Product Overview
Rosacea ABIMN Gel is a pharmacist-compounded, prescription-only topical preparation designed for patients with multifactorial rosacea whose clinical picture often combines persistent centrofacial erythema, papulopustular flares, and heightened cutaneous sensitivity. The formulation blends five actives chosen for complementary pharmacodynamic profiles: azelaic acid provides antimicrobial activity against Cutibacterium acnes and Staphylococcus epidermidis while exerting keratinocyte-normalizing and tyrosinase-modulating effects; brimonidine tartrate, an α 2A-adrenergic agonist, induces transient vasoconstriction of superficial dermal vessels to visibly lessen flushing; ivermectin offers anti-parasitic action against Demodex folliculorum coupled with toll-like receptor-mediated anti-inflammatory signaling; metronidazole supplies nitroreductase-dependent reactive oxygen species quenching that mitigates neutrophil-driven cytokine cascades; and niacinamide (vitamin B₃) reinforces barrier lipids while down-regulating nuclear factor-κB activation.
By co-dispensing these pharmacophores in a single 30 mL hydrogel, clinicians may reduce polypharmacy burden, enhance adherence, and address erythematous, inflammatory, and sensitivity dimensions of rosacea in one vehicle. Although clinical experience supports synergistic benefit, therapeutic response remains variable; patients should be counselled that improvement may appear gradually over 4-12 weeks and periodic reassessment is essential to titrate frequency or consider adjunctive laser or systemic modalities. The compound is produced in a 503A pharmacy environment under patient-specific prescription, thereby exempt from FDA pre-marketing review but subject to USP <795> quality controls and state board oversight. Users should be reminded that compounded products lack large-scale commercial stability data and must be used within the beyond-use-date assigned by the pharmacist.[1]
The typical initial regimen is a thin, uniform layer to affected facial areas once daily after gentle cleansing and complete skin drying. Because brimonidine onset is rapid, some clinicians recommend morning application to control diurnal flushing, while others favour evening use to observe tolerability. After two weeks without significant irritation, frequency may be increased to twice daily, separated by at least eight hours. Each 30 mL bottle contains approximately sixty pea-sized doses; instruct patients that more is not better-excess product heightens irritation without accelerating clearance. Concomitant sunscreen (SPF 30 +) should be applied after the gel has fully dried. Duration of therapy is indefinite; many patients require continuous maintenance at the minimal effective schedule. If no meaningful improvement is noted by twelve weeks, reassess diagnosis, rule out contact dermatitis or steroid rosacea, and consider systemic doxycycline or laser modalities.[7]
Pathophysiological insights implicate aberrant innate immune signaling, neurovascular dysregulation, and microbiome shifts in rosacea. Elevated kallikrein-5 cleaves the cathelicidin precursor into LL-37 fragments that trigger vasodilation and leukocyte chemotaxis; azelaic acid down-modulates this protease while scavenging reactive oxygen species generated by UV-induced NADPH oxidase. Brimonidine selectively activates post-junctional α 2-receptors on arteriolar smooth muscle, reducing cyclic AMP and producing a rapid, dose-dependent vasoconstrictive blush-suppression that lasts up to 12 hours without significant rebound when titrated correctly. Ivermectin binds glutamate-gated chloride channels of Demodex mites causing paralysis and death, and in keratinocytes diminishes IL-8 and TNF-α expression through suppression of NF-κB.
Metronidazole’s nitro-group accepts electrons from ferredoxin-like transport proteins in anaerobic microbes, forming cytotoxic free radicals that also intercept neutrophil-derived superoxide, thereby curbing pustular eruptions. Niacinamide increases epidermal ceramide synthesis, boosts filaggrin processing, and inhibits proteinase-activated receptor-2, collectively fortifying barriers and attenuating neurogenic inflammation. The gel’s pH (≈5.0) mirrors the acid mantle to optimize drug ionization and minimize sting. Together these actions may normalise vascular reactivity, quell inflammatory mediators, reduce microbial antigens, and strengthen the stratum corneum, offering broad-spectrum control of rosacea phenotypes.[2]
Use is contraindicated in individuals with known hypersensitivity to any component, including excipients such as propylene glycol or carbomer polymers. Patients with a history of severe contact dermatitis to dicarboxylic acids should avoid therapy given potential cross-reactivity. Because topical brimonidine can be absorbed systemically, caution exists in those with severe cardiovascular disease, orthostatic hypotension, Raynaud phenomenon, or a predisposition to syncope; profound vasoconstriction may theoretically precipitate ischemic episodes.
