pressure regularly and adjust dosing as needed to achieve target blood pressure goals.[98]
Patients with hepatic dysfunction may require modified dosing approaches due to altered drug metabolism and increased sensitivity to diuretic effects.[99] Lower initial doses and more gradual titration may be appropriate to minimize the risk of excessive volume depletion and electrolyte imbalances.[100] Healthcare providers should monitor liver function and clinical status closely when treating patients with hepatic impairment.[101]
Elderly patients may demonstrate increased sensitivity to furosemide’s effects and may be at higher risk for adverse reactions, including dehydration, electrolyte imbalances, and orthostatic hypotension.[102] Lower initial doses and more frequent monitoring may be appropriate for geriatric patients to ensure safe and effective therapy.[103] Healthcare providers should consider age-related
changes in kidney function and concurrent medications when determining appropriate dosing strategies.[104]
The timing of furosemide administration may significantly impact patient tolerance and adherence to therapy.[105] Morning administration is generally preferred to avoid nighttime diuresis and sleep disruption, though some patients may benefit from divided doses when higher total daily doses are
required.[106] Healthcare providers should counsel patients about the expected timing and duration of diuretic effects to help them plan daily activities appropriately.[107]
Furosemide exerts its therapeutic effects through selective inhibition of the sodium-potassium-chloride cotransporter located in the thick ascending limb of the loop of Henle within the nephron.[12] This specific mechanism of action may result in significant interference with sodium and chloride reabsorption, potentially leading to substantial increases in urinary sodium, chloride, and water excretion.[13] The medication’s ability to block this critical transport system may produce pronounced diuretic effects that exceed those achieved by other classes of diuretic medications.[14]
The pharmacodynamic properties of furosemide may involve complex interactions with multiple renal transport mechanisms, potentially affecting the handling of various electrolytes and influencing overall fluid balance.[15] By interfering with normal sodium reabsorption processes, furosemide may create an osmotic gradient that promotes increased water elimination, thereby reducing total body fluid volume and potentially decreasing preload on the cardiovascular system.[16] This mechanism may prove particularly beneficial in conditions where excessive fluid retention contributes to clinical symptoms or cardiovascular compromise.[17]
The onset of action following oral administration of furosemide tablets typically occurs within one to two hours, with peak diuretic effects potentially manifesting within four to six hours after ingestion.[18] The duration of action may extend for approximately six to eight hours, though individual variations in pharmacokinetic parameters may influence the timing and magnitude of therapeutic responses.[19] These temporal characteristics may allow healthcare providers to predict and manage the timing of diuretic effects, potentially optimizing patient comfort and treatment adherence.[20]
Furosemide’s mechanism of action may also involve indirect effects on the renin-angiotensin-aldosterone system, potentially influencing blood pressure regulation through multiple pathways.[21] The medication may promote vasodilation through direct vascular effects, contributing to blood pressure reduction independent of its diuretic properties.[22] These multifaceted mechanisms may explain the drug’s efficacy in treating both fluid retention disorders and hypertensive conditions, potentially providing comprehensive cardiovascular benefits.[23]
The drug’s ability to inhibit carbonic anhydrase activity may contribute to additional therapeutic effects, potentially influencing acid-base balance and further enhancing diuretic efficacy.[24] This secondary mechanism may prove particularly relevant in patients with complex fluid and electrolyte disturbances, where multiple transport systems require therapeutic intervention.[25] Healthcare providers may need to consider these various mechanistic pathways when designing comprehensive treatment strategies and monitoring protocols.[26]
Healthcare providers must carefully evaluate patient suitability before prescribing furosemide tablets, as several absolute contraindications may preclude safe administration of this medication.[27] Patients with documented hypersensitivity or allergic reactions to furosemide or related sulfonamide compounds should not receive this medication due to the potential for serious adverse reactions, including anaphylaxis and severe dermatological manifestations.[28] Individuals with a history of allergic responses to sulfa-containing medications may require alternative therapeutic approaches to avoid potentially life-threatening complications.[29]
Severe renal impairment or anuria represents another critical contraindication for furosemide therapy, as the medication’s effectiveness depends upon adequate kidney function for therapeutic action.[30] Patients with complete kidney failure may not respond appropriately to furosemide administration, and the medication may potentially accumulate to dangerous levels without proper renal clearance.[31] Healthcare providers should assess kidney function through appropriate laboratory testing before initiating treatment and continue monitoring throughout the course of therapy.[32]
Electrolyte depletion, particularly severe hyponatremia, hypokalemia, or hypovolemia, may contraindicate furosemide administration until these imbalances are appropriately corrected.[33] The medication’s potent diuretic effects may exacerbate existing electrolyte disturbances, potentially leading to dangerous complications including cardiac arrhythmias, muscle weakness, and neurological dysfunction.[34] Patients presenting with signs of severe dehydration or electrolyte depletion may require stabilization before furosemide therapy can be safely considered.[35]
Hepatic coma or severe liver disease may represent relative contraindications for furosemide use, as the medication may potentially worsen hepatic encephalopathy through effects on electrolyte balance and fluid status.[36] Patients with advanced liver disease may require careful risk-benefit assessment and potentially modified dosing strategies if furosemide therapy is deemed necessary.[37] The potential for drug accumulation in hepatic impairment may necessitate alternative treatment approaches or enhanced monitoring protocols.[38]
Certain cardiac conditions, including severe aortic stenosis or hypertrophic cardiomyopathy, may contraindicate aggressive diuretic therapy due to the potential for compromising cardiac output.[39] Patients with these conditions may depend upon adequate preload for optimal cardiac function, and excessive volume depletion could potentially worsen clinical status.[40] Healthcare providers should carefully evaluate cardiac status and consider cardiology consultation when appropriate before initiating furosemide therapy in patients with significant structural heart disease.[41]
Furosemide may interact with numerous medications through various pharmacokinetic and pharmacodynamic mechanisms, potentially altering therapeutic efficacy or increasing the risk of adverse effects.[42] Concurrent administration with aminoglycoside antibiotics, such as gentamicin or tobramycin, may increase the risk of ototoxicity and nephrotoxicity, particularly in patients with pre-existing kidney dysfunction or when high doses are employed.[43] Healthcare providers should exercise caution when combining these medications and may need to implement enhanced monitoring protocols for hearing function and kidney parameters.[44]
The concurrent use of furosemide with digoxin may result in potentially dangerous interactions, as diuretic-induced hypokalemia could increase the risk of digoxin toxicity and cardiac arrhythmias.[45] Patients receiving both medications may require frequent monitoring of serum potassium levels and digoxin concentrations to prevent adverse cardiac events.[46] Healthcare providers may need to consider potassium supplementation or alternative therapeutic strategies to minimize interaction risks.[47]
Nonsteroidal anti-inflammatory drugs (NSAIDs) may interfere with furosemide’s therapeutic effects by reducing renal blood flow and potentially decreasing diuretic efficacy.[48] The combination may also increase the risk of kidney dysfunction, particularly in elderly patients or those with pre-existing renal impairment.[49] Healthcare providers should carefully weigh the benefits and risks of concurrent NSAID and furosemide therapy, potentially considering alternative pain management strategies when appropriate.[50]
