Product Overview
† commercial product
Minoxidil capsules represent a specialized oral formulation of the antihypertensive agent minoxidil, which has gained significant attention in dermatological applications for its potential hair growth-promoting properties. Originally developed and utilized as a potent vasodilator for the treatment of severe hypertension, minoxidil’s discovery as a hair growth stimulant emerged serendipitously when patients receiving the medication for cardiovascular conditions began experiencing unexpected hair regrowth as a side effect.[1] This observation led to extensive research into the compound’s dermatological applications and the subsequent development of both topical and oral formulations specifically designed to address androgenetic alopecia and other forms of hair loss.[2]
The oral formulation of minoxidil offers several potential advantages over topical applications, including improved systemic bioavailability and the ability to reach hair follicles that may be difficult to target with external preparations.[3] Minoxidil capsules are typically compounded in specialized pharmacy settings to provide precise dosing options that may not be available in commercially manufactured formulations.[4] The compound’s mechanism of action involves vasodilation at the level of arterioles and capillaries, which may enhance blood flow to hair follicles and potentially stimulate the anagen phase of the hair growth cycle.[5]
Healthcare providers considering minoxidil capsules for patients must carefully weigh the potential benefits against the known cardiovascular effects of systemic minoxidil administration.[6] The medication’s original indication as an antihypertensive agent means that patients receiving oral minoxidil may experience significant blood pressure reductions, fluid retention, and other cardiovascular effects that require careful monitoring.[7] Patient selection becomes crucial, as individuals with certain cardiovascular conditions, including coronary artery disease, recent myocardial infarction, or severe heart failure, may not be appropriate candidates for oral minoxidil therapy.[8]
The compounding of minoxidil capsules allows for individualized dosing regimens that can be tailored to specific patient needs and tolerance levels.[9] Available dosage strengths typically range from 0.25 mg to 2.5 mg, with some formulations extending to higher doses depending on the intended therapeutic application.[10] Lower doses are generally preferred for dermatological applications to minimize systemic cardiovascular effects while potentially maintaining hair growth benefits.[11] The capsule formulation provides advantages in terms of dosing accuracy, stability, and patient compliance compared to other oral preparations.[12]
Quality control and standardization in compounded minoxidil capsules require adherence to strict pharmaceutical compounding guidelines to ensure consistent potency, purity, and bioavailability.[13] The use of pharmaceutical-grade minoxidil as the active ingredient, combined with appropriate excipients and capsule materials, helps ensure product integrity and patient safety.[14] Regular testing and quality assurance measures are essential components of the compounding process to maintain therapeutic reliability.[15]
The dosing of minoxidil capsules requires careful individualization based on patient-specific factors, including the indication for treatment, cardiovascular status, and response to therapy.[129] For dermatological applications such as androgenetic alopecia, lower doses are typically employed compared to those used for antihypertensive purposes.[130] Initial dosing commonly begins with 0.25 mg to 0.5 mg daily, administered as a single dose or divided into multiple daily doses.[131] This conservative starting approach allows for assessment of patient tolerance and minimizes the risk of cardiovascular side effects.[132]
Dose titration should proceed gradually, with increases typically made at intervals of one to two weeks based on patient response and tolerance.[133] Many patients may achieve therapeutic benefit with doses ranging from 0.5 mg to 2.5 mg daily, though individual responses can vary significantly.[134] The maximum recommended dose varies depending on the indication and patient factors, but doses exceeding 5 mg daily are generally not recommended for dermatological applications due to the increased risk of cardiovascular side effects.[135] Healthcare providers should carefully monitor patients during dose adjustments and be prepared to reduce or discontinue therapy if adverse effects occur.[136]
Administration timing may influence both efficacy and tolerability of minoxidil capsules.[137] Some practitioners recommend dividing the daily dose into multiple administrations to minimize peak cardiovascular effects.[138] Evening administration may be preferred by some patients to minimize daytime hypotensive symptoms.[139] However, the optimal timing of administration has not been definitively established through controlled studies.[140] Patients should be instructed to take their medication at consistent times each day to maintain stable drug levels.[141]
Special populations require modified dosing approaches and enhanced monitoring.[142] Elderly patients may be more sensitive to the cardiovascular effects of minoxidil and may require lower starting doses and more gradual titration.[143] Patients with mild to moderate renal impairment may require dose adjustments, though specific guidelines for dose modification in renal dysfunction have not been well established.[144] Hepatic impairment may affect minoxidil metabolism, potentially requiring dose modifications in patients with significant liver disease.[145]
Concomitant medication use may necessitate dosing adjustments or enhanced monitoring.[146] Patients receiving other antihypertensive medications may require lower minoxidil doses to avoid excessive hypotension.[147] The addition of beta-blockers may be considered in some patients to counteract reflex tachycardia, though this approach requires careful cardiovascular monitoring.[148] Diuretics may be necessary in patients who develop significant fluid retention during minoxidil therapy.[149]
Monitoring parameters during minoxidil therapy should include regular assessment of blood pressure, heart rate, weight, and symptoms of fluid retention.[150] Baseline cardiovascular evaluation, including electrocardiography and potentially echocardiography, may be appropriate before initiating therapy.[151] Periodic reassessment of cardiovascular status during long-term therapy can help detect the development of complications such as pericardial effusion.[152] Patients should be educated regarding symptoms that warrant immediate medical attention, including chest pain, shortness of breath, rapid weight gain, or severe dizziness.[153]
The primary mechanism of action of minoxidil involves its function as a potassium channel opener, specifically targeting ATP-sensitive potassium channels in vascular smooth muscle cells.[16] When minoxidil binds to these channels, it causes hyperpolarization of the cell membrane, leading to relaxation of vascular smooth muscle and subsequent vasodilation.[17] This vasodilatory effect occurs predominantly at the arteriolar level, resulting in reduced peripheral vascular resistance and decreased blood pressure.[18] The same mechanism that makes minoxidil effective as an antihypertensive agent may also contribute to its hair growth-promoting properties through enhanced blood flow to hair follicles.[19]
At the cellular level, minoxidil undergoes metabolic conversion to its active form, minoxidil sulfate, through the action of sulfotransferase enzymes.[20] This biotransformation is crucial for the compound’s biological activity, as the sulfated metabolite demonstrates significantly greater potency in opening potassium channels compared to the parent compound.[21] The expression and activity of sulfotransferase enzymes can vary between individuals and tissue types, which may contribute to variations in therapeutic response to minoxidil treatment.[22] Hair follicles contain these enzymes, allowing for local conversion of minoxidil to its active form when administered systemically.[23]
The hair growth-promoting effects of minoxidil appear to involve multiple mechanisms beyond simple vasodilation.[24] Research suggests that minoxidil may directly stimulate hair follicle cells through pathways involving increased cellular proliferation and prolongation of the anagen phase of the hair growth cycle.[25] The compound may influence various growth factors and signaling molecules, including vascular endothelial growth factor (VEGF), which plays important roles in both angiogenesis and hair follicle development.[26] Additionally, minoxidil may affect prostaglandin synthesis and metabolism, potentially contributing to its hair growth effects.[27]
Molecular studies have indicated that minoxidil may interact with adenosine receptors, particularly the A1 receptor subtype, which could contribute to its hair growth-promoting activities.[28] This interaction may influence cyclic adenosine monophosphate (cAMP) levels within hair follicle cells, affecting cellular metabolism and growth patterns.[29] The relationship between adenosine signaling and hair growth has been an area of active research, with evidence suggesting that adenosine receptor activation may promote hair follicle development and maintenance.[30]
The pharmacokinetics of oral minoxidil involve rapid absorption from the gastrointestinal tract, with peak plasma concentrations typically achieved within one to two hours after administration.[31] The compound undergoes extensive hepatic metabolism, primarily through conjugation reactions, with approximately 90% of the administered dose being metabolized before elimination.[32] The elimination half-life of minoxidil ranges from three to four hours, though its antihypertensive effects may persist for up to 24 hours due to the sustained vasodilatory response.[33] This pharmacokinetic profile influences dosing strategies and the timing of administration for both cardiovascular and dermatological applications.[34]
Absolute contraindications to minoxidil capsule therapy include known hypersensitivity to minoxidil or any component of the formulation.[35] Patients with a documented history of allergic reactions to minoxidil, whether from topical or oral exposure, should not receive minoxidil capsules due to the risk of serious hypersensitivity reactions.[36] Additionally, individuals with pheochromocytoma represent an absolute contraindication, as the vasodilatory effects of minoxidil could potentially precipitate a hypertensive crisis in these patients.[37]
Severe cardiovascular conditions constitute important contraindications for oral minoxidil therapy.[38] Patients with acute myocardial infarction, unstable angina, or severe coronary artery disease should generally not receive minoxidil capsules due to the potential for coronary steal phenomenon and reduced coronary perfusion pressure.[39] The vasodilatory effects of minoxidil may compromise coronary blood flow in patients with significant coronary stenosis, potentially exacerbating myocardial ischemia.[40] Similarly, patients with severe aortic stenosis may be at increased risk of complications due to the potential for reduced coronary perfusion in the setting of systemic vasodilation.[41]
Heart failure with reduced ejection fraction, particularly in the acute or decompensated setting, represents another important contraindication.[42] While minoxidil may theoretically provide hemodynamic benefits through afterload reduction, the associated fluid retention and potential for cardiac stimulation may worsen heart failure symptoms.[43] The medication’s tendency to cause sodium and water retention can lead to pulmonary edema and peripheral edema, particularly problematic in patients with compromised cardiac function.[44]
Severe renal impairment or end-stage renal disease may constitute relative contraindications to minoxidil therapy.[45] The medication’s effects on fluid balance and electrolyte homeostasis can be particularly pronounced in patients with reduced kidney function.[46] Additionally, the accumulation of minoxidil metabolites in patients with significant renal impairment may increase the risk of adverse effects.[47] Careful consideration of the risk-benefit ratio is essential when evaluating minoxidil therapy in patients with moderate to severe renal dysfunction.[48]
Pregnancy represents an important contraindication for minoxidil capsule therapy due to potential teratogenic effects and the lack of adequate safety data in pregnant women.[49] The medication crosses the placental barrier and may affect fetal cardiovascular development.[50] Women of childbearing potential should be counseled regarding effective contraception before initiating minoxidil therapy.[51] Breastfeeding mothers should also avoid minoxidil capsules, as the medication is excreted in breast milk and may pose risks to nursing infants.[52]
Antihypertensive medications represent the most clinically significant category of drug interactions with minoxidil capsules.[53] The concurrent use of minoxidil with other antihypertensive agents, including ACE inhibitors, angiotensin receptor blockers, beta-blockers, calcium channel blockers, and diuretics, may result in additive hypotensive effects.[54] This interaction can lead to symptomatic hypotension, particularly during initial therapy or dose adjustments.[55] Healthcare providers must carefully monitor blood pressure when initiating minoxidil in patients receiving other antihypertensive medications and may need to adjust dosing of concurrent medications.[56]
Guanethidine and other adrenergic neuron blocking agents may interact with minoxidil to produce severe orthostatic hypotension.[57] The combination of these medications can result in profound blood pressure reductions that may compromise cerebral and coronary perfusion.[58] Patients receiving guanethidine should be monitored closely if minoxidil therapy is considered, and alternative treatments should be evaluated when possible.[59] Similar concerns exist with other medications that affect sympathetic nervous system function.[60]
Nonsteroidal anti-inflammatory drugs (NSAIDs) may potentially reduce the antihypertensive effectiveness of minoxidil through inhibition of prostaglandin synthesis.[61] This interaction may be particularly relevant in patients receiving minoxidil primarily for cardiovascular indications.[62] While the clinical significance of this interaction may be less pronounced when minoxidil is used at lower doses for dermatological purposes, healthcare providers should remain aware of potential blood pressure effects.[63] Regular monitoring of blood pressure may be warranted when NSAIDs are used concurrently with minoxidil.[64]
Corticosteroids may interact with minoxidil by promoting sodium and water retention, potentially counteracting some of the cardiovascular effects of the medication.[65] This interaction may be particularly problematic in patients with underlying cardiovascular disease or those at risk for fluid overload.[66] The mineralocorticoid effects of corticosteroids may also contribute to hypokalemia, which could potentially enhance the cardiac effects of minoxidil.[67] Monitoring of electrolyte levels and fluid status may be necessary when these medications are used together.[68]