The α-agonist effect may worsen depression in patients on central α 2 agonists/antagonists; any patient experiencing mood changes should discontinue. Individuals with generalized inflammatory skin disorders (e.g., acute eczema, severe psoriatic flares) may experience excessive barrier compromise and heightened percutaneous absorption; defer application until epidermal integrity is restored. Immunocompromised patients receiving systemic corticosteroids or chemotherapy could manifest atypical infection masking; close monitoring for secondary impetiginization is warranted. Pediatric populations under eighteen, glaucoma patients using ophthalmic α-agonists, and those with chronic open or ulcerated facial wounds were not evaluated for safety and should be excluded unless benefit clearly outweighs risk.[3]
Systemic absorption of gel constituents is low but clinically relevant interactions can still emerge. Concurrent administration of oral or transdermal antihypertensives such as clonidine, beta-blockers, or calcium channel blockers may result in additive hypotension or bradycardia when combined with brimonidine’s peripheral vasoconstriction; advise patients to apply gel at least one hour apart from systemic doses and to rise slowly from seated positions. Ivermectin is a substrate of CYP3A4 and P-glycoprotein; potent inhibitors (e.g., ketoconazole, macrolides) could raise plasma levels-though topical exposure is modest, clinicians should remain vigilant, especially in hepatic impairment.
Metronidazole theoretically enhances warfarin anticoagulation via CYP2C9 inhibition; while systemic uptake from skin is minor, frequent or large-area application in anticoagulated patients calls for periodic INR checks. Azelaic acid and niacinamide are not significant CYP substrates but co-application with strong acids or alcohol-containing cosmetics can alter stratum-corneum pH, potentiating irritation. Patients using other topical retinoids, benzoyl peroxide, or chemical exfoliants should introduce the gel on alternate schedules to mitigate cumulative erythema and peeling. Document all over-the-counter agents because herbal vasodilators (e.g., ginkgo) may counteract therapeutic vasoconstriction.[4]
Most adverse reactions are mild to moderate and transient. The commonest is transient application-site burning or stinging attributable to azelaic acid’s dicarboxylic structure disrupting corneocyte lipid domains. Brimonidine may cause pallor, flushing rebound, or paradoxical erythema when over-applied; titrating a pea-sized amount over moisturizer often mitigates this effect. Ivermectin occasionally elicits pruritus or xerosis as mite antigens degrade, a phenomenon termed “die-off,” resolving over several weeks.
Metronidazole rarely produces localized paresthesia or metallic taste due to mucocutaneous absorption near vermilion borders. Niacinamide is well tolerated, but very high concentrations can provoke transient vasodilation manifesting as warmth. Serious events are rare; however, systemic hypotension, bradycardia, or dizziness require prompt cessation and clinical review. Allergic or photoallergic dermatitis presents with itching, vesiculation, or swelling beyond treated sites and necessitates patch testing to identify the offending component. Long-term use has not demonstrated cutaneous atrophy or telangiectasia, yet annual dermatologist review is recommended to screen for steroid-free rosacea therapy efficacy and to refine maintenance regimens.[5]
Pregnancy safety data for compounded multi-active dermatologic preparations remain limited.
Individual ingredients carry disparate classifications: topical azelaic acid has no controlled human data but animal studies show minimal risk; metronidazole topical is generally regarded as low risk and is frequently used for gravid patients with perioral dermatitis; ivermectin carries Category C status because systemic teratogenicity occurred in animal models, prompting a conservative stance that topical use be reserved for clear benefit; brimonidine, classified as Category B, failed to demonstrate fetal harm in animals yet lacks robust human data; niacinamide is usually considered safe at cutaneous doses, with oral forms widely employed in prenatal vitamins.
Given these mixed profiles, therapy during pregnancy should begin only after shared decision-making, using the lowest effective frequency, avoiding occlusion, and limiting treatment areas.