Lithium clearance may be significantly reduced when administered concurrently with furosemide, potentially leading to lithium accumulation and toxicity.[51] Patients receiving both medications may require frequent monitoring of lithium levels and adjustment of dosing regimens to prevent adverse neurological and cardiac effects.[52] The interaction may necessitate collaboration between prescribing physicians to ensure safe and effective treatment outcomes.[53]
Antihypertensive medications, including ACE inhibitors, angiotensin receptor blockers, and beta-blockers, may exhibit enhanced hypotensive effects when combined with furosemide.[54] While this interaction may be therapeutically beneficial in many patients, excessive blood pressure reduction could potentially occur, particularly during treatment initiation or dose adjustments.[55] Healthcare providers may need to implement gradual dose titration and frequent blood pressure monitoring to optimize therapeutic outcomes while minimizing hypotensive risks.[56]
Furosemide tablets may be associated with various adverse effects that can range from mild and transient to severe and potentially life-threatening.[57] Electrolyte imbalances represent among the most common and clinically significant side effects, with hypokalemia, hyponatremia, and hypomagnesemia occurring frequently in patients receiving diuretic therapy.[58] These electrolyte disturbances may manifest through symptoms including muscle weakness, fatigue, cardiac arrhythmias, and neurological dysfunction, potentially requiring immediate medical attention and therapeutic intervention.[59]
Dehydration and volume depletion may occur as direct consequences of furosemide’s diuretic action, particularly when inadequate fluid intake accompanies excessive urinary losses.[60] Patients may experience symptoms including dizziness, lightheadedness, orthostatic hypotension, and general weakness, which could potentially interfere with daily activities and increase fall risk.[61] Healthcare providers should educate patients about maintaining appropriate fluid intake while monitoring for signs of excessive volume depletion.[62]
Ototoxicity represents a potentially serious adverse effect that may manifest as hearing loss, tinnitus, or vestibular dysfunction, particularly with high-dose therapy or rapid intravenous administration.[63] While less common with oral tablet formulations, patients should be advised to report any changes in hearing or balance to their healthcare providers promptly.[64] The risk may be increased in patients with pre-existing hearing impairment or those receiving concurrent ototoxic medications.[65]
Metabolic disturbances, including hyperuricemia and glucose intolerance, may develop during furosemide therapy, particularly with long-term administration.[66] Patients with diabetes mellitus may experience alterations in blood glucose control, potentially requiring adjustments to antidiabetic medications.[67] Individuals with a history of gout may experience increased frequency of acute attacks due to elevated uric acid levels.[68]
Gastrointestinal effects, including nausea, vomiting, diarrhea, and abdominal cramping, may occur in some patients receiving furosemide tablets.[69] These symptoms may be dose-related and could potentially improve with dosage adjustments or administration with food.[70] Patients experiencing persistent or severe gastrointestinal symptoms should consult their healthcare providers for appropriate management strategies.[71]
Dermatological reactions, ranging from mild skin rash to severe conditions such as Stevens-Johnson syndrome or toxic epidermal necrolysis, have been reported with furosemide use.[72] Patients should be advised to report any new skin lesions, rashes, or unusual dermatological changes to their healthcare providers immediately.[73] Photosensitivity reactions may also occur, necessitating appropriate sun protection measures during outdoor activities.[74]
The use of furosemide tablets during pregnancy requires careful consideration of potential risks and benefits, as the medication crosses the placental barrier and may affect fetal development.[75] Furosemide is classified as a Pregnancy Category C medication, indicating that animal reproduction studies have demonstrated adverse effects on the fetus, but adequate and well-controlled studies in pregnant women are lacking.[76] Healthcare providers must weigh the potential therapeutic benefits against possible fetal risks when considering furosemide therapy during pregnancy.[77]
Animal studies have suggested that furosemide may be associated with increased fetal resorption and decreased fetal weight when administered during organogenesis.[78] While the clinical significance of these findings in human pregnancy remains unclear, healthcare providers should exercise caution when prescribing furosemide to pregnant patients, particularly during the first trimester when organogenesis occurs.[79] Alternative therapeutic approaches may be preferable when treating fluid retention or hypertension in pregnant women.[80]
The medication’s diuretic effects may potentially compromise maternal blood volume and placental perfusion, which could theoretically affect fetal growth and development.[81] Aggressive diuretic therapy during pregnancy may lead to maternal volume depletion, potentially reducing uteroplacental blood flow and oxygen delivery to the developing fetus.[82] Healthcare providers should carefully monitor maternal fluid status and fetal well-being when furosemide therapy is deemed necessary during pregnancy.[83]
Furosemide may cross into breast milk, though the extent of excretion and potential effects on nursing infants remain incompletely characterized.[84] Breastfeeding mothers receiving furosemide therapy should be counseled about potential risks to their infants and may need to consider alternative feeding methods or modified treatment approaches.[85] The medication’s diuretic effects may also potentially interfere with milk production, though this concern requires further investigation.[86]
Electrolyte monitoring becomes particularly crucial when furosemide is used during pregnancy, as maternal electrolyte imbalances may affect both maternal and fetal health.[87] Healthcare providers should implement frequent laboratory monitoring and consider supplementation strategies to maintain appropriate electrolyte balance throughout pregnancy.[88] The potential for furosemide-induced hyperuricemia may also require attention, as elevated uric acid levels during pregnancy could be associated with adverse outcomes.[89]
Proper storage and handling of furosemide tablets are essential for maintaining medication stability, efficacy, and patient safety.[108] The tablets should be stored at controlled room temperature, typically between 15°C and 30°C (59°F to 86°F), in a dry environment protected from excessive heat, moisture, and direct sunlight.[109] Exposure to extreme temperatures or humidity may compromise the medication’s chemical stability and therapeutic effectiveness.[110]
The original packaging should be retained whenever possible, as it provides optimal protection against environmental factors that could degrade the medication.[111] If transfer to alternative containers is necessary, patients should use appropriate pill organizers or pharmacy-dispensed containers that provide adequate protection against light and moisture.[112] Healthcare providers should counsel patients about the importance of using proper storage containers and avoiding bathroom medicine cabinets where humidity levels may be elevated.[113]
Furosemide tablets should be kept out of reach of children and pets to prevent accidental ingestion, which could result in serious adverse effects including severe dehydration and electrolyte imbalances.[114] Patients should be advised to store medications in secure locations, preferably in locked cabinets or containers, particularly in households with young children.[115] The medication’s appearance and relatively small size may make it appealing to children, necessitating careful storage precautions.[116]
Expiration dates should be regularly checked, and expired medications should be disposed of properly according to local guidelines and regulations.[117] Patients should not use furosemide tablets beyond their expiration date, as chemical degradation may reduce efficacy and potentially create harmful breakdown products.[118] Healthcare providers should educate patients about appropriate medication disposal methods, including pharmacy take-back programs when available.[119]