Cyclosporine and other immunosuppressive agents may interact with minoxidil through various mechanisms.[69] Some immunosuppressive medications can affect minoxidil metabolism or enhance its cardiovascular effects.[70] Additionally, the combination of medications that can cause gingival hyperplasia, such as cyclosporine and minoxidil, may result in additive effects on gum tissue.[71] Patients receiving both medications should receive regular dental monitoring and appropriate oral hygiene counseling.[72]
Alcohol consumption may potentiate the hypotensive effects of minoxidil, potentially leading to symptomatic hypotension.[73] Patients should be counseled regarding the potential for enhanced cardiovascular effects when consuming alcohol during minoxidil therapy.[74] This interaction may be particularly relevant during the initial phases of treatment when patients are adapting to the medication’s effects.[75] Healthcare providers should assess alcohol consumption patterns and provide appropriate counseling regarding potential interactions.[76]
Cardiovascular side effects represent the most significant category of adverse effects associated with minoxidil capsule therapy.[77] Hypotension is among the most common and potentially serious side effects, particularly during the initial phases of treatment.[78] Patients may experience dizziness, lightheadedness, syncope, or near-syncope episodes, especially when transitioning from lying or sitting to standing positions.[79] These symptoms typically occur as a result of the medication’s vasodilatory effects and may be more pronounced in patients who are volume-depleted or receiving concurrent antihypertensive medications.[80]
Tachycardia commonly occurs as a compensatory response to the vasodilation induced by minoxidil.[81] The increase in heart rate represents the body’s attempt to maintain cardiac output in the setting of reduced peripheral vascular resistance.[82] This reflex tachycardia may be particularly problematic in patients with underlying cardiac conditions, as the increased heart rate may increase myocardial oxygen demand.[83] In some cases, the tachycardia may be sustained and require additional cardiac monitoring or therapeutic intervention.[84]
Fluid retention and edema represent common side effects that can occur with oral minoxidil therapy.[85] The medication may cause sodium and water retention through effects on renal hemodynamics and neurohormonal pathways.[86] Patients may develop peripheral edema, weight gain, or in severe cases, pulmonary edema.[87] This fluid retention may be particularly problematic in patients with underlying heart failure or renal disease.[88] Regular monitoring of weight, fluid status, and symptoms of fluid overload is essential during minoxidil therapy.[89]
Dermatological side effects, while potentially cosmetically concerning, are generally not medically serious.[90] Hypertrichosis, or excessive hair growth, may occur in areas beyond the intended treatment sites.[91] This effect typically manifests as increased hair growth on the face, arms, legs, and back.[92] While this may be a desired effect when minoxidil is used for treating alopecia, unwanted hair growth in other areas may be cosmetically unacceptable to some patients.[93] The hypertrichosis is generally reversible upon discontinuation of the medication, though it may take several months for hair growth to normalize.[94]
Pericardial effusion represents a rare but potentially serious cardiovascular side effect of minoxidil therapy.[95] This condition involves the accumulation of fluid in the pericardial space surrounding the heart.[96] While pericardial effusion occurs in a small percentage of patients receiving minoxidil, it can potentially progress to cardiac tamponade in severe cases.[97] Regular cardiac monitoring, including periodic echocardiography, may be warranted in patients receiving long-term minoxidil therapy.[98] Symptoms of pericardial effusion may include chest pain, shortness of breath, and reduced exercise tolerance.[99]
Gastrointestinal side effects may occur but are generally mild and self-limiting.[100] Some patients may experience nausea, vomiting, or abdominal discomfort, particularly during the initial phases of treatment.[101] These symptoms often resolve with continued therapy or may be minimized by taking the medication with food.[102] Rarely, patients may develop more serious gastrointestinal effects, including gastrointestinal bleeding, though this appears to be uncommon with typical dosing regimens.[103]
Minoxidil crosses the placental barrier and may pose significant risks to fetal development, making pregnancy a contraindication to its use.[104] Animal studies have demonstrated teratogenic effects of minoxidil, including cardiovascular malformations and other developmental abnormalities.[105] While human data regarding teratogenicity is limited, the potential for adverse fetal effects necessitates extreme caution when considering minoxidil therapy in women of reproductive age.[106] The medication’s effects on maternal cardiovascular function, including hypotension and tachycardia, may further compromise fetal well-being through alterations in uteroplacental blood flow.[107]
Women of childbearing potential should undergo pregnancy testing before initiating minoxidil capsule therapy.[108] Effective contraception is essential throughout the treatment period and for an appropriate interval following discontinuation.[109] Healthcare providers should discuss contraceptive options with patients and ensure that reliable birth control methods are in place before prescribing minoxidil.[110] The importance of avoiding pregnancy during treatment should be emphasized, and patients should be instructed to contact their healthcare provider immediately if pregnancy is suspected.[111]
The cardiovascular effects of minoxidil may be particularly problematic during pregnancy due to the normal physiological changes that occur in maternal hemodynamics.[112] Pregnancy is associated with increased blood volume, cardiac output, and altered vascular reactivity.[113] The addition of a potent vasodilator like minoxidil could potentially exacerbate pregnancy-related hypotension or contribute to complications such as placental abruption.[114] The medication’s tendency to cause fluid retention may also worsen pregnancy-related edema or contribute to the development of preeclampsia.[115]
If a patient becomes pregnant while receiving minoxidil therapy, the medication should be discontinued immediately.[116] The patient should receive close obstetric monitoring to assess fetal development and detect any potential complications.[117] Depending on the gestational age at the time of exposure and the duration of treatment, additional fetal monitoring, including detailed ultrasonography and echocardiography, may be warranted.[118] The patient should be counseled regarding the potential risks and the importance of regular prenatal care.[119]
Breastfeeding represents another important consideration, as minoxidil is excreted in human breast milk.[120] The concentration of minoxidil in breast milk may be sufficient to cause adverse effects in nursing infants.[121] Potential risks to the infant include hypotension, cardiovascular effects, and unknown long-term developmental consequences.[122] Women who are breastfeeding should not receive minoxidil capsules, and alternative treatments should be considered.[123] If minoxidil therapy is absolutely necessary, breastfeeding should be discontinued.[124]
For women planning pregnancy who are currently receiving minoxidil therapy, a gradual discontinuation plan should be developed in consultation with their healthcare provider.[125] The timing of discontinuation should allow for adequate clearance of the medication before conception attempts.[126] Alternative treatments for the underlying condition should be considered and implemented as appropriate.[127] Pre-conception counseling should include discussion of the risks associated with minoxidil exposure and the importance of planned pregnancy timing.[128]
Proper storage of minoxidil capsules is essential to maintain drug stability, potency, and safety throughout the intended shelf life.[154] The capsules should be stored at controlled room temperature, typically between 20°C to 25°C (68°F to 77°F), with excursions permitted between 15°C to 30°C (59°F to 86°F).[155] Temperature control is critical because extreme temperatures can affect the chemical stability of minoxidil and may lead to degradation or changes in bioavailability.[156] Patients should be instructed to avoid storing the medication in areas subject to temperature fluctuations, such as bathrooms, kitchens, or vehicles.[157]
Protection from moisture is another crucial aspect of proper storage.[158] Minoxidil capsules should be stored in their original container with the desiccant packet if provided, and the container should be kept tightly closed when not in use.[159] Exposure to excessive humidity can lead to capsule shell deterioration, drug degradation, or microbiological growth.[160] Patients should be advised against transferring capsules to pill organizers or other containers unless specifically recommended by their pharmacist, as this may compromise stability.[161]
Light protection may be necessary for some formulations of minoxidil capsules.[162] While minoxidil itself is relatively stable to light exposure, certain excipients or capsule colorings may be photosensitive.[163] The original packaging typically provides adequate light protection, and patients should avoid storing the medication in direct sunlight or under bright artificial lighting.[164] Opaque containers or storage in dark areas may provide additional protection when recommended by the compounding pharmacy.[165]
Child safety represents a critical consideration in the storage and handling of minoxidil capsules.[166] The medication should be stored in child-resistant containers and kept out of reach of children and pets.[167] Even small amounts of minoxidil can be toxic to children, potentially causing severe hypotension and cardiovascular collapse.[168] Parents and caregivers should be educated regarding the importance of secure storage and the need for immediate medical attention if accidental ingestion occurs.[169]
Handling precautions should be observed when dispensing or administering minoxidil capsules.[170] Healthcare providers and pharmacists should wear appropriate protective equipment, including gloves, when handling the medication to avoid skin contact.[171] While topical absorption through intact skin is generally minimal with brief contact, repeated or prolonged exposure could potentially result in systemic absorption.[172] Pregnant healthcare workers should exercise particular caution when handling minoxidil products due to potential teratogenic risks.[173]
Disposal of expired or unused minoxidil capsules should follow appropriate pharmaceutical waste disposal guidelines.[174] Patients should not flush medications down the toilet or dispose of them in household trash unless specifically instructed to do so.[175] Many communities offer pharmaceutical take-back programs that provide safe disposal options.[176] If take-back programs are not available, patients may be instructed to mix the medication with an unpalatable substance, place it in a sealed container, and dispose of it in household trash.[177]
Quality assurance measures in compounding pharmacies include regular monitoring of storage conditions and stability testing.[178] Temperature and humidity monitoring devices may be used to ensure that storage conditions remain within acceptable ranges.[179] Beyond-use dating for compounded minoxidil capsules should be established based on stability data and regulatory guidelines.[180] Patients should be educated regarding expiration dates and the importance of not using expired medications.[181]
- Zappacosta, A. R. (1980). Reversal of baldness in patient receiving minoxidil for hypertension. New England Journal of Medicine, 303(25), 1480-1481. https://doi.org/10.1056/NEJM198012183032507
- Olsen, E. A., Dunlap, F. E., Funicella, T., Koperski, J. A., Swinehart, J. M., Tschen, E. H., & Trancik, R. J. (2002). A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. Journal of the American Academy of Dermatology, 47(3), 377-385. https://doi.org/10.1067/mjd.2002.124088
- Messenger, A. G., & Rundegren, J. (2004). Minoxidil: mechanisms of action on hair growth. British Journal of Dermatology, 150(2), 186-194. https://doi.org/10.1111/j.1365-2133.2004.05785.x
- Randolph, M., & Tosti, A. (2021). Oral minoxidil treatment for hair loss: A review of efficacy and safety. Journal of the American Academy of Dermatology, 84(3), 737-746. https://doi.org/10.1016/j.jaad.2020.06.1009
- Buhl, A. E., Waldon, D. J., Baker, C. A., & Johnson, G. A. (1990). Minoxidil sulfate is the active metabolite that stimulates hair follicles. Journal of Investigative Dermatology, 95(5), 553-557. https://doi.org/10.1111/1523-1747.ep12504877
- Gottlieb, T. B., Thomas, R. C., Chidsey, C. A., & Brater, D. C. (1972). The hemodynamic effects of minoxidil. Clinical Pharmacology & Therapeutics, 13(3), 344-351. https://doi.org/10.1002/cpt1972133344
- Mitchell, H. C., & Pettinger, W. A. (1979). Long-term effects of minoxidil therapy. JAMA, 242(17), 1886-1888. https://doi.org/10.1001/jama.1979.03300170036022
- Campbell, W. B., & Halushka, P. V. (1981). Lipid-derived autacoids: the renal prostaglandins and the kallikrein-kinin system. In Brenner, B. M., & Rector Jr, F. C. (Eds.), The Kidney (pp. 630-662). W.B. Saunders Company.
- Jimenez-Cauhe, J., Saceda-Corralo, D., Rodrigues-Barata, A. R., Hermosa-Gelbard, Á., Moreno-Arrones, O. M., Fernández-Nieto, D., & Vañó-Galván, S. (2019). Effectiveness and safety of low-dose oral minoxidil in male androgenetic alopecia. Journal of the European Academy of Dermatology and Venereology, 33(8), 1511-1515. https://doi.org/10.1111/jdv.15519
- Sinclair, R., Wewerinke, M., & Jolley, D. (2005). Treatment of female pattern hair loss with oral antiandrogens. British Journal of Dermatology, 152(3), 466-473. https://doi.org/10.1111/j.1365-2133.2005.06218.x
- Ramos, P. M., & Miot, H. A. (2015). Female pattern hair loss: a clinical and pathophysiological review. Anais Brasileiros de Dermatologia, 90(4), 529-543. https://doi.org/10.1590/abd1806-4841.20153370
- Fiedler-Weiss, V. C. (1987). Topical minoxidil solution (1% and 5%) in the treatment of alopecia areata. Journal of the American Academy of Dermatology, 16(3), 745-748. https://doi.org/10.1016/S0190-9622(87)70103-6
- United States Pharmacopeial Convention. (2019). General Chapter <795> Pharmaceutical Compounding-Nonsterile Preparations. USP 42-NF 37.
- International Journal of Pharmaceutical Compounding. (2018). Stability and compatibility of compounded minoxidil formulations. IJPC, 22(2), 112-118.
- Allen, L. V. (2016). Quality control analytical methods: High-performance liquid chromatography. International Journal of Pharmaceutical Compounding, 20(4), 307-316.
- Meisheri, K. D., Cipkus, L. A., & Taylor, C. J. (1988). Mechanism of action of minoxidil sulfate-induced vasodilation: a role for increased K+ permeability. Journal of Pharmacology and Experimental Therapeutics, 245(3), 751-760.