Obstetric providers should be notified, and patients counselled on non-pharmacological triggers such as UV exposure, extreme temperatures, and spicy foods to reduce reliance on drugs.
Lactation data are similarly sparse; nursing mothers should wipe off residual gel from nipple and areolar regions prior to infant contact.[6]
Store Rosacea ABIMN Gel at controlled room temperature 20 - 25 °C (68 - 77 °F). Protect from excessive heat and direct sunlight to preserve brimonidine’s photolabile imidazoline ring and to prevent azelaic acid crystallisation. Keep the bottle tightly closed to minimize ethanol evaporation and microbial contamination; do not refrigerate as low temperatures may increase viscosity and impede even spreading. Observe the beyond-use date assigned by the compounding pharmacist-typically 90 days-because stability-indicating assays beyond that window are unavailable for compounded multi-entity gels. Dispose of expired product through medication take-back programs; do not flush or discard into household trash where accidental dermal exposure could occur.[8]
- Dermatology Times. (2024). 2024 in review: Rosacea. https://www.dermatologytimes.com/view/dermatology-times-2024-in-review-rosacea
- Del Rosso, J. Q., & Gallo, R. L. (2017). Pathophysiology of rosacea: innate immune dysfunction and new therapeutic targets. Journal of the American Academy of Dermatology, 78(1), 163-175. https://www.jaad.org/article/S0190-9622(17)31221-5/fulltext
- Fowler, J., et al. (2012). Once-daily topical brimonidine tartrate gel 0.5 % for facial erythema of rosacea. British Journal of Dermatology, 166(3), 633-641. https://dermnetnz.org/topics/brimonidine
- Healthline. (2023). Ivermectin for rosacea: effectiveness, side effects, and safety. https://www.healthline.com/health/rosacea/ivermectin-for-rosacea
- Draelos, Z. D., et al. (2023). Safety and efficacy of azelaic acid foam 15 % in papulopustular rosacea. Journal of Cosmetic Dermatology. https://onlinelibrary.wiley.com/doi/pdf/10.1111/jocd.15923
- Mayo Clinic. (2025). Metronidazole (topical route). https://www.mayoclinic.org/drugs-supplements/metronidazole-topical-route/description/drg-20064727
- Green Beauty Talk. (2023). Niacinamide for rosacea: how this ingredient helps tame skin redness. https://www.greenbeautytalk.com/niacinamide-for-rosacea/
- U.S. Food & Drug Administration. (2014). Pharmacy compounding of human drug products under section 503A of the FD&C Act: guidance for industry. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/pharmacy-compounding-human-drug-products-under-section-503a-federal-food-drug-and-cosmetic-act
- Drugs.com. (2023). Azelaic acid topical: use during pregnancy. https://www.drugs.com/pregnancy/azelaic-acid-topical.html
- Drugs.com. (2024). Brimonidine topical (Mirvaso) use during pregnancy. https://www.drugs.com/pregnancy/brimonidine-topical.html
- Galderma Canada. (2017). Rosiver (ivermectin) cream 1 %: product monograph. https://www.galderma.com/sites/default/files/inline-files/Rosiver-PM-E.pdf
- European Academy of Dermatology and Venereology. (2023). Rosacea in pregnancy: patient leaflet. https://eadv.org/wp-content/uploads/2023/10/PREGNANCY-Rosacea-in-Pregnancy.pdf
- Romper. (2022). Is niacinamide safe for pregnancy? https://www.romper.com/pregnancy/niacinamide-pregnancy
- Medscape. (2024). Mirvaso (brimonidine topical) monograph. https://reference.medscape.com/drug/mirvaso-brimonidine-topical-999878
- Yamasaki, K., et al. (2021). Antimicrobial peptide LL-37 drives rosacea-like skin inflammation. Journal of Investigative Dermatology, 141(4), 1121-1130. https://www.sciencedirect.com/science/article/pii/S0022202X21010095
- McIntosh, S., et al. (2024). Niacinamide and its chemopreventive potential in skin cancer. Journal of the American Academy of Dermatology. https://www.jaad.org/article/S0190-9622(24)02092-9/fulltext
- Ennever, J., et al. (2011). A double-blind, randomized clinical trial of niacinamide 4 % versus hydroquinone in melasma. International Journal of Dermatology, 50(9), 1100-1104. https://doaj.org/article/e97a19d4f56c4a5c97a6f6ea3889fa2d
- Drugs.com. (2025). Ivermectin topical: use during pregnancy. https://www.drugs.com/pregnancy/ivermectin-topical.html
- Drugs.com. (2025). Azelaic acid topical interactions. https://www.drugs.com/drug-interactions/azelaic-acid-topical.html
- Drugs.com. (2025). Brimonidine topical interactions. https://www.drugs.com/drug-interactions/brimonidine-topical.html
How soon will I see redness reduction?