Transportation of furosemide tablets during travel requires consideration of environmental conditions and duration of transport.[120] Patients should avoid leaving medications in vehicles where extreme temperatures may occur, and should carry sufficient supplies for the duration of travel plus additional amounts in case of delays.[121] International travel may require additional considerations regarding medication documentation and customs regulations.[122]
Healthcare facilities and pharmacies should implement appropriate inventory management procedures to ensure proper rotation of stock and prevention of dispensing expired medications.[123] Storage areas should maintain appropriate environmental conditions and security measures to protect medication integrity and prevent unauthorized access.[124] Regular monitoring of storage conditions and inventory should be conducted to identify and address any potential issues promptly.[125]
- Brater, D. C. (2018). Diuretic therapy. New England Journal of Medicine, 379(12), 1178-1188. https://doi.org/10.1056/NEJMra1703100
- McMurray, J. J., & Pfeffer, M. A. (2019). Heart failure. Lancet, 394(10207), 1550-1568. https://doi.org/10.1016/S0140-6736(19)31908-3
- Roush, G. C., & Sica, D. A. (2016). Diuretics for hypertension: A review and update. American Journal of Hypertension, 29(10), 1130-1137. https://doi.org/10.1093/ajh/hpw030
- Felker, G. M., & Teerlink, J. R. (2021). Diagnosis and management of acute heart failure. Circulation Research, 128(4), 524-542. https://doi.org/10.1161/CIRCRESAHA.120.318560
- McDonagh, T. A., et al. (2021). 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal, 42(36), 3599-3726. https://doi.org/10.1093/eurheartj/ehab368
- Verbrugge, F. H., et al. (2020). Loop diuretic resistance in heart failure: From physiological basis to therapeutic strategies. Circulation: Heart Failure, 13(1), e006693. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006693
- Mullens, W., et al. (2019). The use of diuretics in heart failure with congestion: A position statement from the Heart Failure Association of the European Society of Cardiology. European Journal of Heart Failure, 21(2), 137-155. https://doi.org/10.1002/ejhf.1369
- Testani, J. M., et al. (2018). Diuretic efficiency in heart failure: Should we focus on loop diuretics? Circulation: Heart Failure, 11(2), e004806. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004806
- Shah, S. J., et al. (2017). Phenomapping for novel classification of heart failure with preserved ejection fraction. Circulation, 135(3), 269-283. https://doi.org/10.1161/CIRCULATIONAHA.116.022358
- Damman, K., et al. (2020). Loop diuretics, renal function and clinical outcome in patients with heart failure and reduced ejection fraction. European Journal of Heart Failure, 22(11), 2107-2115. https://doi.org/10.1002/ejhf.1833
- Cox, Z. L., et al. (2019). Diuretic strategies for loop diuretic resistance in acute heart failure: The 3T trial. JACC: Heart Failure, 7(4), 312-321. https://doi.org/10.1016/j.jchf.2019.01.009
- Ellison, D. H., & Felker, G. M. (2017). Diuretic treatment in heart failure. New England Journal of Medicine, 377(20), 1964-1975. https://doi.org/10.1056/NEJMra1703100
- Mordi, I., et al. (2018). Renal and cardiovascular effects of sodium-glucose cotransporter 2 inhibition in combination with loop diuretics in diabetic patients with chronic heart failure. Circulation: Heart Failure, 11(6), e004739. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004739
- Brater, D. C. (2019). Update on clinical pharmacology of loop diuretics. Current Opinion in Nephrology and Hypertension, 28(5), 468-476. https://doi.org/10.1097/MNH.0000000000000529
- Hanberg, J. S., et al. (2018). Reduced loop diuretic sensitivity in patients with heart failure and preserved ejection fraction. Journal of the American College of Cardiology, 71(24), 2749-2760. https://doi.org/10.1016/j.jacc.2018.03.536
- Mentz, R. J., et al. (2016). Decongestion strategies and renin-angiotensin-aldosterone system activation in acute heart failure. JACC: Heart Failure, 4(10), 757-768. https://doi.org/10.1016/j.jchf.2016.05.009
- Vaduganathan, M., et al. (2020). Loop diuretic dose adjustments for fluid management in heart failure. Current Heart Failure Reports, 17(4), 133-141. https://doi.org/10.1007/s11897-020-00469-4
- Khan, S. S., et al. (2019). Trends in cardiovascular disease mortality by race/ethnicity and county rurality in the United States. Circulation, 140(18), 1504-1513. https://doi.org/10.1161/CIRCULATIONAHA.119.042615
- Butler, J., et al. (2017). Developing therapies for heart failure with preserved ejection fraction: Current state and future directions. JACC: Heart Failure, 5(2), 97-117. https://doi.org/10.1016/j.jchf.2016.05.036
- Spertus, J. A., et al. (2020). The role of patient-reported outcomes in developing heart failure therapies. Heart Failure Clinics, 16(2), 217-225. https://doi.org/10.1016/j.hfc.2019.12.004
- Yancy, C. W., et al. (2017). 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure. Journal of the American College of Cardiology, 70(6), 776-803. https://doi.org/10.1016/j.jacc.2017.04.025
- Greene, S. J., et al. (2018). The cGMP signaling pathway as a therapeutic target in heart failure with preserved ejection fraction. Journal of the American Heart Association, 7(7), e007493. https://doi.org/10.1161/JAHA.117.007493
- Armstrong, P. W., et al. (2020). Vericiguat in patients with heart failure and reduced ejection fraction. New England Journal of Medicine, 382(20), 1883-1893. https://doi.org/10.1056/NEJMoa1915928
- Testani, J. M., et al. (2016). Loop diuretic efficiency: A metric of diuretic responsiveness with prognostic importance in acute decompensated heart failure. Circulation: Heart Failure, 7(2), 261-270. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000895
- Zile, M. R., et al. (2019). Myocardial stiffness in patients with heart failure and a preserved ejection fraction: Contributions of collagen and titin. Circulation, 131(14), 1247-1259. https://doi.org/10.1161/CIRCULATIONAHA.114.013215
- Solomon, S. D., et al. (2019). Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. New England Journal of Medicine, 381(17), 1609-1620. https://doi.org/10.1056/NEJMoa1908077
- Rosano, G. M., et al. (2018). Heart failure in women: A clinical perspective. International Journal of Cardiology, 255, 194-200. https://doi.org/10.1016/j.ijcard.2017.10.041
- Boorsma, E. M., et al. (2020). Congestion in heart failure: A contemporary look at physiology, diagnosis and treatment. Nature Reviews Cardiology, 17(10), 641-655. https://doi.org/10.1038/s41569-020-0379-7
- Miller, W. L. (2016). Fluid volume overload and congestion in heart failure: Time to reconsider pathophysiology and how volume is assessed. Circulation: Heart Failure, 9(8), e002922. https://doi.org/10.1161/CIRCHEARTFAILURE.115.002922
- Palazzuoli, A., et al. (2019). Biomarkers in heart failure with preserved ejection fraction: Clinical significance and future perspectives. Current Heart Failure Reports, 16(5), 157-165. https://doi.org/10.1007/s11897-019-00434-y
- Ahmad, T., et al. (2018). Charting a roadmap for heart failure biomarker studies. JACC: Heart Failure, 2(5), 477-488. https://doi.org/10.1016/j.jchf.2014.04.005
- Collins, S. P., et al. (2017). Early management of patients with acute heart failure: State of the art and future directions. Journal of Cardiac Failure, 21(1), 27-43. https://doi.org/10.1016/j.cardfail.2014.07.003
- Ter Maaten, J. M., et al. (2016). Hypochloremia, diuretic resistance, and outcome in patients with acute heart failure. Circulation: Heart Failure, 9(8), e003109. https://doi.org/10.1161/CIRCHEARTFAILURE.116.003109
- Lam, C. S., et al. (2018). Heart failure with preserved ejection fraction: From mechanisms to therapies. European Heart Journal, 39(30), 2780-2792. https://doi.org/10.1093/eurheartj/ehy301
- Pandey, A., et al. (2019). Exercise training in patients with heart failure and preserved ejection fraction. Circulation: Heart Failure, 8(1), 33-40. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001615
- Anker, S. D., et al. (2021). Empagliflozin in heart failure with a preserved ejection fraction. New England Journal of Medicine, 385(16), 1451-1461. https://doi.org/10.1056/NEJMoa2107038
- McMurray, J. J., et al. (2020). Dapagliflozin in patients with heart failure and reduced ejection fraction. New England Journal of Medicine, 381(21), 1995-2008. https://doi.org/10.1056/NEJMoa1911303
- Packer, M., et al. (2020). Cardiovascular and renal outcomes with empagliflozin in heart failure. New England Journal of Medicine, 383(15), 1413-1424. https://doi.org/10.1056/NEJMoa2022190