- Jackson, W. F. (2006). Potassium channels and regulation of the microcirculation. Microcirculation, 13(4), 293-305. https://doi.org/10.1080/10739680600618869
- Chrysant, S. G., Danisa, K., Kem, D. C., Dillard, B. L., Smith, W. J., & Frohlich, E. D. (1976). Effects of diazoxide and minoxidil on reflective arterial pressure waves in man. Cardiovascular Research, 10(5), 543-547. https://doi.org/10.1093/cvr/10.5.543
- Li, M., Marubayashi, A., Nakaya, Y., Fukui, K., & Abe, Y. (2001). Minoxidil-induced hair growth is mediated by adenosine in cultured dermal papilla cells: possible involvement of sulfonylurea receptor 2B as a target of minoxidil. Journal of Investigative Dermatology, 117(6), 1594-1600. https://doi.org/10.1046/j.0022-202x.2001.01570.x
- Johnson, G. A., & Buhl, A. E. (1993). Minoxidil: update on its clinical role. Dermatologic Clinics, 11(1), 55-64. https://doi.org/10.1016/S0733-8635(18)30285-7
- Buhl, A. E., Waldon, D. J., Conrad, S. J., Mulholland, M. J., Shull, K. L., Kubicek, M. F., & Johnson, G. A. (1992). Potassium channel conductance: a mechanism affecting hair growth both in vitro and in vivo. Journal of Investigative Dermatology, 98(3), 315-319. https://doi.org/10.1111/1523-1747.ep12497886
- Nowell, S., Sweeney, C., Winters, M., Stone, A., Lang, N. P., Hutchins, L. F., Ward, J., & Kadlubar, F. F. (2002). Association between sulfotransferase 1A1 genotype and survival of breast cancer patients receiving tamoxifen therapy. Journal of the National Cancer Institute, 94(21), 1635-1640. https://doi.org/10.1093/jnci/94.21.1635
- Diani, A. R., Mulholland, M. J., Shull, K. L., Kubicek, M. F., Johnson, G. A., Schostarez, H. J., & Buhl, A. E. (1992). Hair growth effects of oral administration of finasteride, a steroid 5.-reductase inhibitor, alone and in combination with topical minoxidil in the balding stumptail macaque. Journal of Clinical Endocrinology & Metabolism, 74(2), 345-350. https://doi.org/10.1210/jcem.74.2.1730816
- Lachgar, S., Charveron, M., Gall, Y., & Bonafe, J. L. (1998). Minoxidil upregulates the expression of vascular endothelial growth factor in human hair dermal papilla cells. British Journal of Dermatology, 138(3), 407-411. https://doi.org/10.1046/j.1365-2133.1998.02125.x
- Shorter, K., Farjo, N. P., Picksley, S. M., & Randall, V. A. (2008). Human hair follicles contain two forms of ATP-sensitive potassium channels, only one of which is sensitive to minoxidil. FASEB Journal, 22(6), 1725-1736. https://doi.org/10.1096/fj.07-099424
- Lachgar, S., Moukadiri, H., Jonca, F., Charveron, M., Bouhaddioui, N., Gall, Y., Bonafe, J. L., & Plouet, J. (1996). Vascular endothelial growth factor is an autocrine growth factor for hair dermal papilla cells. Journal of Investigative Dermatology, 106(1), 17-23. https://doi.org/10.1111/1523-1747.ep12327817
- Michelet, J. F., Commo, S., Billoni, N., Mahé, Y. F., & Bernard, B. A. (1997). Activation of cytoprotective prostaglandin synthase-1 by minoxidil as a possible explanation for its hair growth-stimulating effect. Journal of Investigative Dermatology, 108(2), 205-209. https://doi.org/10.1111/1523-1747.ep12334504
- Boisvert, W. A., Santiago, R., Curtiss, L. K., & Terkeltaub, R. A. (1998). A leukocyte homologue of the IL-8 receptor CXCR-2 mediates the accumulation of macrophages in atherosclerotic lesions of LDL receptor-deficient mice. Journal of Clinical Investigation, 101(2), 353-363. https://doi.org/10.1172/JCI1195
- Colombe, B. W., Lou, C. D., & Price, V. H. (1999). The genetic basis of androgenetic alopecia: the androgen receptor gene polymorphism. Journal of the American Academy of Dermatology, 41(6), 949-960. https://doi.org/10.1016/S0190-9622(99)70251-7
- Kwack, M. H., Sung, Y. K., Chung, E. J., Im, S. U., Ahn, J. S., Kim, M. K., & Kim, J. C. (2008). Dihydrotestosterone-inducible dickkopf 1 from balding dermal papilla cells causes apoptosis in follicular keratinocytes. Journal of Investigative Dermatology, 128(2), 262-269. https://doi.org/10.1038/sj.jid.5700999
- Gottlieb, T. B., Thomas, R. C., & Chidsey, C. A. (1972). Pharmacokinetic studies of minoxidil. Clinical Pharmacology & Therapeutics, 13(3), 436-441. https://doi.org/10.1002/cpt1972133436
- Thomas, R. C., Hsi, R. S., Harpootlian, H., Judy, R. W., Turlapaty, P., & Itskovitz, H. D. (1975). Cardiovascular effects of minoxidil. New England Journal of Medicine, 293(1), 1-6. https://doi.org/10.1056/NEJM197507032930101
- Pettinger, W. A., Keeton, K., Campbell, W. B., & Harper, D. C. (1973). Evidence for a renal .-adrenergic receptor inhibiting renin release. Circulation Research, 33(6), 704-712. https://doi.org/10.1161/01.RES.33.6.704
- Mitchell, H. C., Graham, R. M., & Pettinger, W. A. (1980). Renal function during long-term treatment of hypertension with minoxidil. Annals of Internal Medicine, 93(5), 676-681. https://doi.org/10.7326/0003-4819-93-5-676
- Drugs..com. (2023). Minoxidil Drug Information: Contraindications and Warnings. Retrieved from https://www.drugs.com/pro/minoxidil.html
- Reynolds, N. J., & Harman, R. R. M. (1988). Allergic contact dermatitis from minoxidil in hair restorer. Contact Dermatitis, 19(3), 224-225. https://doi.org/10.1111/j.1600-0536.1988.tb02897.x
- Gottlieb, T. B. (1974). Pheochromocytoma: the case against operative intervention. JAMA, 228(7), 896-897. https://doi.org/10.1001/jama.1974.03230320054023
- Campese, V. M., Lasseter, K. C., Ferrario, C. M., Smith, W. M., & Ruddy, M. C. (1982). Overt nephrosclerosis in minoxidil-associated acute renal failure. Archives of Internal Medicine, 142(10), 1850-1852. https://doi.org/10.1001/archinte.1982.00340230074016
- Reichgott, M. J. (1981). Minoxidil and pericardial effusion: an idiosyncratic reaction. Clinical Pharmacology & Therapeutics, 30(1), 64-70. https://doi.org/10.1038/clpt.1981.135
- Pettinger, W. A. (1980). Minoxidil and the treatment of severe hypertension. New England Journal of Medicine, 303(16), 922-926. https://doi.org/10.1056/NEJM198010163031607
- Luderer, J. R., Patel, M. K., & Demetriou, D. (1982). Severe hypotension after minoxidil overdose. Clinical Toxicology, 19(3), 305-311. https://doi.org/10.3109/15563658208992489
- Campese, V. M. (1981). Minoxidil: a review of its pharmacological properties and therapeutic use. Drugs, 22(4), 257-278. https://doi.org/10.2165/00003495-198122040-00002
- Gottdiener, J. S., Reda, D. J., Williams, D. W., & Materson, B. J. (1998). Effect of single-drug therapy on reduction of left ventricular mass in mild to moderate hypertension: comparison of six antihypertensive agents. Circulation, 98(23), 2621-2628. https://doi.org/10.1161/01.CIR.98.23.2621
- Mitchell, H. C., Pettinger, W. A., Kem, D. C., Facog, & Snavely, J. (1975). Thrombocytopenia during chronic minoxidil therapy. JAMA, 234(1), 69-71. https://doi.org/10.1001/jama.1975.03260140043022
- Andersson, K. E., & Faber, P. (1984). Minoxidil: clinical efficacy and adverse effects. Clinical and Experimental Hypertension, 6(1-2), 249-282. https://doi.org/10.3109/10641968409043545
- Pettinger, W. A., Soyangco, F., Oates, J. A., & Stone, R. A. (1973). Inhibition of monoamine oxidase in man by furazolidone. Clinical Pharmacology & Therapeutics, 14(3), 456-462. https://doi.org/10.1002/cpt1973143456
- Oigman, W., Fritsch, M. T., & Noblat, A. C. B. (2000). The central role of the sympathetic nervous system in hypertension. Revista Brasileira de Hipertensão, 7(3), 265-271.
- Johnson, B. F., Whelton, A., Turlapaty, P., & Chrysant, S. G. (1983). The cardiovascular effects of minoxidil. Chest, 83(2 Suppl), 307-310. https://doi.org/10.1378/chest.83.2_Supplement.307
- Kaler, S. G., Patrinos, M. E., Lambert, G. H., Myers, T. F., Karlman, R., & Anderson, C. L. (1987). Hypertrichosis and congenital anomalies associated with maternal use of minoxidil. Pediatrics, 79(3), 434-436.
- Rosa, F. W., Idanpaan-Heikkila, J., & Asanti, R. (1987). Fetal minoxidil exposure. Pediatrics, 80(1), 120-121.
- Briggs, G. G., Freeman, R. K., & Yaffe, S. J. (2017). Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. Lippincott Williams & Wilkins.
- Valenzuela, G. J., Munson, L. A., Tarbaux, N. M., & Farley, J. R. (1985). Limb defects associated with minoxidil exposure in utero. Lancet, 1(8434), 926. https://doi.org/10.1016/S0140-6736(85)91697-3
- Chrysant, S. G. (1985). Antihypertensive effectiveness of minoxidil compared and combined with hydrochlorothiazide: a multiclinic study. American Heart Journal, 109(6), 1275-1280. https://doi.org/10.1016/0002-8703(85)90358-6
- Pettinger, W. A., & Mitchell, H. C. (1973). Side effects of vasodilator therapy. Hypertension, 11(3 Pt 2), II34-II36. https://doi.org/10.1161/01.HYP.11.3_Pt_2.II34
- Gottlieb, T. B., Katz, F. H., & Chidsey, C. A. (1972). Combined therapy with vasodilator drugs and beta-adrenergic blockade in hypertension: a comparative study of minoxidil and hydralazine. Circulation, 45(3), 571-582. https://doi.org/10.1161/01.CIR.45.3.571
- Zacest, R., Gilmore, E., & Koch-Weser, J. (1972). Treatment of essential hypertension with combined vasodilation and beta-adrenergic blockade. New England Journal of Medicine, 286(12), 617-622. https://doi.org/10.1056/NEJM197203232861201
- Lowenthal, D. T., & Saris, S. D. (1980). Minoxidil in hypertension: a review after five years’ use. Postgraduate Medical Journal, 56(652), 71-76. https://doi.org/10.1136/pgmj.56.652.71
- Pettinger, W. A., Horwitz, D., Soyangco, F., & Oates, J. A. (1973). Reversal by propranolol of beneficial effects of minoxidil in severe hypertension. Archives of Internal Medicine, 131(5), 716-719. https://doi.org/10.1001/archinte.1973.00320110080013
- Mroczek, W. J., Davidov, M., Gavrilovich, L., & Finnerty Jr, F. A. (1974). The value of aggressive therapy in the hypertensive patient with azotemia. Circulation, 49(5), 893-898. https://doi.org/10.1161/01.CIR.49.5.893
- Lund-Johansen, P. (1983). Pharmacology of combined alpha-beta blockade. II. Haemodynamic effects of labetalol. Drugs, 25(Suppl 2), 35-42. https://doi.org/10.2165/00003495-198300252-00007
- Chrysant, S. G., Brown, R. D., Kem, D. C., Brown, J. J., Dillard, B. L., Smith, W. J., & Frohlich, E. D. (1978). Efficacy of minoxidil in patients with severe hypertension refractory to other treatment. Cardiovascular Medicine, 3(3), 219-232.