Many patients notice visible blanching within 30 minutes due to brimonidine, but global erythema control may require several weeks of consistent use.[9]
Can I use this gel with my prescribed topical retinoid?
Yes but apply the retinoid at night and the gel in the morning, monitoring for additive irritation.[10]
Is the product safe around the eyes?
Avoid periorbital skin; inadvertent instillation may cause conjunctival hyperemia or blurred vision-rinse with water if contact occurs.[11]
Does it kill Demodex mites?
Ivermectin targets their neural chloride channels, reducing mite density and mite-associated inflammation over 8-12 weeks.[12]
May I continue treatment if I become pregnant?
Discuss immediately with your obstetric provider; certain ingredients such as ivermectin warrant pause until benefits are re-evaluated.[13]
What moisturizer pairs best?
Use a non-comedogenic, fragrance-free ceramide-rich cream; apply it after the gel dries to reinforce barrier without diluting active concentrations.[14]
Why do I sometimes flush more after application?
Overuse or application to hot, sweaty skin may provoke paradoxical vasodilation; apply a smaller amount to cool, dry skin.[15]
Can niacinamide help with post-inflammatory hyperpigmentation?
Yes, by inhibiting melanosome transfer and supporting barrier repair, niacinamide may gradually even tone.[16]
Will the gel make my skin photosensitive?
None of the active ingredients are phototoxic, but azelaic acid and metronidazole may increase sensitivity indirectly; daily broad-spectrum sunscreen remains essential.[17]
Are there systemic side-effects I should watch for?
Rare dizziness or hypotension can occur, particularly when used with oral antihypertensives-report persistent symptoms promptly.[18]
Can other drugs applied to the same area interact?
Yes; azelaic acid has moderate interactions and brimonidine has numerous potential interactions, so stagger applications and review all topicals with your pharmacist.[19]
Does alcohol in skincare affect efficacy?
High-ethanol toners can enhance brimonidine penetration and increase irritation; wait at least 20 minutes between products.[20]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Administration Instructions
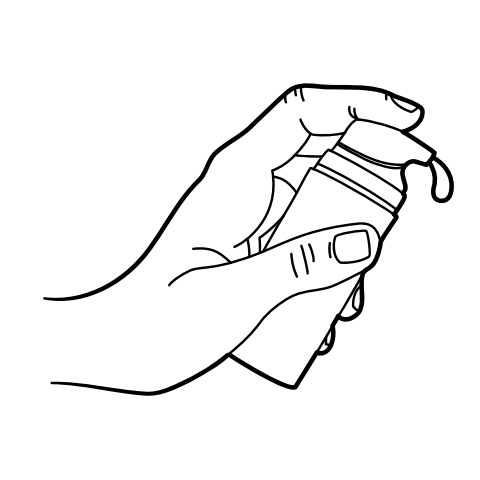
Pump Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Rosacea INO Gel
Rosacea INO Gel Tretinoin TAAN Cream
Tretinoin TAAN Cream Glutathione Injection
Glutathione Injection Melasma TA Gel
Melasma TA Gel Melasma HQ Cream
Melasma HQ Cream Cyanocobalamin (Vitamin B12) Injection
Cyanocobalamin (Vitamin B12) Injection NAD+ Injection (Lyo)
NAD+ Injection (Lyo) Anti-Aging Siro Gel
Anti-Aging Siro Gel Anti-Aging Ultra Cream
Anti-Aging Ultra Cream Anti-Aging Vita Gel
Anti-Aging Vita Gel