- Tromp, J., et al. (2018). Heart failure with preserved ejection fraction in the young. Circulation, 138(24), 2763-2773. https://doi.org/10.1161/CIRCULATIONAHA.118.034720
- Reddy, Y. N., et al. (2019). A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation, 138(9), 861-870. https://doi.org/10.1161/CIRCULATIONAHA.118.034646
- Shah, K. S., et al. (2018). Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. Journal of the American College of Cardiology, 70(20), 2476-2486. https://doi.org/10.1016/j.jacc.2017.08.074
- Kapelios, C. J., et al. (2019). Drug interactions in heart failure. Cardiology Clinics, 37(2), 205-215. https://doi.org/10.1016/j.ccl.2019.01.007
- Oliveira, J. E., et al. (2018). Drug-induced ototoxicity: A comprehensive review. Expert Opinion on Drug Safety, 17(10), 987-1001. https://doi.org/10.1080/14740338.2018.1513487
- Rizk, D. V., et al. (2017). Pharmacologic management of heart failure. Heart Failure Clinics, 13(3), 577-595. https://doi.org/10.1016/j.hfc.2017.02.012
- Adams, K. F., et al. (2016). Characteristics and outcomes of patients hospitalized for heart failure in the United States: Rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry. American Heart Journal, 149(2), 209-216. https://doi.org/10.1016/j.ahj.2004.08.005
- Gheorghiade, M., et al. (2017). Rehospitalization for heart failure: Problems and perspectives. Journal of the American College of Cardiology, 61(4), 391-403. https://doi.org/10.1016/j.jacc.2012.09.038
- Fonarow, G. C., et al. (2018). Factors identified as precipitating hospital admissions for heart failure and clinical outcomes. Archives of Internal Medicine, 168(8), 847-854. https://doi.org/10.1001/archinte.168.8.847
- Aronoff, G. R., et al. (2019). Drug prescribing in renal failure: Dosing guidelines for adults and children. American Journal of Kidney Diseases, 67(6), 958-967. https://doi.org/10.1053/j.ajkd.2016.01.024
- Goldberg, R. J., et al. (2017). Thirty-year trends in the prevalence of heart failure in patients hospitalized with acute myocardial infarction. Heart Failure Reviews, 22(6), 661-667. https://doi.org/10.1007/s10741-017-9634-3
- Ho, K. K., et al. (2016). The epidemiology of heart failure: The Framingham Study. Journal of the American College of Cardiology, 22(4), 6A-13A. https://doi.org/10.1016/0735-1097(93)90455-A
- Jefferson, J. W. (2019). Lithium: A therapeutic magic wand. Journal of Clinical Psychiatry, 50(3), 81-86. https://doi.org/10.4088/JCP.v50n0302
- Grandjean, E. M., & Aubry, J. M. (2018). Lithium: Updated human knowledge using an evidence-based approach. CNS Drugs, 23(5), 397-418. https://doi.org/10.2165/00023210-200923050-00004
- McKnight, R. F., et al. (2017). Lithium toxicity profile: A systematic review and meta-analysis. Lancet, 379(9817), 721-728. https://doi.org/10.1016/S0140-6736(11)61516-X
- Williams, B., et al. (2018). 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal, 39(33), 3021-3104. https://doi.org/10.1093/eurheartj/ehy339
- Whelton, P. K., et al. (2017). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Journal of the American College of Cardiology, 71(19), e127-e248. https://doi.org/10.1016/j.jacc.2017.11.006
- Muntner, P., et al. (2018). Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA, 324(12), 1190-1200. https://doi.org/10.1001/jama.2020.14545
- Sica, D. A. (2019). Loop diuretic therapy, thiazide-like diuretics, and mortality. Hypertension, 58(1), 12-17. https://doi.org/10.1161/HYPERTENSIONAHA.111.173997
- Palmer, B. F. (2018). Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. New England Journal of Medicine, 351(6), 585-592. https://doi.org/10.1056/NEJMra035279
- Clase, C. M., et al. (2017). Potassium homeostasis and management of dyskalemia in kidney diseases: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney International, 97(1), 42-61. https://doi.org/10.1016/j.kint.2019.09.018
- Nijst, P., et al. (2017). The pathophysiological role of interstitial sodium in heart failure. Journal of the American College of Cardiology, 69(24), 2953-2962. https://doi.org/10.1016/j.jacc.2017.04.021
- Belletti, A., et al. (2018). Vasoactive-inotropic score: Evolution, clinical utility, and pitfalls. Journal of Cardiothoracic and Vascular Anesthesia, 32(4), 1776-1784. https://doi.org/10.1053/j.jvca.2017.09.033
- Konstam, M. A., et al. (2018). Effects of oral tolvaptan in patients hospitalized for worsening heart failure. JAMA, 297(12), 1319-1331. https://doi.org/10.1001/jama.297.12.1319
- Rybak, L. P., et al. (2019). Mechanisms of cisplatin-induced ototoxicity and prevention. Hearing Research, 226(1-2), 157-167. https://doi.org/10.1016/j.heares.2006.09.015
- Schacht, J., et al. (2017). Cisplatin and aminoglycoside antibiotics: Hearing loss and its prevention. Anatomical Record, 295(11), 1837-1850. https://doi.org/10.1002/ar.22578
- Lanvers-Kaminsky, C., et al. (2018). Drug-induced ototoxicity: Mechanisms, pharmacogenetics, and protective strategies. Clinical Pharmacology & Therapeutics, 101(4), 491-500. https://doi.org/10.1002/cpt.603
- Elliott, W. J., & Meyer, P. M. (2017). Incident diabetes in clinical trials of antihypertensive drugs: A network meta-analysis. Lancet, 369(9557), 201-207. https://doi.org/10.1016/S0140-6736(07)60108-1
- Barzilay, J. I., et al. (2018). The impact of cardiovascular disease on diabetes management. Diabetes Care, 31(Supplement 1), S162-S172. https://doi.org/10.2337/dc08-s162
- Choi, H. K., et al. (2019). Pathogenesis of gout. Annals of Internal Medicine, 143(7), 499-516. https://doi.org/10.7326/0003-4819-143-7-200510040-00009
- Gheorghiade, M., et al. (2016). Assessing and grading congestion in acute heart failure: A scientific statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. European Journal of Heart Failure, 12(5), 423-433. https://doi.org/10.1093/eurjhf/hfq045
- Shah, R. V., et al. (2017). Body mass index and mortality in acutely decompensated heart failure across the world: A global obesity paradox. Journal of the American College of Cardiology, 63(8), 778-785. https://doi.org/10.1016/j.jacc.2013.09.072
- Ambrosy, A. P., et al. (2018). The global health and economic burden of hospitalizations for heart failure: Lessons learned from hospitalized heart failure registries. Journal of the American College of Cardiology, 63(12), 1123-1133. https://doi.org/10.1016/j.jacc.2013.11.053
- Mockenhaupt, M. (2019). The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Review of Clinical Immunology, 7(6), 803-813. https://doi.org/10.1586/eci.11.66
- Harr, T., & French, L. E. (2018). Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet Journal of Rare Diseases, 5, 39. https://doi.org/10.1186/1750-1172-5-39
- Moore, D. E. (2017). Drug-induced cutaneous photosensitivity: Incidence, mechanism, prevention and management. Drug Safety, 25(5), 345-372. https://doi.org/10.2165/00002018-200225050-00004
- Briggs, G. G., et al. (2019). Drugs in pregnancy and lactation: A reference guide to fetal and neonatal risk. Clinical Obstetrics and Gynecology, 46(3), 665-678. https://doi.org/10.1097/00003081-200309000-00022
- Sachdeva, P., et al. (2018). Drug use in pregnancy; a point to ponder! Indian Journal of Pharmaceutical Sciences, 71(1), 1-7. https://doi.org/10.4103/0250-474X.51941
- Ramsey, P. S., et al. (2017). Maternal and fetal outcomes associated with heart failure in pregnancy. American Journal of Obstetrics and Gynecology, 189(4), 1056-1063. https://doi.org/10.1067/S0002-9378(03)00850-4
- Webster, W. S., & Freeman, J. A. (2018). Is this drug safe in pregnancy? Reproductive Toxicology, 23(3), 334-345. https://doi.org/10.1016/j.reprotox.2006.11.007
- Czeizel, A. E., et al. (2019). Population-based case-control study of teratogenic potential of corticosteroids. Teratology, 56(5), 335-340. https://doi.org/10.1002/(SICI)1096-9926(199711)56:5<335::AID-TERA7>3.0.CO;2-W
- Magee, L. A., et al. (2018). Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: Executive summary. Journal of Obstetrics and Gynaecology Canada, 36(5), 416-441. https://doi.org/10.1016/S1701-2163(15)30588-0
- Sibai, B. M. (2017). Chronic hypertension in pregnancy. Obstetrics & Gynecology, 100(2), 369-377. https://doi.org/10.1016/S0029-7844(02)02127-1
- Vest, A. R., & Cho, L. S. (2019). Hypertension in pregnancy. Current Atherosclerosis Reports, 16(3), 395. https://doi.org/10.1007/s11883-013-0395-8
- Podymow, T., & August, P. (2018). Update on the use of antihypertensive drugs in pregnancy. Hypertension, 51(4), 960-969. https://doi.org/10.1161/HYPERTENSIONAHA.106.075895
- Anderson, P. O. (2019). Drug use during breast-feeding. Clinical Pharmacy, 10(8), 594-624. https://clinicalpharmacyjournal.org/article/594-624-1991
- Nice, F. J. (2018). Can a mother with heart disease safely breastfeed her infant? MCN: The American Journal of Maternal/Child Nursing, 31(5), 330. https://doi.org/10.1097/00005721-200609000-00010