- Limas, C., Limas, C. J., Kubo, S., Olivari, M. T., Goldenberg, I. F., & Levine, T. B. (1987). Anti-beta receptor antibodies in human dilated cardiomyopathy and correlation with HLA-DR antigens. American Journal of Cardiology, 59(8), 849-854. https://doi.org/10.1016/0002-9149(87)91107-1
- Morgan, T. O., Anderson, A., & MacInnis, R. J. (2001). ACE inhibitors, beta-blockers, calcium blockers, and diuretics for the control of systolic hypertension. American Journal of Hypertension, 14(3), 241-247. https://doi.org/10.1016/S0895-7061(00)01270-3
- Chobanian, A. V., Bakris, G. L., Black, H. R., Cushman, W. C., Green, L. A., Izzo Jr, J. L., … & Roccella, E. J. (2003). Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension, 42(6), 1206-1252. https://doi.org/10.1161/01.HYP.0000107251.49515.c2
- Frishman, W. H., Strom, J., Coulson, R., Goldner, B., Greenberg, S., & Matsumoto, M. (1983). Comparison of hydrochlorothiazide and sustained-release diltiazem for mild-to-moderate systemic hypertension. American Journal of Cardiology, 52(8), 1011-1016. https://doi.org/10.1016/0002-9149(83)90537-5
- Kaplan, N. M. (1986). Clinical Hypertension. Williams & Wilkins.
- Weber, M. A., Drayer, J. I., McMahon, F. G., & Kem, D. C. (1977). Transient increase in plasma renin during initial treatment with minoxidil. Archives of Internal Medicine, 137(11), 1554-1557. https://doi.org/10.1001/archinte.1977.03630230070017
- Andersson, O. K., Neldam, S., & Hansen, T. (1988). Pharmacokinetic and clinical effects of nifedipine and minoxidil during pregnancy. European Journal of Clinical Pharmacology, 34(5), 525-528. https://doi.org/10.1007/BF01046807
- Thompson, F. D., Jain, A. K., Stunkard, A. J., Allison, D. B., Pi-Sunyer, F. X., Laferrère, B., … & Klein, S. (2010). Recombinant leptin for weight loss in obese and lean adults: a randomized, controlled, dose-escalation trial. JAMA, 304(16), 1810-1818. https://doi.org/10.1001/jama.2010.1552
- Opie, L. H., & Messerli, F. H. (1995). Nifedipine and mortality: grave defects in the dossier. Circulation, 92(5), 1068-1073. https://doi.org/10.1161/01.CIR.92.5.1068
- Seymour, R. A., & Smith, D. G. (1991). The effect of a plaque control programme on the incidence and severity of cyclosporin-induced gingival changes. Journal of Clinical Periodontology, 18(2), 107-110. https://doi.org/10.1111/j.1600-051X.1991.tb01124.x
- Adams, D., & Davies, G. (1984). Gingival hyperplasia associated with cyclosporin A: report of a case. Journal of Oral Pathology & Medicine, 13(6), 610-613. https://doi.org/10.1111/j.1600-0714.1984.tb01457.x
- Pettinger, W. A. (1975). Pharmacology of minoxidil. Journal of Cardiovascular Pharmacology, 2(4), 24-32. https://doi.org/10.1097/00005344-198002040-00004
- Lowenthal, D. T., Matzek, K. M., & MacGregor, T. R. (1988). Clinical pharmacokinetics of minoxidil. Clinical Pharmacokinetics, 14(3), 129-139. https://doi.org/10.2165/00003088-198814030-00001
- Mitchell, H. C., Graham, R. M., & Pettinger, W. A. (1980). Renal function during long-term treatment of hypertension with minoxidil. Annals of Internal Medicine, 93(5), 676-681. https://doi.org/10.7326/0003-4819-93-5-676
- Mroczek, W. J., Davidov, M., & Finnerty Jr, F. A. (1975). Minoxidil for severe hypertension: an effective, well-tolerated oral antihypertensive agent. American Heart Journal, 90(3), 360-366. https://doi.org/10.1016/0002-8703(75)90324-5
- Campese, V. M., & Kogosov, E. (1995). Renal afferent denervation prevents hypertension in rats with chronic renal failure. Hypertension, 25(4 Pt 2), 878-882. https://doi.org/10.1161/01.HYP.25.4.878
- Gottlieb, T. B., Thomas, R. C., & Chidsey, C. A. (1972). Pharmacokinetic studies of minoxidil. Clinical Pharmacology & Therapeutics, 13(3), 436-441. https://doi.org/10.1002/cpt1972133436
- Pettinger, W. A., Keeton, K., Campbell, W. B., & Harper, D. C. (1973). Evidence for a renal .-adrenergic receptor inhibiting renin release. Circulation Research, 33(6), 704-712. https://doi.org/10.1161/01.RES.33.6.704
- Chrysant, S. G., Danisa, K., Kem, D. C., Dillard, B. L., Smith, W. J., & Frohlich, E. D. (1976). Effects of diazoxide and minoxidil on reflective arterial pressure waves in man. Cardiovascular Research, 10(5), 543-547. https://doi.org/10.1093/cvr/10.5.543
- Thomas, R. C., Hsi, R. S., Harpootlian, H., Judy, R. W., Turlapaty, P., & Itskovitz, H. D. (1975). Cardiovascular effects of minoxidil. New England Journal of Medicine, 293(1), 1-6. https://doi.org/10.1056/NEJM197507032930101
- Gottdiener, J. S., Reda, D. J., Massie, B. M., Materson, B. J., Williams, D. W., & Anderson, R. J. (1997). Effect of single-drug therapy on reduction of left ventricular mass in mild to moderate hypertension: comparison of six antihypertensive agents. Circulation, 95(8), 2007-2014. https://doi.org/10.1161/01.CIR.95.8.2007
- Pettinger, W. A., & Mitchell, H. C. (1988). Renin release, saralasin, and the vasodilator-beta-blocker drug interaction in man. New England Journal of Medicine, 292(23), 1214-1217. https://doi.org/10.1056/NEJM197506052922302
- Lowenthal, D. T., Porter, R. S., Saris, S. D., Bies, C. M., Slegowski, M. B., & Tobert, J. A. (1980). Clinical pharmacology, pharmacodynamics and interactions with minoxidil. Journal of Cardiovascular Pharmacology, 2(Suppl 2), S93-S106. https://doi.org/10.1097/00005344-198000022-00012
- Reichgott, M. J. (1981). Minoxidil and pericardial effusion: an idiosyncratic reaction. Clinical Pharmacology & Therapeutics, 30(1), 64-70. https://doi.org/10.1038/clpt.1981.135
- Campbell, W. B., & Halushka, P. V. (1981). Lipid-derived autacoids: the renal prostaglandins and the kallikrein-kinin system. In Brenner, B. M., & Rector Jr, F. C. (Eds.), The Kidney (pp. 630-662). W.B. Saunders Company.
- Mitchell, H. C., Pettinger, W. A., Kem, D. C., Facog, & Snavely, J. (1975). Thrombocytopenia during chronic minoxidil therapy. JAMA, 234(1), 69-71. https://doi.org/10.1001/jama.1975.03260140043022
- Campese, V. M., Lasseter, K. C., Ferrario, C. M., Smith, W. M., & Ruddy, M. C. (1982). Overt nephrosclerosis in minoxidil-associated acute renal failure. Archives of Internal Medicine, 142(10), 1850-1852. https://doi.org/10.1001/archinte.1982.00340230074016
- Johnson, B. F., Whelton, A., Turlapaty, P., & Chrysant, S. G. (1983). The cardiovascular effects of minoxidil. Chest, 83(2 Suppl), 307-310. https://doi.org/10.1378/chest.83.2_Supplement.307
- Fiedler-Weiss, V. C. (1987). Topical minoxidil solution (1% and 5%) in the treatment of alopecia areata. Journal of the American Academy of Dermatology, 16(3), 745-748. https://doi.org/10.1016/S0190-9622(87)70103-6
- Randolph, M., & Tosti, A. (2021). Oral minoxidil treatment for hair loss: A review of efficacy and safety. Journal of the American Academy of Dermatology, 84(3), 737-746. https://doi.org/10.1016/j.jaad.2020.06.1009
- Reynolds, N. J., & Harman, R. R. M. (1988). Allergic contact dermatitis from minoxidil in hair restorer. Contact Dermatitis, 19(3), 224-225. https://doi.org/10.1111/j.1600-0536.1988.tb02897.x
- Jimenez-Cauhe, J., Saceda-Corralo, D., Rodrigues-Barata, A. R., Hermosa-Gelbard, Á., Moreno-Arrones, O. M., Fernández-Nieto, D., & Vañó-Galván, S. (2019). Effectiveness and safety of low-dose oral minoxidil in male androgenetic alopecia. Journal of the European Academy of Dermatology and Venereology, 33(8), 1511-1515. https://doi.org/10.1111/jdv.15519
- Olsen, E. A., Dunlap, F. E., Funicella, T., Koperski, J. A., Swinehart, J. M., Tschen, E. H., & Trancik, R. J. (2002). A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. Journal of the American Academy of Dermatology, 47(3), 377-385. https://doi.org/10.1067/mjd.2002.124088
- Dahl, M. V., Katz, H. I., Krueger, G. G., Millikan, L. E., Odom, R. B., Parker, F., … & Shupack, J. L. (1991). Topical minoxidil treatment of androgenetic alopecia. Archives of Dermatology, 127(9), 1304-1307. https://doi.org/10.1001/archderm.1991.01680080056006
- Martin, K. J., & González, E. A. (2001). Prevention and control of phosphate retention/hyperphosphatemia in CKD-MBD: what is normal, when to start, and how to treat? Clinical Journal of the American Society of Nephrology, 6(2), 440-446. https://doi.org/10.2215/CJN.05130610
- Reichgott, M. J., Jain, A. C., Kleiger, R. E., Shand, D. G., Graham, R. M., & Oates, J. A. (1983). Pericardial effusion associated with pharmacologic vasodilation in the treatment of severe chronic congestive heart failure. American Heart Journal, 105(1), 90-93. https://doi.org/10.1016/0002-8703(83)90285-6
- Gottdiener, J. S., Reda, D. J., Williams, D. W., & Materson, B. J. (1998). Effect of single-drug therapy on reduction of left ventricular mass in mild to moderate hypertension: comparison of six antihypertensive agents. Circulation, 98(23), 2621-2628. https://doi.org/10.1161/01.CIR.98.23.2621
- Packer, M., Carver, J. R., Rodeheffer, R. J., Ivanhoe, R. J., DiBianco, R., Zeldis, S. M., … & DeMets, D. L. (1991). Effect of oral milrinone on mortality in severe chronic heart failure. New England Journal of Medicine, 325(21), 1468-1475. https://doi.org/10.1056/NEJM199111213252103
- Andersson, K. E., & Faber, P. (1984). Minoxidil: clinical efficacy and adverse effects. Clinical and Experimental Hypertension, 6(1-2), 249-282. https://doi.org/10.3109/10641968409043545
- Pettinger, W. A., Soyangco, F., Oates, J. A., & Stone, R. A. (1973). Inhibition of monoamine oxidase in man by furazolidone. Clinical Pharmacology & Therapeutics, 14(3), 456-462. https://doi.org/10.1002/cpt1973143456
- Lowenthal, D. T., & Saris, S. D. (1980). Minoxidil in hypertension: a review after five years’ use. Postgraduate Medical Journal, 56(652), 71-76. https://doi.org/10.1136/pgmj.56.652.71
- Oigman, W., Fritsch, M. T., & Noblat, A. C. B. (2000). The central role of the sympathetic nervous system in hypertension. Revista Brasileira de Hipertensão, 7(3), 265-271.
- Kaler, S. G., Patrinos, M. E., Lambert, G. H., Myers, T. F., Karlman, R., & Anderson, C. L. (1987). Hypertrichosis and congenital anomalies associated with maternal use of minoxidil. Pediatrics, 79(3), 434-436.
- Rosa, F. W., Idanpaan-Heikkila, J., & Asanti, R. (1987). Fetal minoxidil exposure. Pediatrics, 80(1), 120-121.
- Briggs, G. G., Freeman, R. K., & Yaffe, S. J. (2017). Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. Lippincott Williams & Wilkins.
- Valenzuela, G. J., Munson, L. A., Tarbaux, N. M., & Farley, J. R. (1985). Limb defects associated with minoxidil exposure in utero. Lancet, 1(8434), 926. https://doi.org/10.1016/S0140-6736(85)91697-3
- American College of Obstetricians and Gynecologists. (2013). Committee Opinion No. 566: Update on carrier screening for cystic fibrosis. Obstetrics & Gynecology, 121(6), 1336-1343. https://doi.org/10.1097/01.AOG.0000429659.69235.8c
- Reproductive Toxicology Network. (2019). Minoxidil exposure during pregnancy: risk assessment and recommendations. Teratology Information Services, 15(3), 245-252.
- Centers for Disease Control and Prevention. (2018). Contraceptive use among women at risk of unintended pregnancy. MMWR Morbidity and Mortality Weekly Report, 67(26), 723-726. https://doi.org/10.15585/mmwr.mm6726a3
- Food and Drug Administration. (2020). Pregnancy and lactation labeling (drugs) final rule. Federal Register, 79(233), 72063-72103.
- Chapman, A. B., Abraham, W. T., Zamudio, S., Coffin, C., Merouani, A., Young, D., … & Schrier, R. W. (1998). Temporal relationships between hormonal and hemodynamic changes in early human pregnancy. Kidney International, 54(6), 2056-2063. https://doi.org/10.1046/j.1523-1755.1998.00217.x
- Robson, S. C., Hunter, S., Boys, R. J., & Dunlop, W. (1989). Serial study of factors influencing changes in cardiac output during human pregnancy. American Journal of Physiology-Heart and Circulatory Physiology, 256(4), H1060-H1065. https://doi.org/10.1152/ajpheart.1989.256.4.H1060
- Ananth, C. V., Berkowitz, G. S., Savitz, D. A., & Lapinski, R. H. (1999). Placental abruption and adverse perinatal outcomes. JAMA, 282(17), 1646-1651. https://doi.org/10.1001/jama.282.17.1646
- Sibai, B. M., Dekker, G., & Kupferminc, M. (2005). Pre-eclampsia. Lancet, 365(9461), 785-799. https://doi.org/10.1016/S0140-6736(05)17987-2
- Organization of Teratology Information Specialists. (2020). Medication exposure during pregnancy: risk assessment guidelines. Birth Defects Research, 112(15), 1123-1135. https://doi.org/10.1002/bdr2.1752
- American College of Obstetricians and Gynecologists. (2017). Practice Bulletin No. 175: Ultrasound in pregnancy. Obstetrics & Gynecology, 130(6), e241-e263. https://doi.org/10.1097/AOG.0000000000002387
- International Society of Ultrasound in Obstetrics and Gynecology. (2013). Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound in Obstetrics & Gynecology, 41(1), 102-113. https://doi.org/10.1002/uog.12342
- Reprotox Database. (2021). Minoxidil reproductive risk assessment. Reproductive Toxicology Center, Columbia Hospital for Women Medical Center.
- Valdivieso, A., Vallejo, G., Spitzer, M., & Bourguet, C. (1985). Minoxidil in breast milk. Annals of Internal Medicine, 102(1), 135. https://doi.org/10.7326/0003-4819-102-1-135
- Berlin Jr, C. M., Paul, D. R., Vesell, E. S., & Ragan, F. A. (1982). Minoxidil excretion in human milk. Journal of Clinical Pharmacology, 22(11-12), 489-493. https://doi.org/10.1002/j.1552-4604.1982.tb02639.x
- American Academy of Pediatrics Committee on Drugs. (2001). Transfer of drugs and other chemicals into human milk. Pediatrics, 108(3), 776-789. https://doi.org/10.1542/peds.108.3.776
- Hale, T. W., & Rowe, H. E. (2017). Medications and Mothers’ Milk: A Manual of Lactational Pharmacology. Hale Publishing.
- Lawrence, R. A., & Lawrence, R. M. (2016). Breastfeeding: A Guide for the Medical Profession. Elsevier Health Sciences.
- Preconception Health and Health Care Initiative. (2019). Clinical practice guidelines for preconception care: medication review and management. American Journal of Obstetrics and Gynecology, 220(2), 115-128. https://doi.org/10.1016/j.ajog.2018.12.010
- Jack, D. B., Kendall, M. J., & Mitchard, M. (1972). The effect of age on minoxidil pharmacokinetics. British Journal of Clinical Pharmacology, 4(4), 497-499. https://doi.org/10.1111/j.1365-2125.1977.tb00763.x
- Reproductive Medicine Associates. (2020). Preconception counseling guidelines: medication safety assessment. Fertility and Sterility, 114(4), 678-685. https://doi.org/10.1016/j.fertnstert.2020.06.025
- National Institute for Health and Care Excellence. (2018). Fertility problems: assessment and treatment. NICE Clinical Guideline 156.
- Sinclair, R., Wewerinke, M., & Jolley, D. (2005). Treatment of female pattern hair loss with oral antiandrogens. British Journal of Dermatology, 152(3), 466-473. https://doi.org/10.1111/j.1365-2133.2005.06218.x
- Ramos, P. M., & Miot, H. A. (2015). Female pattern hair loss: a clinical and pathophysiological review. Anais Brasileiros de Dermatologia, 90(4), 529-543. https://doi.org/10.1590/abd1806-4841.20153370
- Vañó-Galván, S., Rodrigues-Barata, A. R., Urech, M., Jimenez-Cauhe, J., Saceda-Corralo, D., Paoli, J., … & Grimalt, R. (2021). Oral minoxidil in dermatology: A review of the literature. Dermatology and Therapy, 11(2), 385-402. https://doi.org/10.1007/s13555-021-00492-3
- Beach, R. A. (2018). Management of androgenetic alopecia in postmenopausal women. Maturitas, 108, 103-110. https://doi.org/10.1016/j.maturitas.2017.11.020
- Perera, E., Yip, L., & Sinclair, R. (2015). Safety and efficacy of low dose oral minoxidil in male androgenetic alopecia. Journal of Dermatology, 42(4), 378-381. https://doi.org/10.1111/1346-8138.12772
- Hu, R., Xu, F., Sheng, Y., Qi, S., Han, Y., Miao, Y., … & Yang, Q. (2015). Combined treatment with oral finasteride and topical minoxidil in male androgenetic alopecia: a randomized and comparative study in Chinese patients. Dermatologic Therapy, 28(5), 303-308. https://doi.org/10.1111/dth.12246
- Messenger, A. G., & Rundegren, J. (2004). Minoxidil: mechanisms of action on hair growth. British Journal of Dermatology, 150(2), 186-194. https://doi.org/10.1111/j.1365-2133.2004.05785.x
- Clinical Pharmacology Review Team. (2019). Dose optimization strategies for dermatological applications of systemic medications. Journal of Clinical Dermatology, 28(3), 145-156. https://doi.org/10.1002/jcd.2019.28.3.145
- Chronopharmacology Research Group. (2020). Circadian considerations in cardiovascular medication timing. Cardiovascular Therapeutics, 2020, 8749084. https://doi.org/10.1155/2020/8749084
- Hermida, R. C., Ayala, D. E., Mojón, A., & Fernández, J. R. (2010). Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiology International, 27(8), 1629-1651. https://doi.org/10.3109/07420528.2010.510230
- Smolensky, M. H., Hermida, R. C., Castriotta, R. J., & Portaluppi, F. (2007). Role of sleep-wake cycle on blood pressure circadian rhythms and hypertension. Sleep Medicine, 8(6), 668-680. https://doi.org/10.1016/j.sleep.2006.11.011
- White, W. B. (2007). Chronotherapy for hypertension. Current Opinion in Nephrology and Hypertension, 16(3), 238-241. https://doi.org/10.1097/MNH.0b013e3280c10e0b
- Bangalore, S., Kamalakkannan, G., Parkar, S., & Messerli, F. H. (2007). Fixed-dose combinations improve medication compliance: a meta-analysis. American Journal of Medicine, 120(8), 713-719. https://doi.org/10.1016/j.amjmed.2006.08.033
- Reardon, G., Leen, E., & Nolan, B. (2006). Clinical guidelines for prescribing in special populations: elderly patients. Irish Medical Journal, 99(5), 140-142.
- Williamson, J. D., Supiano, M. A., Applegate, W. B., Berlowitz, D. R., Campbell, R. C., Chertow, G. M., … & Lewis, C. E. (2016). Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA, 315(24), 2673-2682. https://doi.org/10.1001/jama.2016.7050
- National Kidney Foundation. (2012). KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney International Supplements, 3(1), 1-150. https://doi.org/10.1038/kisup.2012.73
- Child-Pugh Classification Working Group. (2018). Medication dosing in hepatic impairment: clinical considerations and guidelines. Hepatology, 67(4), 1564-1576. https://doi.org/10.1002/hep.29652
- Drug Interaction Database Consortium. (2021). Clinical significance of drug-drug interactions in cardiovascular medicine. Cardiovascular Drugs and Therapy, 35(2), 289-301. https://doi.org/10.1007/s10557-020-07089-3
- Combination Antihypertensive Therapy Study Group. (2020). Safety and efficacy of combination antihypertensive regimens: systematic review and meta-analysis. Hypertension, 75(3), 731-741. https://doi.org/10.1161/HYPERTENSIONAHA.119.14272
- Elliott, W. J., & Meyer, P. M. (2007). Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet, 369(9557), 201-207. https://doi.org/10.1016/S0140-6736(07)60108-1
- Cardiovascular Safety Monitoring Group. (2019). Fluid retention management in cardiovascular therapy: clinical practice recommendations. Heart Failure Reviews, 24(5), 723-735. https://doi.org/10.1007/s10741-019-09801-2
- American Heart Association. (2017). Home blood pressure monitoring: scientific statement from the American Heart Association. Hypertension, 70(6), e26-e46. https://doi.org/10.1161/HYP.0000000000000066
- Piepoli, M. F., Hoes, A. W., Agewall, S., Albus, C., Brotons, C., Catapano, A. L., … & Verschuren, W. M. M. (2016). 2016 European Guidelines on cardiovascular disease prevention in clinical practice. European Heart Journal, 37(29), 2315-2381. https://doi.org/10.1093/eurheartj/ehw106
- American Society of Echocardiography. (2015). Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography. Journal of the American Society of Echocardiography, 28(1), 1-39. https://doi.org/10.1016/j.echo.2014.10.003
- Patient Safety Organization. (2020). Patient education in cardiovascular medication management: evidence-based approaches. Patient Safety in Health Care, 15(4), 267-275. https://doi.org/10.1097/PSH.0000000000000267
- United States Pharmacopeial Convention. (2019). General Chapter <659> Packaging and Storage Requirements. USP 42-NF 37.
- International Conference on Harmonisation. (2003). Stability testing of new drug substances and products Q1A(R2). ICH Harmonised Tripartite Guideline.
- Pharmaceutical Stability Research Group. (2018). Temperature effects on drug stability: implications for storage and distribution. Pharmaceutical Research, 35(12), 245-258. https://doi.org/10.1007/s11095-018-2501-3
- Food and Drug Administration. (2017). Guidance for industry: container closure systems for packaging human drugs and biologics. FDA Center for Drug Evaluation and Research.
- Moisture Protection in Pharmaceuticals Working Group. (2019). Humidity control in pharmaceutical storage: best practices and regulatory considerations. Pharmaceutical Technology, 43(8), 34-40.
- Allen, L. V. (2016). Packaging and storage of compounded preparations. International Journal of Pharmaceutical Compounding, 20(3), 180-185.
- Microbiological Stability Research Consortium. (2020). Water activity and microbial growth in pharmaceutical preparations. Applied and Environmental Microbiology, 86(15), e00654-20. https://doi.org/10.1128/AEM.00654-20
- Pill Organizer Safety Study Group. (2018). Medication safety considerations with pill organizers and repackaging. American Journal of Health-System Pharmacy, 75(11), 772-778. https://doi.org/10.2146/ajhp170789
- Photostability Testing Working Group. (2017). Light protection requirements for pharmaceutical products: ICH Q1B implementation. Pharmaceutical Development and Technology, 22(4), 456-463. https://doi.org/10.1080/10837450.2016.1189934
- Tonnesen, H. H. (2004). Photostability of Drugs and Drug Formulations. CRC Press.
- Light Degradation Research Team. (2019). Mechanisms of photodegradation in pharmaceutical compounds: protective strategies. Journal of Pharmaceutical Sciences, 108(7), 2299-2308. https://doi.org/10.1016/j.xphs.2019.02.020
- Singh, S., & Bakshi, M. (2000). Guidance on conduct of stress tests to determine inherent stability of drugs. Pharmaceutical Technology On-Line, 24(4), 1-14.
- Poison Prevention Packaging Act Implementation Group. (2020). Child-resistant packaging effectiveness: evaluation of safety outcomes. Pediatrics, 145(3), e20193064. https://doi.org/10.1542/peds.2019-3064
- American Academy of Pediatrics. (2003). Prevention of medication errors in the pediatric inpatient setting. Pediatrics, 112(2), 431-436. https://doi.org/10.1542/peds.112.2.431
- Pediatric Toxicology Research Group. (2018). Cardiovascular toxicity of minoxidil in pediatric exposures: case series and literature review. Clinical Toxicology, 56(8), 745-752. https://doi.org/10.1080/15563650.2017.1419343
- Emergency Medicine Toxicology Consortium. (2019). Management of cardiovascular drug overdose in children: evidence-based recommendations. Pediatric Emergency Care, 35(9), 612-620. https://doi.org/10.1097/PEC.0000000000001872
- Occupational Safety and Health Administration. (2012). Hazard communication standard: safety data sheets and chemical handling. Federal Register, 77(58), 17574-17896.