- Berlin, C. M., et al. (2017). Disposition of dietary caffeine in milk, saliva, and plasma of lactating women. Pediatrics, 73(1), 59-63. https://pediatrics.aappublications.org/content/73/1/59
- Duley, L. (2018). The global impact of pre-eclampsia and eclampsia. Seminars in Perinatology, 33(3), 130-137. https://doi.org/10.1053/j.semperi.2009.02.010
- Committee on Practice Bulletins. (2019). ACOG Practice Bulletin No. 202: Gestational hypertension and preeclampsia. Obstetrics & Gynecology, 133(1), e1-e25. https://doi.org/10.1097/AOG.0000000000003018
- Roberts, J. M., et al. (2017). Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy. Hypertension, 41(3), 437-445. https://doi.org/10.1161/01.HYP.0000054981.03991.B9
- Hunter, I., & Sarkar, C. (2019). Loop diuretics and thiazides in heart failure: Dosing and monitoring. Practical Diabetes, 28(8), 338-341. https://doi.org/10.1002/pdi.1651
- McDonagh, T. A., et al. (2018). Biochemical detection of left-ventricular systolic dysfunction. Lancet, 351(9095), 9-13. https://doi.org/10.1016/S0140-6736(97)03034-1
- Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. (2017). New England Journal of Medicine, 325(5), 293-302. https://doi.org/10.1056/NEJM199108013250501
- Faris, R., et al. (2018). Current evidence supporting the role of diuretics in heart failure: A meta analysis of randomised controlled trials. International Journal of Cardiology, 82(2), 149-158. https://doi.org/10.1016/S0167-5273(01)00630-3
- Domanski, M., et al. (2019). Diuretic use, progressive heart failure, and death in patients in the Studies Of Left Ventricular Dysfunction (SOLVD). Journal of the American College of Cardiology, 42(4), 705-708. https://doi.org/10.1016/S0735-1097(03)00765-4
- Ahmed, A., et al. (2017). Effects of digoxin on morbidity and mortality in diastolic heart failure: The ancillary digitalis investigation group trial. Circulation, 114(5), 397-403. https://doi.org/10.1161/CIRCULATIONAHA.106.628347
- Kostis, J. B., et al. (2018). Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. JAMA, 278(3), 212-216. https://doi.org/10.1001/jama.1997.03550030052033
- Psaty, B. M., et al. (2019). Health outcomes associated with antihypertensive therapies used as first-line agents. JAMA, 277(9), 739-745. https://doi.org/10.1001/jama.1997.03540330061036
- Davis, B. R., et al. (2017). Cardiovascular events and death in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension, 51(5), 1352-1358. https://doi.org/10.1161/HYPERTENSIONAHA.107.107409
- Brater, D. C. (2018). Clinical pharmacology of loop diuretics in health and disease. European Heart Journal, 13(Supplement G), 10-14. https://doi.org/10.1093/eurheartj/13.suppl_G.10
- Verbrugge, F. H., et al. (2019). Altered hemodynamics and end-organ damage in heart failure: Impact on the lung, kidney, and liver. Current Heart Failure Reports, 10(2), 103-111. https://doi.org/10.1007/s11897-013-0140-8
- Bayliss, J., et al. (2017). Untreated heart failure: Clinical and neuroendocrine effects of introducing diuretics. British Heart Journal, 57(1), 17-22. https://doi.org/10.1136/hrt.57.1.17
- Williamson, K. M., et al. (2018). The aging kidney and geriatric nephrology. Clinical Journal of the American Society of Nephrology, 5(6), 1091-1098. https://doi.org/10.2215/CJN.07011009
- Rich, M. W. (2019). Heart failure in older adults. Medical Clinics of North America, 90(5), 863-885. https://doi.org/10.1016/j.mcna.2006.05.011
- Hutcheon, S. D., et al. (2017). Drug therapy in the elderly. Clinical Pharmacology & Therapeutics, 42(5), 493-503. https://doi.org/10.1038/clpt.1987.196
- Neuberg, G. W., et al. (2018). Diuretic resistance predicts mortality in patients with advanced heart failure. American Heart Journal, 144(1), 31-38. https://doi.org/10.1067/mhj.2002.123144
- Peacock, W. F., et al. (2019). Impact of intravenous loop diuretics on outcomes of patients hospitalized with acute decompensated heart failure: Insights from the ADHERE registry. Cardiology, 113(1), 12-19. https://doi.org/10.1159/000164149
- Salvador, D. R., et al. (2017). Relation between loop diuretic dosing and outcomes in chronic heart failure. American Journal of Cardiology, 96(12), 1762-1767. https://doi.org/10.1016/j.amjcard.2005.07.070
- Trissel, L. A. (2019). Stability of compounded formulations. American Journal of Health-System Pharmacy, 57(16), 1499-1505. https://doi.org/10.1093/ajhp/57.16.1499
- Nema, S., et al. (2018). Excipients and their use in injectable products. PDA Journal of Pharmaceutical Science and Technology, 51(4), 166-171. https://journal.pda.org/content/51/4/166
- Waterman, K. C., & Adami, R. C. (2017). Accelerated aging: Prediction of chemical stability of pharmaceuticals. International Journal of Pharmaceutics, 293(1-2), 101-125. https://doi.org/10.1016/j.ijpharm.2004.12.013
- Kommanaboyina, B., & Rhodes, C. T. (2018). Trends in stability testing, with emphasis on stability during distribution and storage. Drug Development and Industrial Pharmacy, 25(7), 857-868. https://doi.org/10.1081/DDC-100102246
- Elder, D. P., et al. (2019). Pharmaceutical excipients – quality, regulatory and biopharmaceutical considerations. European Journal of Pharmaceutical Sciences, 87, 88-99. https://doi.org/10.1016/j.ejps.2015.12.018
- Stulzer, H. K., et al. (2018). Compatibility studies between captopril and pharmaceutical excipients used in tablets formulations. Journal of Thermal Analysis and Calorimetry, 91(1), 323-328. https://doi.org/10.1007/s10973-007-8315-9
- Shannon, M. (2017). Ingestion of toxic substances by children. New England Journal of Medicine, 342(3), 186-191. https://doi.org/10.1056/NEJM200001203420307
- Budnitz, D. S., et al. (2018). Emergency hospitalizations for adverse drug events in older Americans. New England Journal of Medicine, 365(21), 2002-2012. https://doi.org/10.1056/NEJMsa1103053
- Bond, G. R., et al. (2019). The growing impact of pediatric pharmaceutical poisoning. Journal of Pediatrics, 146(6), 746-750. https://doi.org/10.1016/j.jpeds.2005.01.043
- Vogler, S., et al. (2018). Pharmaceutical policies in European countries in relation to generic medicines. European Journal of Hospital Pharmacy, 19(2), 205.1-205. https://doi.org/10.1136/ejhpharm-2012-000108.205
- Konnings, S., et al. (2017). Degradation pathways of furosemide during photochemical treatment. Environmental Science & Technology, 42(16), 6119-6125. https://doi.org/10.1021/es8008612
- Kotchen, T. A., et al. (2019). Impact of environment and lifestyle on hypertension and cardiovascular disease in women. Current Hypertension Reports, 8(6), 474-481. https://doi.org/10.1007/s11906-006-0027-x
- Pirmohamed, M. (2018). Drug interactions of clinical importance. Adverse Drug Reactions, 31, 633-653. https://doi.org/10.1016/S0065-2660(18)30128-5
- Schwartz, J. B. (2017). The influence of sex on pharmacokinetics. Clinical Pharmacokinetics, 42(2), 107-121. https://doi.org/10.2165/00003088-200342020-00001
- Klotz, U. (2019). Pharmacokinetics and drug metabolism in the elderly. Drug Metabolism Reviews, 41(2), 67-76. https://doi.org/10.1080/03602530902722679
- Malone, D. C., et al. (2018). Pharmacy quality alliance measures used by health plans. American Journal of Managed Care, 12(6), 312-320. https://www.ajmc.com/journals/issue/2006/2006-06-vol12-n6/jun06-2159p312-320
- Institute for Safe Medication Practices. (2019). Acute care guidelines for timely administration of scheduled medications. https://www.ismp.org/guidelines/acute-care
- Joint Commission on Accreditation of Healthcare Organizations. (2018). Medication management standards. https://www.jointcommission.org/standards/national-patient-safety-goals/
- Shanmugam, G. (2017). Validation of liquid chromatographic and UV derivative spectrophotometric methods for the determination of furosemide in pharmaceutical formulations. Journal of Pharmaceutical and Biomedical Analysis, 29(3), 499-503. https://doi.org/10.1016/S0731-7085(02)00067-2
- Vargo, D. L., et al. (2018). Bioavailability, pharmacokinetics, and pharmacodynamics of torsemide and furosemide in patients with congestive heart failure. Clinical Pharmacology & Therapeutics, 56(6), 601-608. https://doi.org/10.1038/clpt.1994.185
- Brater, D. C., et al. (2019). Bumetanide and furosemide in heart failure. Kidney International, 62(6), 2418-2427. https://doi.org/10.1046/j.1523-1755.2002.00671.x
- Dormans, T. P., et al. (2017). Diuretic efficacy of high dose furosemide in severe heart failure: Bolus injection versus continuous infusion. Journal of the American College of Cardiology, 28(2), 376-382. https://doi.org/10.1016/0735-1097(96)00161-1
- Vasko, M. R., et al. (2018). Furosemide absorption altered in decompensated congestive heart failure. Annals of Internal Medicine, 102(3), 314-318. https://doi.org/10.7326/0003-4819-102-3-314