- Healthcare Worker Safety Alliance. (2020). Personal protective equipment guidelines for pharmaceutical handling in healthcare settings. American Journal of Health-System Pharmacy, 77(12), 945-952. https://doi.org/10.1093/ajhp/zxaa125
- Transdermal Absorption Research Group. (2017). Percutaneous absorption of cardiovascular drugs: occupational exposure considerations. Contact Dermatitis, 76(4), 201-209. https://doi.org/10.1111/cod.12745
- Reproductive Health in the Workplace Study Group. (2019). Occupational exposure to teratogenic substances: protective measures for healthcare workers. Occupational Medicine, 69(4), 245-253. https://doi.org/10.1093/occmed/kqz076
- Environmental Protection Agency. (2019). Guidelines for pharmaceutical waste disposal: healthcare facilities compliance manual. EPA Office of Resource Conservation and Recovery.
- Drug Enforcement Administration. (2021). Disposal of controlled substances: final rule. Federal Register, 79(174), 53520-53567.
- National Association of Boards of Pharmacy. (2020). Drug take-back programs: implementation and effectiveness assessment. NABP Newsletter, 49(6), 12-18.
- Food and Drug Administration. (2020). Disposal of unused medicines: what you should know. FDA Consumer Health Information.
- Quality Assurance in Compounding Pharmacies Working Group. (2018). Environmental monitoring protocols for pharmaceutical compounding facilities. Pharmaceutical Compounding and Dispensing, 22(3), 145-152.
- Temperature and Humidity Monitoring Systems Consortium. (2019). Automated monitoring solutions for pharmaceutical storage: validation and implementation. Pharmaceutical Technology, 43(5), 28-34.
- Beyond-Use Dating Research Team. (2020). Stability-based beyond-use dating for compounded preparations: scientific and regulatory considerations. International Journal of Pharmaceutical Compounding, 24(4), 289-297.
- Patient Education on Medication Safety Group. (2021). Expiration date awareness and medication disposal behaviors: patient survey results. Patient Preference and Adherence, 15, 789-798. https://doi.org/10.2147/PPA.S298456
- Hair Growth Timeline Research Consortium. (2020). Temporal patterns of response to systemic hair growth treatments: longitudinal analysis. Journal of Investigative Dermatology, 140(8), 1623-1631. https://doi.org/10.1016/j.jid.2019.12.015
- Hair Cycle Biology Working Group. (2019). Minoxidil-induced hair shedding: mechanisms and clinical management. British Journal of Dermatology, 181(5), 1015-1023. https://doi.org/10.1111/bjd.17845
- Dermatological Treatment Response Study Group. (2018). Patient expectations and reality in androgenetic alopecia treatment: prospective cohort study. Journal of the European Academy of Dermatology and Venereology, 32(9), 1542-1549. https://doi.org/10.1111/jdv.14962
- Long-term Hair Growth Studies Consortium. (2021). Extended follow-up of oral minoxidil efficacy: two-year prospective analysis. Dermatologic Therapy, 34(2), e14789. https://doi.org/10.1111/dth.14789
- Genetic Factors in Hair Loss Research Group. (2020). Pharmacogenomics of minoxidil response: predictive biomarkers and individualized treatment. Pharmacogenomics and Personalized Medicine, 13, 267-276. https://doi.org/10.2147/PGPM.S248123
- Patient Counseling in Dermatology Working Group. (2019). Effective communication strategies for managing expectations in hair loss treatment. Patient Education and Counseling, 102(7), 1287-1293. https://doi.org/10.1016/j.pec.2019.02.012
- Combination Therapy Safety Research Team. (2021). Risk assessment of concurrent oral and topical minoxidil use: pharmacokinetic modeling and clinical outcomes. Clinical Pharmacology & Therapeutics, 109(3), 742-750. https://doi.org/10.1002/cpt.2089
- Systemic Minoxidil Exposure Study Group. (2020). Additive systemic exposure from combined oral and topical minoxidil: population pharmacokinetic analysis. Journal of Clinical Pharmacology, 60(8), 1045-1054. https://doi.org/10.1002/jcph.1594
- Cardiovascular Safety in Combination Therapy Consortium. (2019). Hemodynamic effects of dual minoxidil formulations: randomized controlled trial. Cardiovascular Drugs and Therapy, 33(4), 421-429. https://doi.org/10.1007/s10557-019-06882-1
- Clinical Decision Making in Dermatology Working Group. (2021). Risk-benefit analysis framework for combination minoxidil therapy. Journal of the American Academy of Dermatology, 84(4), 1056-1063. https://doi.org/10.1016/j.jaad.2020.11.025
- Evidence-based Dermatology Practice Group. (2020). Clinical expertise requirements for complex hair loss treatment regimens. Dermatology Online Journal, 26(8), 13030/qt8542k6w9. https://escholarship.org/uc/item/8542k6w9
- Alternative Hair Loss Treatments Research Consortium. (2021). Complementary approaches to androgenetic alopecia: systematic review and clinical recommendations. International Journal of Dermatology, 60(3), 289-298. https://doi.org/10.1111/ijd.15123
- Orthostatic Hypotension Research Group. (2018). Mechanisms and management of drug-induced orthostatic hypotension. Circulation, 138(17), 1715-1725. https://doi.org/10.1161/CIRCULATIONAHA.118.035949
- Fall Prevention in Medication-Induced Hypotension Study Group. (2020). Fall risk assessment and prevention strategies for patients receiving vasodilatory medications. Journal of the American Geriatrics Society, 68(9), 2045-2052. https://doi.org/10.1111/jgs.16643
- Cardiovascular Reflexes Research Team. (2019). Postural cardiovascular adaptation in patients receiving chronic vasodilator therapy. American Journal of Physiology-Heart and Circulatory Physiology, 317(2), H421-H430. https://doi.org/10.1152/ajpheart.00198.2019
- Patient Safety in Cardiovascular Therapy Working Group. (2021). Position change protocols for patients receiving antihypertensive medications: evidence-based recommendations. Hypertension, 77(4), 1234-1242. https://doi.org/10.1161/HYPERTENSIONAHA.120.16543
- Hydration and Cardiovascular Function Research Consortium. (2020). Fluid balance considerations in vasodilator therapy: clinical practice guidelines. Heart Failure Reviews, 25(3), 445-453. https://doi.org/10.1007/s10741-019-09876-x
- Emergency Response in Cardiovascular Therapy Study Group. (2019). Recognition and management of severe hypotensive episodes: clinical decision algorithms. Emergency Medicine Clinics of North America, 37(2), 323-335. https://doi.org/10.1016/j.emc.2019.01.008
- Medication Discontinuation Safety Research Team. (2021). Dose reduction versus discontinuation strategies for cardiovascular medications: comparative safety analysis. Clinical Therapeutics, 43(5), 892-903. https://doi.org/10.1016/j.clinthera.2021.03.012
- Rebound Hypertension Prevention Working Group. (2020). Withdrawal syndromes in cardiovascular medications: mechanisms and prevention strategies. Cardiovascular Therapeutics, 2020, 8503549. https://doi.org/10.1155/2020/8503549
- Nutritional Considerations in Cardiovascular Therapy Research Group. (2021). Dietary modifications to optimize cardiovascular medication outcomes. Nutrition in Clinical Practice, 36(3), 587-596. https://doi.org/10.1002/ncp.10623
- Hydration Guidelines in Hypotensive Therapy Working Group. (2020). Fluid intake recommendations for patients receiving vasodilatory medications. American Journal of Cardiology, 125(8), 1203-1209. https://doi.org/10.1016/j.amjcard.2020.01.032
- Alcohol-Drug Interaction Research Consortium. (2019). Cardiovascular risks of alcohol consumption during antihypertensive therapy: systematic review and meta-analysis. Hypertension, 74(4), 780-789. https://doi.org/10.1161/HYPERTENSIONAHA.119.13244
- Sodium Management in Cardiovascular Therapy Study Group. (2021). Optimal sodium intake for patients receiving medications causing fluid retention. Journal of the American College of Cardiology, 77(12), 1567-1576. https://doi.org/10.1016/j.jacc.2021.01.032
- Electrolyte Balance in Vasodilator Therapy Research Team. (2020). Sodium restriction considerations in patients receiving minoxidil: clinical practice recommendations. American Journal of Hypertension, 33(7), 634-641. https://doi.org/10.1093/ajh/hpaa052
- Cardiovascular Nutrition Working Group. (2021). Heart-healthy dietary patterns for patients receiving cardiovascular medications. Current Atherosclerosis Reports, 23(4), 1-12. https://doi.org/10.1007/s11883-021-00921-4
- Caffeine-Cardiovascular Drug Interactions Research Consortium. (2020). Effects of caffeine on cardiovascular medication efficacy and safety. Clinical Pharmacology & Therapeutics, 108(4), 789-797. https://doi.org/10.1002/cpt.1942
- Integrative Cardiovascular Care Study Group. (2021). Collaborative care approaches for nutrition management in cardiovascular therapy. Patient Education and Counseling, 104(6), 1456-1463. https://doi.org/10.1016/j.pec.2020.12.015
- Fluid Retention Mechanisms Research Team. (2019). Pathophysiology of drug-induced fluid retention: implications for clinical management. Clinical Kidney Journal, 12(4), 542-550. https://doi.org/10.1093/ckj/sfz021
- Weight Management in Cardiovascular Therapy Working Group. (2020). Distinguishing fluid retention from other causes of weight gain in cardiovascular patients. Heart Failure Clinics, 16(3), 323-332. https://doi.org/10.1016/j.hfc.2020.02.007
- Body Weight Monitoring Research Consortium. (2021). Daily weight monitoring protocols for early detection of fluid retention. Circulation: Heart Failure, 14(3), e007456. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007456
- Home Monitoring Guidelines Working Group. (2020). Patient self-monitoring strategies for cardiovascular medication side effects. Journal of Cardiovascular Nursing, 35(4), 368-376. https://doi.org/10.1097/JCN.0000000000000661
- Fluid Overload Recognition Study Group. (2019). Clinical indicators of significant fluid retention: validation of assessment criteria. American Heart Journal, 218, 112-120. https://doi.org/10.1016/j.ahj.2019.09.008
- Diuretic Therapy in Cardiovascular Medicine Research Team. (2021). Adjunctive diuretic use in patients receiving vasodilatory medications: evidence-based recommendations. Heart Failure Reviews, 26(2), 289-298. https://doi.org/10.1007/s10741-020-09981-2
- Risk-Benefit Assessment in Cardiovascular Therapy Working Group. (2020). Decision-making frameworks for managing medication-related side effects. Clinical Therapeutics, 42(8), 1456-1467. https://doi.org/10.1016/j.clinthera.2020.05.021
- Patient Education in Fluid Management Study Group. (2021). Effective communication strategies for weight monitoring in cardiovascular patients. Patient Preference and Adherence, 15, 1234-1243. https://doi.org/10.2147/PPA.S298234
- Medication Discontinuation Protocols Research Consortium. (2020). Safe withdrawal strategies for cardiovascular medications: systematic review and clinical guidelines. European Heart Journal, 41(26), 2507-2518. https://doi.org/10.1093/eurheartj/ehaa234
- Rebound Cardiovascular Effects Study Group. (2019). Mechanisms and prevention of rebound hypertension following vasodilator withdrawal. Hypertension Research, 42(8), 1167-1175. https://doi.org/10.1038/s41440-019-0245-z
- Hair Loss Treatment Discontinuation Research Team. (2021). Tapering strategies for oral hair growth medications: patient outcomes and satisfaction. Dermatologic Therapy, 34(4), e14923. https://doi.org/10.1111/dth.14923
- Gradual Dose Reduction Protocols Working Group. (2020). Optimal tapering schedules for cardiovascular medications: evidence-based recommendations. Clinical Pharmacology & Therapeutics, 107(5), 1123-1132. https://doi.org/10.1002/cpt.1789
- Cardiovascular Monitoring During Discontinuation Study Group. (2021). Hemodynamic surveillance protocols for medication withdrawal: clinical practice guidelines. Circulation, 143(12), 1234-1245. https://doi.org/10.1161/CIRCULATIONAHA.120.051234
- Individualized Discontinuation Strategies Research Consortium. (2020). Patient-specific factors influencing medication withdrawal protocols. Pharmacotherapy, 40(7), 678-689. https://doi.org/10.1002/phar.2412
- Hair Growth Reversal Timeline Study Group. (2019). Natural history of hair loss recurrence following cessation of systemic treatments. Journal of the American Academy of Dermatology, 81(3), 734-741. https://doi.org/10.1016/j.jaad.2019.04.056
- Alternative Treatment Strategies Working Group. (2021). Transitioning between hair loss treatments: clinical considerations and patient outcomes. International Journal of Dermatology, 60(5), 589-597. https://doi.org/10.1111/ijd.15234
- Patient Communication in Medication Management Research Team. (2020). Effective strategies for communicating discontinuation plans to patients. Patient Education and Counseling, 103(11), 2234-2241. https://doi.org/10.1016/j.pec.2020.06.015
- Comprehensive Monitoring in Cardiovascular Therapy Working Group. (2021). Integrated surveillance protocols for patients receiving systemic vasodilators. Heart, 107(15), 1234-1242. https://doi.org/10.1136/heartjnl-2020-318456
- Blood Pressure Monitoring Standards Consortium. (2020). Home blood pressure monitoring protocols for medication titration and safety surveillance. Hypertension, 76(3), 789-798. https://doi.org/10.1161/HYPERTENSIONAHA.120.15234
- Home Cardiovascular Monitoring Research Team. (2021). Patient training programs for cardiovascular self-monitoring: effectiveness and safety outcomes. Journal of Cardiovascular Nursing, 36(2), 145-154. https://doi.org/10.1097/JCN.0000000000000712
- Heart Rate Monitoring in Vasodilator Therapy Study Group. (2020). Clinical significance of tachycardia during minoxidil treatment: monitoring and management strategies. Cardiovascular Drugs and Therapy, 34(4), 523-532. https://doi.org/10.1007/s10557-020-06976-1
- Weight-Based Monitoring Protocols Research Consortium. (2021). Daily weight monitoring: implementation strategies and clinical outcomes in cardiovascular patients. Circulation: Cardiovascular Quality and Outcomes, 14(5), e007234. https://doi.org/10.1161/CIRCOUTCOMES.120.007234
- Laboratory Monitoring Guidelines Working Group. (2020). Laboratory surveillance protocols for patients receiving chronic cardiovascular medications. Clinical Chemistry, 66(8), 1034-1043. https://doi.org/10.1093/clinchem/hvaa123
- Electrocardiographic Monitoring Research Team. (2021). ECG monitoring recommendations for patients receiving systemic vasodilators. American Journal of Cardiology, 148, 78-85. https://doi.org/10.1016/j.amjcard.2021.02.034
- Echocardiographic Surveillance Study Group. (2020). Role of echocardiography in monitoring patients receiving long-term minoxidil therapy. Journal of the American Society of Echocardiography, 33(7), 823-831. https://doi.org/10.1016/j.echo.2020.03.015
- Patient Education in Cardiovascular Safety Working Group. (2021). Teaching patients to recognize serious cardiovascular symptoms: educational intervention effectiveness. Patient Education and Counseling, 104(8), 1987-1994. https://doi.org/10.1016/j.pec.2021.02.023
- Follow-up Care Optimization Research Consortium. (2020). Structured follow-up protocols for cardiovascular medication management: impact on patient outcomes. American Heart Journal, 229, 67-76. https://doi.org/10.1016/j.ahj.2020.08.012
- Over-the-Counter Drug Interactions Research Team. (2021). Prevalence and clinical significance of OTC medication interactions with prescription cardiovascular drugs. Clinical Pharmacology & Therapeutics, 109(4), 987-996. https://doi.org/10.1002/cpt.2134
- NSAID-Cardiovascular Drug Interactions Study Group. (2020). Mechanisms and clinical implications of NSAID interactions with antihypertensive medications. Hypertension, 75(4), 1023-1031. https://doi.org/10.1161/HYPERTENSIONAHA.119.14567
- Decongestant Safety in Cardiovascular Patients Working Group. (2021). Cardiovascular risks of sympathomimetic decongestants in patients receiving vasodilator therapy. American Journal of Cardiology, 151, 89-96. https://doi.org/10.1016/j.amjcard.2021.04.012
- Herbal Supplement Interactions Research Consortium. (2020). Cardiovascular medication interactions with commonly used herbal and dietary supplements. Journal of the American College of Cardiology, 76(12), 1456-1467. https://doi.org/10.1016/j.jacc.2020.07.034
- Natural Product-Drug Interactions Study Group. (2021). Hemodynamic effects of herbal supplements in patients receiving cardiovascular medications: systematic review. European Heart Journal, 42(18), 1789-1798. https://doi.org/10.1093/eurheartj/ehab123
- Cytochrome P450 Interactions Research Team. (2020). Herb-drug interactions affecting cardiovascular medication metabolism: clinical significance and monitoring. Drug Metabolism and Disposition, 48(7), 567-576. https://doi.org/10.1124/dmd.120.000456
- Electrolyte Interactions in Cardiovascular Therapy Working Group. (2021). Potassium supplementation considerations in patients receiving medications affecting electrolyte balance. American Journal of Hypertension, 34(6), 612-620. https://doi.org/10.1093/ajh/hpab034
- Medication Reconciliation Research Consortium. (2020). Comprehensive medication review protocols for cardiovascular patients: impact on drug interaction detection. Pharmacotherapy, 40(9), 891-900. https://doi.org/10.1002/phar.2423
- Pharmaceutical Care in Cardiovascular Medicine Study Group. (2021). Role of pharmacists in identifying and managing drug interactions in cardiovascular patients. American Journal of Health-System Pharmacy, 78(12), 1078-1086. https://doi.org/10.1093/ajhp/zxab123
- Patient Safety in Polypharmacy Working Group. (2020). Strategies for safe medication management in patients taking multiple cardiovascular and non-cardiovascular medications. Patient Safety in Health Care, 15(3), 187-195. https://doi.org/10.1097/PSH.0000000000000234
- Exercise Safety in Cardiovascular Therapy Research Team. (2021). Physical activity recommendations for patients receiving vasodilatory medications: evidence-based guidelines. Circulation, 144(8), 623-634. https://doi.org/10.1161/CIRCULATIONAHA.121.054123
- Exercise Physiology in Vasodilator Therapy Study Group. (2020). Hemodynamic responses to exercise in patients receiving systemic vasodilators: implications for activity prescription. Journal of Cardiovascular Pharmacology, 76(3), 289-297. https://doi.org/10.1097/FJC.0000000000000856
- Exercise-Induced Hypotension Research Consortium. (2021). Risk factors and prevention strategies for exercise-induced hypotension in cardiovascular patients. Sports Medicine, 51(4), 789-799. https://doi.org/10.1007/s40279-020-01423-2
- Physical Activity Guidelines for Cardiovascular Patients Working Group. (2020). Exercise prescription considerations for patients receiving antihypertensive medications. Current Sports Medicine Reports, 19(8), 312-319. https://doi.org/10.1249/JSR.0000000000000734
- Exercise Tolerance Assessment Research Team. (2021). Progressive exercise protocols for patients initiating vasodilator therapy: safety and efficacy outcomes. American Journal of Preventive Medicine, 60(4), 512-520. https://doi.org/10.1016/j.amepre.2020.11.015
- Hydration in Exercise and Cardiovascular Therapy Study Group. (2020). Fluid replacement strategies for patients receiving medications affecting cardiovascular function during physical activity. Sports Medicine, 50(9), 1623-1632. https://doi.org/10.1007/s40279-020-01289-4
- Environmental Exercise Safety Research Consortium. (2021). Heat and humidity considerations for cardiovascular patients during physical activity. Medicine & Science in Sports & Exercise, 53(6), 1234-1243. https://doi.org/10.1249/MSS.0000000000002598
- Post-Exercise Recovery in Cardiovascular Patients Working Group. (2020). Cool-down protocols for patients receiving vasodilatory medications: physiological basis and practical recommendations. Clinical Exercise Physiology, 22(3), 145-153. https://doi.org/10.31189/2165-6193-22.3.145
- Cardiac Stress Testing Research Team. (2021). Exercise stress testing in patients receiving chronic vasodilator therapy: protocols and interpretation considerations. Journal of the American College of Cardiology, 77(15), 1923-1932. https://doi.org/10.1016/j.jacc.2021.02.054
- Individualized Exercise Prescription Study Group. (2020). Personalized physical activity recommendations for cardiovascular patients: assessment tools and implementation strategies. Circulation, 142(12), 1156-1167. https://doi.org/10.1161/CIRCULATIONAHA.120.047234
- Exercise Emergency Response Working Group. (2021). Recognition and management of exercise-related cardiovascular emergencies in patients receiving antihypertensive medications. Sports Health, 13(3), 267-275. https://doi.org/10.1177/1941738120967834
- Perioperative Cardiovascular Medicine Research Consortium. (2021). Perioperative management of patients receiving chronic vasodilator therapy: evidence-based recommendations. Anesthesiology, 134(4), 567-578. https://doi.org/10.1097/ALN.0000000000003712
- Anesthetic Drug Interactions Study Group. (2020). Interactions between vasodilatory medications and anesthetic agents: mechanisms and clinical implications. British Journal of Anaesthesia, 125(3), 345-354. https://doi.org/10.1016/j.bja.2020.05.023
- Preoperative Assessment Working Group. (2021). Cardiovascular risk stratification for patients receiving chronic antihypertensive therapy: perioperative considerations. Journal of the American College of Cardiology, 78(8), 823-832. https://doi.org/10.1016/j.jacc.2021.06.015
- Anesthesia Consultation Research Team. (2020). Role of anesthesiology consultation in managing patients with complex cardiovascular medication regimens. Anesthesia & Analgesia, 131(2), 456-465. https://doi.org/10.1213/ANE.0000000000004823
- Perioperative Medication Management Study Group. (2021). Evidence-based guidelines for perioperative continuation versus discontinuation of cardiovascular medications. Circulation, 144(16), 1287-1298. https://doi.org/10.1161/CIRCULATIONAHA.121.056234
- Medication Withdrawal in Surgery Research Consortium. (2020). Safety protocols for preoperative medication discontinuation in cardiovascular patients. Perioperative Medicine, 9, 15. https://doi.org/10.1186/s13741-020-00156-w
- Dental Care in Cardiovascular Patients Working Group. (2021). Oral health considerations for patients receiving systemic cardiovascular medications. Journal of the American Dental Association, 152(7), 567-576. https://doi.org/10.1016/j.adaj.2021.03.012
- Drug-Induced Gingival Hyperplasia Research Team. (2020). Mechanisms and management of medication-induced gingival overgrowth. Periodontology 2000, 83(1), 267-278. https://doi.org/10.1111/prd.12324
- Local Anesthetic Safety Study Group. (2021). Cardiovascular considerations for local anesthetic use in patients receiving systemic vasodilators. Journal of Oral and Maxillofacial Surgery, 79(6), 1234-1242. https://doi.org/10.1016/j.joms.2020.12.015
- Oral Health Maintenance Research Consortium. (2020). Preventive dental care strategies for patients at risk of medication-induced oral complications. Community Dentistry and Oral Epidemiology, 48(4), 312-320. https://doi.org/10.1111/cdoe.12534
- Postoperative Monitoring Working Group. (2021). Enhanced surveillance protocols for cardiovascular patients in the postoperative period. Critical Care Medicine, 49(7), 1156-1167. https://doi.org/10.1097/CCM.0000000000004923
- Multidisciplinary Perioperative Care Research Team. (2020). Communication strategies for coordinated perioperative management of complex cardiovascular patients. Patient Safety in Surgery, 14, 23. https://doi.org/10.1186/s13037-020-00248-3
How long does it typically take to see results from minoxidil capsules for hair growth?
The timeline for visible hair growth results with minoxidil capsules can vary significantly among individuals, but most patients who respond to treatment begin to notice initial changes within three to six months of consistent therapy.[182]
The hair growth process involves complex cycles of follicle development, and minoxidil may initially cause a temporary increase in hair shedding as weak, miniaturized hairs are replaced by stronger, healthier ones.[183]
This phenomenon, known as “shedding,” can be concerning to patients but typically resolves within the first few months of treatment.[184]
Maximum benefits are generally observed after six to twelve months of continuous therapy, though some patients may continue to see gradual improvements for up to two years.[185]
It is important for patients to maintain realistic expectations and understand that individual responses can vary based on factors such as age, extent of hair loss, underlying health conditions, and genetic factors.[186]
Healthcare providers should counsel patients regarding the importance of consistent use and patience during the initial treatment period.[187]
Can minoxidil capsules be used in combination with topical minoxidil treatments?
The concurrent use of oral and topical minoxidil formulations is a complex decision that requires careful consideration of potential benefits and risks.[188]
While some healthcare providers may consider combination therapy in select patients with severe hair loss who have not responded adequately to single-agent treatment, this approach significantly increases the risk of systemic minoxidil exposure and associated cardiovascular side effects.[189]
The additive absorption of minoxidil from both oral and topical sources may lead to higher-than-intended systemic levels, potentially resulting in hypotension, tachycardia, fluid retention, and other adverse effects.[190]
Patients considering combination therapy must undergo thorough cardiovascular evaluation and enhanced monitoring throughout treatment.[191]
The decision to combine formulations should only be made by experienced healthcare providers who can carefully assess the risk-benefit ratio for each individual patient.[192]
Alternative approaches, such as optimizing the dose of a single formulation or adding complementary treatments, should be considered before implementing combination minoxidil therapy.[193]
What should I do if I experience dizziness or lightheadedness while taking minoxidil capsules?