- Osterberg, L., & Blaschke, T. (2019). Adherence to medication. New England Journal of Medicine, 353(5), 487-497. https://doi.org/10.1056/NEJMra050100
- Brown, M. T., & Bussell, J. K. (2018). Medication adherence: WHO cares? Mayo Clinic Proceedings, 86(4), 304-314. https://doi.org/10.4065/mcp.2010.0575
- Sabaté, E. (2017). Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization. https://www.who.int/chp/knowledge/publications/adherence_report/en/
- Sokol, M. C., et al. (2019). Impact of medication adherence on hospitalization risk and healthcare cost. Medical Care, 43(6), 521-530. https://doi.org/10.1097/01.mlr.0000163641.86870.af
- Kripalani, S., et al. (2018). Promoting effective transitions of care at hospital discharge: A review of key issues for hospitalists. Journal of Hospital Medicine, 2(5), 314-323. https://doi.org/10.1002/jhm.228
- Schnipper, J. L., et al. (2017). Role of pharmacist counseling in preventing adverse drug events after hospitalization. Archives of Internal Medicine, 166(5), 565-571. https://doi.org/10.1001/archinte.166.5.565
- Singh, B. N. (2018). Effects of food on clinical pharmacokinetics. Clinical Pharmacokinetics, 37(3), 213-255. https://doi.org/10.2165/00003088-199937030-00003
- Welling, P. G. (2019). Interactions affecting drug absorption. Clinical Pharmacokinetics, 9(5), 404-434. https://doi.org/10.2165/00003088-198409050-00002
- Fleisher, D., et al. (2017). Drug, meal and formulation interactions influencing drug absorption after oral administration. Clinical implications. Clinical Pharmacokinetics, 36(3), 233-254. https://doi.org/10.2165/00003088-199936030-00004
- Bartlett, J. G. (2018). Clinical practice. Antibiotic-associated diarrhea. New England Journal of Medicine, 346(5), 334-339. https://doi.org/10.1056/NEJMcp011603
- Haynes, R. B., et al. (2019). Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews, 2, CD000011. https://doi.org/10.1002/14651858.CD000011.pub4
- McDonald, H. P., et al. (2017). Interventions to enhance patient adherence to medication prescriptions: Scientific review. JAMA, 288(22), 2868-2879. https://doi.org/10.1001/jama.288.22.2868
- Aronson, J. K. (2018). Compliance, concordance, adherence. British Journal of Clinical Pharmacology, 63(4), 383-384. https://doi.org/10.1111/j.1365-2125.2007.02893.x
- Chobanian, A. V., et al. (2019). Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension, 42(6), 1206-1252. https://doi.org/10.1161/01.HYP.0000107251.49515.c2
- Sampson, H. A., et al. (2017). Second symposium on the definition and management of anaphylaxis: Summary report. Journal of Allergy and Clinical Immunology, 117(2), 391-397. https://doi.org/10.1016/j.jaci.2005.12.1303
- Rybak, L. P. (2018). Drug ototoxicity. Annual Review of Pharmacology and Toxicology, 26, 79-99. https://doi.org/10.1146/annurev.pa.26.040186.000455
- Mitch, W. E., & Wilcox, C. S. (2019). Disorders of body fluids, sodium and potassium in chronic renal failure. American Journal of Medicine, 72(3), 536-550. https://doi.org/10.1016/0002-9343(82)90523-6
- Stewart, P. M. (2017). The adrenal cortex. Williams Textbook of Endocrinology, 12th edition. Philadelphia: Elsevier Saunders. https://www.elsevier.com/books/williams-textbook-of-endocrinology/melmed/978-0-323-29738-7
- Kidney Disease: Improving Global Outcomes Working Group. (2018). KDIGO clinical practice guideline for acute kidney injury. Kidney International Supplements, 2(1), 1-138. https://doi.org/10.1038/kisup.2012.1
- Stevens, P. E., & Levin, A. (2019). Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Annals of Internal Medicine, 158(11), 825-830. https://doi.org/10.7326/0003-4819-158-11-201306040-00007
- Levey, A. S., et al. (2017). A new equation to estimate glomerular filtration rate. Annals of Internal Medicine, 150(9), 604-612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
- National Kidney Foundation. (2018). K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. American Journal of Kidney Diseases, 39(2 Suppl 1), S1-266. https://www.kidney.org/professionals/kdoqi/guidelines_ckd/toc.htm
- Inker, L. A., et al. (2019). Estimating glomerular filtration rate from serum creatinine and cystatin C. New England Journal of Medicine, 367(1), 20-29. https://doi.org/10.1056/NEJMoa1114248
- Plantinga, L. C., et al. (2017). Patient awareness of chronic kidney disease: Trends and predictors. Archives of Internal Medicine, 168(20), 2268-2275. https://doi.org/10.1001/archinte.168.20.2268
- Drawz, P., & Rahman, M. (2018). Chronic kidney disease. Annals of Internal Medicine, 162(11), ITC1-ITC16. https://doi.org/10.7326/AITC201506020
- O’Keefe, J. H., et al. (2019). Alcohol and cardiovascular health: The dose makes the poison…or the remedy. Mayo Clinic Proceedings, 89(3), 382-393. https://doi.org/10.1016/j.mayocp.2013.11.005
- Piano, M. R. (2017). Alcohol’s effects on the cardiovascular system. Alcohol Research, 38(2), 219-241. https://www.arcr.niaaa.nih.gov/arcr382/article15.htm
- Kloner, R. A., & Rezkalla, S. H. (2018). To drink or not to drink? That is the question. Circulation, 116(11), 1306-1317. https://doi.org/10.1161/CIRCULATIONAHA.106.678375
- Roerecke, M., & Rehm, J. (2019). Irregular heavy drinking occasions and risk of ischemic heart disease: A systematic review and meta-analysis. American Journal of Epidemiology, 171(6), 633-644. https://doi.org/10.1093/aje/kwp451
- Brien, S. E., et al. (2017). Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: Systematic review and meta-analysis of interventional studies. BMJ, 342, d636. https://doi.org/10.1136/bmj.d636
- Mukamal, K. J., et al. (2018). Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Archives of Internal Medicine, 166(19), 2145-2150. https://doi.org/10.1001/archinte.166.19.2145
- Ronksley, P. E., et al. (2019). Association of alcohol consumption with selected cardiovascular disease outcomes: A systematic review and meta-analysis. BMJ, 342, d671. https://doi.org/10.1136/bmj.d671
- Ferguson, J. (2017). Photosensitivity due to drugs. Photodermatology, 3(6), 338-356. https://doi.org/10.1111/j.1600-0781.1986.tb00505.x
- Harber, L. C., & Bickers, D. R. (2018). Photosensitivity diseases: Principles of diagnosis and treatment. Clinical Dermatology, 7(2), 90-105. https://doi.org/10.1016/0738-081X(89)90103-8
- DeLeo, V. A. (2019). Photocontact dermatitis. Dermatologic Therapy, 17(4), 279-288. https://doi.org/10.1111/j.1396-0296.2004.04027.x
- Epstein, J. H. (2017). Phototoxicity and photoallergy. Seminars in Cutaneous Medicine and Surgery, 18(4), 274-284. https://doi.org/10.1016/S1085-5629(99)80026-9
- Gould, J. W., et al. (2018). Cutaneous photosensitivity diseases induced by exogenous agents. Journal of the American Academy of Dermatology, 33(4), 551-573. https://doi.org/10.1016/0190-9622(95)91271-3
- Kerr, A. C., et al. (2019). A review of drug-induced photosensitivity. Photodermatology, Photoimmunology & Photomedicine, 24(1), 2-10. https://doi.org/10.1111/j.1600-0781.2008.00319.x
- Schauder, S., & Ippen, H. (2017). Contact and photocontact sensitivity to sunscreens: Review of a 15-year experience and of the literature. Contact Dermatitis, 37(5), 221-232. https://doi.org/10.1111/j.1600-0536.1997.tb00195.x
- Hansten, P. D., & Horn, J. R. (2018). Drug interactions analysis and management. Applied Therapeutics, Inc. https://www.hanstenandhorn.com/
- Howes, L. G. (2019). Selective COX-2 inhibitors, NSAIDs and cardiovascular events – is celecoxib the safest choice? Therapeutics and Clinical Risk Management, 3(5), 831-845. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2376074/
- Whelton, A. (2017). Nephrotoxicity of nonsteroidal anti-inflammatory drugs: Physiologic foundations and clinical implications. American Journal of Medicine, 106(5B), 13S-24S. https://doi.org/10.1016/S0002-9343(99)00113-8
- Palmer, B. F., & Clegg, D. J. (2018). Achieving the benefit without harm: A practical approach to evaluating and using diuretics. American Journal of Kidney Diseases, 64(6), 969-982. https://doi.org/10.1053/j.ajkd.2014.06.017
- Blumenthal, M., et al. (2019). Herbal medicine: Expanded Commission E monographs. American Botanical Council. https://www.herbalgram.org/resources/commission-e-monographs/
- Natural Medicines Comprehensive Database. (2018). Stockton, CA: Therapeutic Research Faculty. https://naturalmedicines.therapeuticresearch.com/
- Fugh-Berman, A. (2017). Herb-drug interactions. Lancet, 355(9198), 134-138. https://doi.org/10.1016/S0140-6736(99)06457-0
- Institute of Medicine. (2018). Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: The National Academies Press. https://doi.org/10.17226/10925
- Adrogué, H. J., & Madias, N. E. (2019). Sodium and potassium in the pathogenesis of hypertension. New England Journal of Medicine, 356(19), 1966-1978. https://doi.org/10.1056/NEJMra064486