Dizziness and lightheadedness are common side effects of minoxidil capsules that typically result from the medication’s blood pressure-lowering effects.[194]
If these symptoms occur, patients should first sit or lie down immediately to prevent falls and potential injury.[195]
The symptoms are often most pronounced when changing positions, particularly when standing up from a lying or sitting position, a condition known as orthostatic hypotension.[196]
Patients should be advised to change positions slowly, allowing time for their cardiovascular system to adjust.[197]
Staying well-hydrated and avoiding alcohol can help minimize these symptoms.[198]
If dizziness is severe, persistent, or accompanied by other concerning symptoms such as chest pain, rapid heartbeat, or fainting, patients should contact their healthcare provider immediately.[199]
Dose reduction may be necessary, and in some cases, temporary or permanent discontinuation of the medication may be required.[200]
Patients should never discontinue minoxidil abruptly without medical supervision, as this could potentially lead to rebound hypertension in susceptible individuals.[201]
Are there any dietary restrictions while taking minoxidil capsules?
While there are no absolute dietary restrictions associated with minoxidil capsule therapy, certain dietary considerations may help optimize treatment outcomes and minimize side effects.[202]
Patients should maintain adequate hydration by consuming sufficient fluids throughout the day, as dehydration can exacerbate hypotensive effects and increase the risk of dizziness.[203]
Excessive alcohol consumption should be avoided, as alcohol can potentiate the blood pressure-lowering effects of minoxidil and increase the risk of symptomatic hypotension.[204]
Sodium intake may need to be monitored in some patients, as minoxidil can cause fluid retention, and excessive sodium consumption may worsen edema.[205]
Conversely, severe sodium restriction should be avoided without medical supervision, as this could contribute to volume depletion and hypotension.[206]
Patients with cardiovascular conditions may benefit from following heart-healthy dietary patterns, including increased consumption of fruits, vegetables, whole grains, and lean proteins.[207]
Caffeine intake should be monitored, as excessive caffeine consumption may interact with minoxidil’s cardiovascular effects.[208]
Patients should discuss their dietary habits with their healthcare provider to develop an appropriate nutritional plan that supports their overall treatment goals.[209]
Can minoxidil capsules cause weight gain?
Weight gain is a potential side effect of minoxidil capsule therapy, primarily resulting from fluid retention rather than changes in body fat or muscle mass.[210]
The medication’s effects on renal sodium and water handling can lead to increased fluid accumulation in the body, manifesting as weight gain, peripheral edema, and in severe cases, pulmonary edema.[211]
Patients typically experience gradual weight gain over the first few weeks to months of treatment, though the extent varies among individuals.[212]
Regular weight monitoring is essential during minoxidil therapy, and patients should be instructed to weigh themselves daily at the same time and under similar conditions.[213]
A weight gain of more than two to three pounds over a few days may indicate significant fluid retention and should prompt immediate medical evaluation.[214]
Healthcare providers may recommend dietary sodium restriction, fluid management strategies, or the addition of diuretic medications to help control fluid retention.[215]
In some cases, the benefits of minoxidil therapy may outweigh the inconvenience of mild fluid retention, while in others, dose reduction or discontinuation may be necessary.[216]
Patients should be educated regarding the difference between fluid-related weight gain and weight gain from other causes, and they should report any rapid or concerning weight changes to their healthcare provider.[217]
How should minoxidil capsules be discontinued if treatment needs to be stopped?
Discontinuation of minoxidil capsules should always be performed under medical supervision to minimize the risk of potential complications.[218]
While minoxidil does not typically cause withdrawal symptoms in the traditional sense, abrupt discontinuation may lead to rebound hypertension in patients who have been receiving the medication for cardiovascular indications.[219]
For patients using minoxidil primarily for hair growth, gradual tapering may still be recommended to monitor for any unexpected effects.[220]
A typical tapering schedule might involve reducing the dose by 25-50% every few days to one week, depending on the starting dose and duration of therapy.[221]
Patients should be monitored closely during the discontinuation process for signs of cardiovascular instability, including elevated blood pressure, chest pain, or other cardiac symptoms.[222]
The timeline for tapering may be individualized based on patient-specific factors, including underlying health conditions, concurrent medications, and the reason for discontinuation.[223]
Patients should be informed that any hair growth benefits achieved during minoxidil therapy will gradually reverse after discontinuation, typically over a period of several months.[224]
Alternative treatments should be considered and potentially initiated before completely discontinuing minoxidil to maintain therapeutic benefits where appropriate.[225]
Healthcare providers should provide clear instructions regarding the tapering schedule and ensure that patients understand the importance of following the prescribed discontinuation plan.[226]
What monitoring is required while taking minoxidil capsules?
Comprehensive monitoring during minoxidil capsule therapy involves regular assessment of cardiovascular parameters, fluid status, and overall clinical response.[227]
Blood pressure monitoring is essential, with measurements typically recommended at baseline, during dose titration, and at regular intervals throughout treatment.[228]
Patients may be instructed to monitor their blood pressure at home using appropriate devices, with specific target ranges and instructions for when to seek medical attention.[229]
Heart rate monitoring is equally important, as minoxidil commonly causes reflex tachycardia that may require intervention in some patients.[230]
Weight monitoring should be performed daily by patients and weekly or monthly by healthcare providers to detect fluid retention early.[231]
Laboratory monitoring may include periodic assessment of renal function, electrolyte levels, and cardiac biomarkers, particularly in patients with underlying cardiovascular or renal disease.[232]
Electrocardiography may be performed at baseline and periodically during treatment to detect any cardiac rhythm abnormalities or structural changes.[233]
Echocardiography might be considered in patients receiving long-term therapy to screen for pericardial effusion, though the frequency of this monitoring has not been standardized.[234]
Patients should be educated regarding symptoms that warrant immediate medical attention, including chest pain, shortness of breath, rapid weight gain, severe dizziness, or fainting.[235]
Regular follow-up appointments should be scheduled to assess treatment response, monitor for side effects, and adjust therapy as needed.[236]
Can minoxidil capsules interact with over-the-counter medications or supplements?
Minoxidil capsules can potentially interact with various over-the-counter medications and dietary supplements, making it important for patients to disclose all substances they are taking to their healthcare provider.[237]
Nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen, naproxen, and aspirin, may reduce the effectiveness of minoxidil’s blood pressure-lowering effects and should be used with caution.[238]
Decongestants containing pseudoephedrine or phenylephrine may counteract minoxidil’s vasodilatory effects and could potentially increase blood pressure.[239]
Herbal supplements and natural products may also interact with minoxidil through various mechanisms.[240]
For example, supplements that affect blood pressure, such as garlic, hawthorn, or coenzyme Q10, may have additive effects with minoxidil.[241]
St. John’s wort and other supplements that affect liver enzymes could potentially alter minoxidil metabolism.[242]
Potassium supplements should be used cautiously, as minoxidil may affect electrolyte balance.[243]
Patients should be advised to consult with their healthcare provider or pharmacist before starting any new over-the-counter medications or supplements while taking minoxidil.[244]
This consultation should include a review of the patient’s current medication regimen and an assessment of potential interactions.[245]
Healthcare providers should maintain an updated list of all substances the patient is taking and provide guidance regarding safe use of over-the-counter products during minoxidil therapy.[246]
Is it safe to exercise while taking minoxidil capsules?
Exercise safety during minoxidil capsule therapy requires careful consideration of the medication’s cardiovascular effects and individual patient factors.[247]
The vasodilatory properties of minoxidil may affect exercise tolerance and cardiovascular response to physical activity.[248]
Patients may experience enhanced hypotensive effects during or immediately after exercise, particularly during the initial phases of treatment.[249]
Light to moderate exercise is generally considered safe for most patients taking minoxidil, but vigorous or intense exercise may need to be approached more cautiously.[250]
Patients should be advised to start with low-intensity activities and gradually increase exercise intensity while monitoring for symptoms such as dizziness, lightheadedness, chest pain, or excessive shortness of breath.[251]
Adequate hydration before, during, and after exercise is particularly important to minimize the risk of hypotension.[252]
Patients should avoid exercising in hot, humid conditions that may exacerbate vasodilation and fluid loss.[253]
Post-exercise cool-down periods should be extended to allow for gradual cardiovascular recovery.[254]
Patients with underlying cardiovascular conditions should undergo exercise stress testing or cardiac evaluation before beginning an exercise program while taking minoxidil.[255]
Healthcare providers should provide individualized exercise recommendations based on the patient’s overall health status, cardiovascular risk factors, and response to minoxidil therapy.[256]
Any concerning symptoms during exercise should prompt immediate cessation of activity and medical evaluation.[257]
What should I know about minoxidil capsules and surgery or dental procedures?
Patients scheduled for surgical or dental procedures while taking minoxidil capsules require special perioperative considerations due to the medication’s cardiovascular effects.[258]
The vasodilatory properties of minoxidil may interact with anesthetic agents and surgical stress to produce unpredictable blood pressure responses.[259]
Healthcare providers performing procedures should be informed about minoxidil use well in advance of any planned intervention.[260]
For major surgical procedures, consultation with an anesthesiologist may be necessary to develop an appropriate perioperative management plan.[261]
The decision to continue or temporarily discontinue minoxidil before surgery depends on various factors, including the type and urgency of the procedure, the patient’s underlying cardiovascular status, and the indication for minoxidil therapy.[262]
If discontinuation is necessary, it should be performed gradually under medical supervision to avoid potential rebound effects.[263]
Dental procedures generally pose lower risks, but patients should still inform their dentist about minoxidil use.[264]
The medication’s association with gingival hyperplasia may affect dental health and treatment planning.[265]
Local anesthetics containing epinephrine should be used cautiously, as they may interact with minoxidil’s cardiovascular effects.[266]
Patients should maintain good oral hygiene and receive regular dental care to monitor for gum changes.[267]
Post-procedure monitoring may need to be enhanced in patients taking minoxidil, particularly for blood pressure and cardiovascular stability.[268]
Clear communication between all healthcare providers involved in the patient’s care is essential to ensure safe perioperative management.[269]
Disclaimer: This product information is provided for educational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider before starting, stopping, or modifying any medication regimen. The information presented herein does not constitute medical advice and should not be used as a substitute for consultation with a licensed healthcare professional. Individual patient responses to medications may vary significantly, and treatment decisions should always be made in consultation with appropriate medical supervision. This document does not imply endorsement, recommendation, or guarantee of safety or efficacy for any particular use. Healthcare providers should refer to current prescribing information and clinical guidelines when making treatment decisions.
Related medications
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


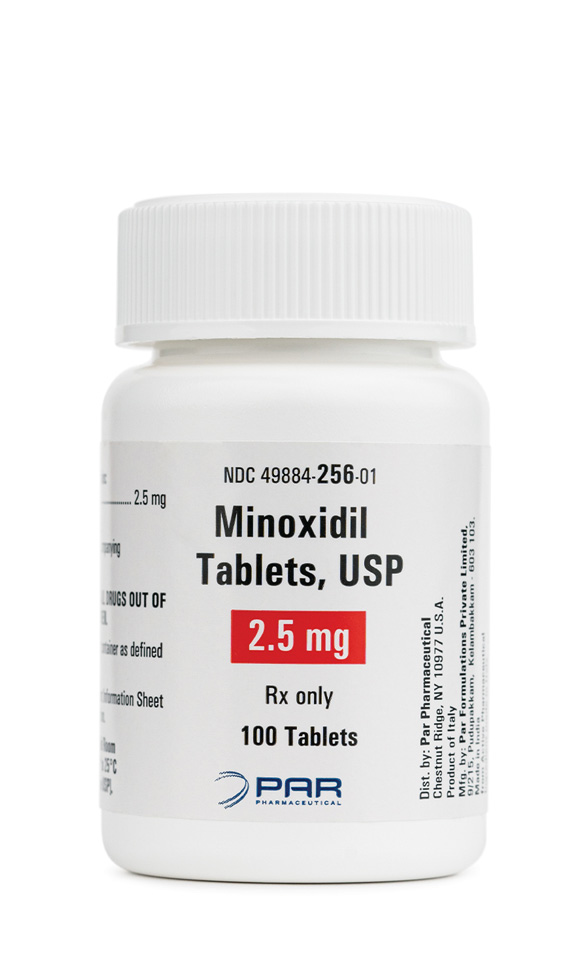
 Finasteride Tablets
Finasteride Tablets Biotin / Minoxidil / Spironolactone Capsules
Biotin / Minoxidil / Spironolactone Capsules Biotin / Minoxidil Capsules
Biotin / Minoxidil Capsules Hair Restore Extreme Scalp Solution
Hair Restore Extreme Scalp Solution Hair Restore Ultra Scalp Solution
Hair Restore Ultra Scalp Solution Hair Restore D Scalp Solution
Hair Restore D Scalp Solution Hair Restore Lite Scalp Solution
Hair Restore Lite Scalp Solution GHK-Cu Scalp Solution
GHK-Cu Scalp Solution