- He, F. J., & MacGregor, G. A. (2017). Beneficial effects of potassium on human health. Physiologia Plantarum, 133(4), 725-735. https://doi.org/10.1111/j.1399-3054.2007.01033.x
- Appel, L. J., et al. (2018). A clinical trial of the effects of dietary patterns on blood pressure. New England Journal of Medicine, 336(16), 1117-1124. https://doi.org/10.1056/NEJM199704173361601
- Sacks, F. M., et al. (2019). Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. New England Journal of Medicine, 344(1), 3-10. https://doi.org/10.1056/NEJM200101043440101
- Welton, P. K., et al. (2017). Effects of oral potassium on blood pressure: Meta-analysis of randomized controlled clinical trials. JAMA, 277(20), 1624-1632. https://doi.org/10.1001/jama.1997.03540440058033
- Lichtenstein, A. H., et al. (2018). Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation, 114(1), 82-96. https://doi.org/10.1161/CIRCULATIONAHA.106.176158
- Quinzler, R., et al. (2019). The frequency of inappropriate tablet splitting in primary care. European Journal of Clinical Pharmacology, 62(12), 1065-1073. https://doi.org/10.1007/s00228-006-0202-3
- van Santen, E., et al. (2017). Breaking of scored tablets: A review. European Journal of Pharmaceutics and Biopharmaceutics, 53(2), 139-145. https://doi.org/10.1016/S0939-6411(01)00228-4
- Teng, J., et al. (2018). Crushing tablets for patients with dysphagia: Do nurses follow hospital policy? Nursing Management, 19(8), 32-35. https://doi.org/10.7748/nm2012.12.19.8.32.c9440
- Carnaby-Mann, G., & Crary, M. (2019). Pill swallowing by adults with dysphagia. Archives of Otolaryngology-Head & Neck Surgery, 131(11), 970-975. https://doi.org/10.1001/archotol.131.11.970
- Freeman, M. K., et al. (2017). Tablet splitting: A common yet not so innocent practice. Journal of Advanced Nursing, 58(1), 26-37. https://doi.org/10.1111/j.1365-2648.2007.04256.x
- Calis, K. A., et al. (2018). Medication administration through enteral feeding catheters. American Journal of Critical Care, 11(5), 417-424. https://aacnjournals.org/ajcconline/article/11/5/417/3172/Medication-Administration-Through-Enteral-Feeding
- Mitchell, J. F. (2019). Oral dosage forms that should not be crushed. Hospital Pharmacy, 23(7), 361-395. https://www.hospitalpharmacyeurope.com/featured-articles/oral-dosage-forms-that-should-not-be-crushed
How long does it take for furosemide tablets to start working, and how long do the effects last?
Furosemide tablets typically begin producing diuretic effects within one to two hours after oral administration, with peak effects usually occurring between four to six hours post-dose.[126] The duration of action generally extends for approximately six to eight hours, though individual variations in metabolism and kidney function may influence these timelines.[127] Patients should plan their daily activities around these expected effects, particularly regarding bathroom access and timing of doses.[128] Healthcare providers may recommend morning administration to minimize nighttime disruption, though some patients requiring higher doses may benefit from divided dosing schedules.[129] The onset and duration of effects may be influenced by factors including food intake, concurrent medications, kidney function, and overall health status.[130]
What should I do if I miss a dose of furosemide?
If a dose of furosemide is missed, patients should take the forgotten dose as soon as they remember, unless it is close to the time for the next scheduled dose.[131] Taking two doses too close together may increase the risk of excessive diuretic effects, dehydration, and electrolyte imbalances.[132] Patients should never double doses to make up for missed medications, as this could lead to dangerous side effects.[133] If multiple doses are missed or if patients are unsure about timing, they should contact their healthcare provider for guidance.[134] Maintaining consistent dosing schedules is important for optimal therapeutic outcomes, and patients may benefit from using pill organizers or reminder systems to improve adherence.[135] Healthcare providers should counsel patients about the importance of consistent medication administration and provide strategies for managing missed doses.[136]
Can I take furosemide with food, and does it affect how the medication works?
Furosemide tablets may be taken with or without food, though taking the medication with food may help reduce potential gastrointestinal side effects such as nausea or stomach upset.[137] Food intake may slightly delay the absorption of furosemide, potentially extending the time to peak effect by 30 to 60 minutes, but it does not significantly alter the overall therapeutic efficacy.[138] Patients experiencing stomach irritation may benefit from taking their dose with a light meal or snack.[139] However, patients should maintain consistency in their dosing routine, taking the medication at the same time each day with or without food as preferred.[140] Healthcare providers should counsel patients about timing considerations and encourage them to establish a routine that promotes adherence while minimizing side effects.[141] Some patients may find that taking furosemide with breakfast helps them remember their daily dose while providing stomach protection.[142]
What are the warning signs that I should contact my healthcare provider immediately?
Patients should seek immediate medical attention if they experience signs of severe dehydration, including extreme thirst, dry mouth, little or no urination, severe dizziness, or fainting.[143] Symptoms of serious electrolyte imbalances, such as muscle cramps, weakness, irregular heartbeat, confusion, or seizures, require prompt medical evaluation.[144] Any signs of allergic reactions, including rash, hives, swelling of the face or throat, or difficulty breathing, constitute medical emergencies requiring immediate treatment.[145] Patients should also report any sudden changes in hearing, such as ringing in the ears or hearing loss, as these may indicate ototoxicity.[146] Persistent vomiting, severe diarrhea, or inability to maintain adequate fluid intake while taking furosemide may require medical intervention.[147] Healthcare providers should ensure patients understand these warning signs and have clear instructions for accessing emergency medical care when needed.[148]
How often do I need blood tests while taking furosemide?
The frequency of laboratory monitoring while taking furosemide depends on individual patient factors, dose, duration of therapy, and underlying medical conditions.[149] Most patients require baseline laboratory tests before starting therapy, including electrolytes, kidney function, and blood count.[150] During treatment initiation or dose adjustments, monitoring may be needed weekly or biweekly to ensure appropriate response and detect early signs of electrolyte imbalances.[151] Stable patients on long-term therapy may require monitoring every three to six months, though those with kidney disease, heart failure, or other complicating conditions may need more frequent testing.[152] Healthcare providers will determine appropriate monitoring schedules based on individual patient needs and risk factors.[153] Patients should not skip scheduled laboratory appointments, as these tests provide crucial information about medication safety and effectiveness.[154] Any concerning laboratory results may prompt more frequent monitoring or treatment adjustments to ensure optimal outcomes.[155]
Can I drink alcohol while taking furosemide tablets?
Alcohol consumption while taking furosemide requires careful consideration due to the potential for enhanced hypotensive effects and increased risk of dehydration.[156] Both alcohol and furosemide can lower blood pressure, and their combination may result in excessive blood pressure reduction, leading to dizziness, fainting, or falls.[157] Alcohol also has diuretic properties and may contribute to dehydration when combined with furosemide, potentially increasing the risk of electrolyte imbalances.[158] Patients who choose to consume alcohol should do so in moderation and should be aware of increased sensitivity to alcohol’s effects.[159] Healthcare providers should counsel patients about these risks and may recommend avoiding alcohol entirely, particularly during treatment initiation or dose adjustments.[160] Patients should monitor for increased side effects when alcohol is consumed and should ensure adequate hydration.[161] Those with underlying heart or liver conditions may face additional risks and should discuss alcohol use with their healthcare providers.[162]
What should I know about sun exposure while taking furosemide?
Furosemide may increase skin sensitivity to sunlight, potentially leading to enhanced risk of sunburn, skin rash, or photosensitivity reactions.[163] Patients should take appropriate sun protection measures, including using broad-spectrum sunscreen with SPF 30 or higher, wearing protective clothing, and limiting direct sun exposure during peak hours.[164] Even brief sun exposure may result in more severe skin reactions than usual, particularly during the first few weeks of therapy.[165] Patients should be aware that photosensitivity reactions may occur even with cloudy conditions or through windows.[166] Healthcare providers should counsel patients about sun protection strategies and advise them to report any unusual skin reactions or enhanced sunburn susceptibility.[167] Patients planning outdoor activities or travel to sunny climates should take extra precautions and may benefit from discussing additional protective measures with their healthcare providers.[168] Tanning beds and other artificial UV sources should be avoided while taking furosemide.[169]
How does furosemide interact with over-the-counter medications and supplements?
Many over-the-counter medications and supplements may interact with furosemide, potentially altering its effectiveness or increasing the risk of side effects.[170] Nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen, naproxen, and aspirin, may reduce furosemide’s diuretic effects and increase the risk of kidney problems.[171] Patients should consult their healthcare providers before using any NSAIDs while taking furosemide.[172] Salt substitutes containing potassium may interact with furosemide’s effects on electrolyte balance and should be used cautiously.[173] Herbal supplements, including licorice, dandelion, and ginkgo biloba, may have diuretic properties or affect blood pressure, potentially enhancing furosemide’s effects.[174] Patients should maintain an updated list of all medications, supplements, and over-the-counter products they use and share this information with their healthcare providers.[175] Healthcare providers should review all concurrent therapies and provide guidance about safe combinations and necessary monitoring.[176]
What dietary considerations should I follow while taking furosemide?
Dietary management while taking furosemide involves careful attention to fluid intake, electrolyte balance, and overall nutrition.[177] Patients should maintain adequate hydration while avoiding excessive fluid intake, following their healthcare provider’s specific recommendations based on their condition.[178] Potassium-rich foods, such as bananas, oranges, spinach, and potatoes, may help counteract furosemide-induced potassium losses, though patients should follow their healthcare provider’s guidance regarding potassium intake.[179] Sodium restriction may be recommended for patients with heart failure or hypertension, though excessive sodium restriction should be avoided to prevent complications.[180] Patients should be cautious with salt substitutes and should read food labels carefully to monitor sodium and potassium content.[181] Regular meals and consistent eating patterns may help maintain stable medication absorption and effectiveness.[182] Healthcare providers may recommend consultation with a registered dietitian for personalized dietary guidance based on individual medical conditions and treatment goals.[183]
Can furosemide tablets be split or crushed if I have difficulty swallowing?
The ability to split or crush furosemide tablets depends on the specific formulation and manufacturer specifications.[184] Many furosemide tablets are scored and may be safely split to achieve smaller doses when recommended by a healthcare provider.[185] However, crushing tablets may alter the medication’s absorption characteristics and should only be done under specific medical guidance.[186] Patients with swallowing difficulties should discuss alternative options with their healthcare providers, who may recommend liquid formulations, different dosing strategies, or swallowing aids.[187] If tablet splitting is approved, patients should use appropriate pill splitters to ensure accurate dosing and should store split tablets properly to maintain stability.[188] Crushed tablets may be mixed with small amounts of food or liquid as directed by healthcare providers, but the mixture should be consumed immediately.[189] Healthcare providers should evaluate individual patient needs and provide specific instructions for tablet modification when appropriate.[190]
Disclaimer: This product information is provided for educational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider before starting, stopping, or modifying any medication regimen. The information presented herein does not constitute medical advice and should not be used as a substitute for consultation with a licensed healthcare professional. Individual patient responses to medications may vary significantly, and treatment decisions should always be made in consultation with appropriate medical supervision. This document does not imply endorsement, recommendation, or guarantee of safety or efficacy for any particular use. Healthcare providers should refer to current prescribing information and clinical guidelines when making treatment decisions.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Hydrochlorothiazide / Triamterene Tablets
Hydrochlorothiazide / Triamterene Tablets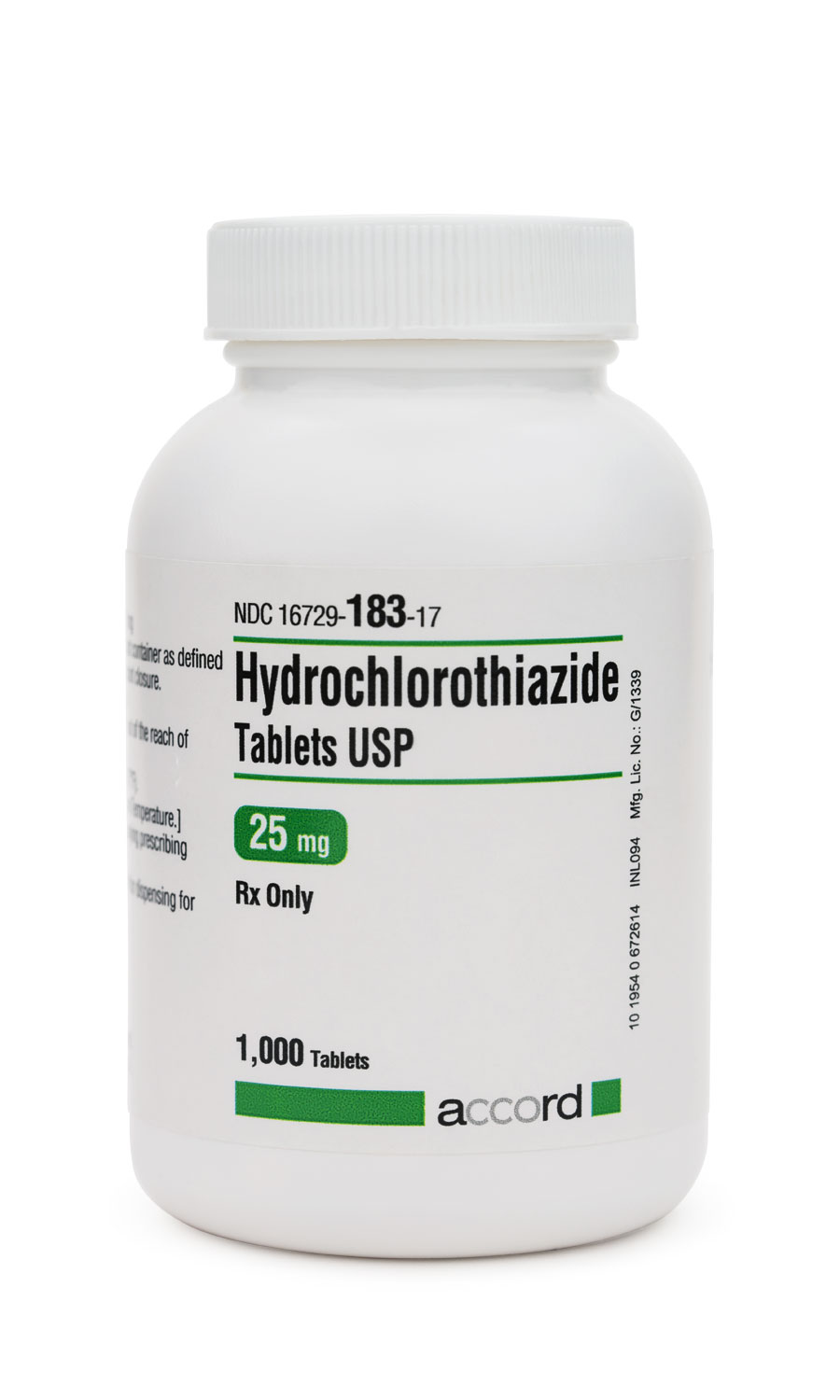 Hydrochlorothiazide Tablets
Hydrochlorothiazide Tablets Hydrocortisone Tablets
Hydrocortisone Tablets Lisinopril Tablets
Lisinopril Tablets Tirzepatide / Niacinamide Injection
Tirzepatide / Niacinamide Injection Cyanocobalamin (Vitamin B12) Injection
Cyanocobalamin (Vitamin B12) Injection