Product Overview
† commercial product
Melatonin capsules represent a formulation of N-acetyl-5-methoxytryptamine, a naturally occurring hormone primarily synthesized by the pineal gland during periods of darkness. This neurohormone plays a crucial role in regulating circadian rhythms and sleep-wake cycles in humans and other mammals.[1]
The compound melatonin was first isolated and characterized in 1958 by Aaron Lerner and colleagues, who identified its chemical structure and named it based on its ability to lighten melanophores in amphibian skin.[3] Since its discovery, extensive research has revealed melatonin’s multifaceted physiological functions, extending beyond sleep regulation to include antioxidant properties, immune system modulation, and potential neuroprotective effects.[4] The endogenous production of melatonin follows a distinct circadian pattern, with levels typically rising in the evening, peaking during the middle of the night, and declining toward morning.[5]
The bioavailability of oral melatonin varies considerably among individuals, with factors such as age, hepatic function, and concurrent medications potentially influencing absorption and metabolism.[9] Following oral administration, melatonin undergoes first-pass hepatic metabolism primarily through cytochrome P450 enzymes, particularly CYP1A2, resulting in the formation of 6-sulfatoxymelatonin, which is subsequently eliminated through renal excretion.[10] The pharmacokinetic profile of melatonin demonstrates rapid absorption with peak plasma concentrations typically achieved within 30 to 120 minutes after oral administration, though considerable inter-individual variability exists.[11]
Healthcare providers may consider melatonin supplementation for patients experiencing various sleep-related disorders, including delayed sleep phase syndrome, jet lag, shift work sleep disorder, and certain forms of insomnia.[12] The therapeutic application of melatonin extends beyond primary sleep disorders to include potential benefits in managing sleep disturbances associated with neurodevelopmental conditions, neurodegenerative diseases, and certain psychiatric disorders.[13] However, the decision to prescribe melatonin should always be based on comprehensive patient assessment and consideration of individual factors that may influence treatment response and safety.[14]
Melatonin exhibits significant inter-individual variability in absorption, metabolism, and therapeutic response, necessitating careful titration and monitoring to achieve optimal outcomes.[145] For most adult patients with sleep disorders, initial melatonin doses typically range from 0.5 mg to 3 mg administered one to three hours before desired bedtime.[146] The 10 mg strength may represent a higher dose that could be appropriate for patients who have not responded adequately to lower doses or those with specific conditions requiring higher melatonin levels.[147] However, healthcare providers should generally employ a start-low-and-go-slow approach, beginning with the lowest effective dose and increasing gradually as needed based on clinical response and tolerability.[148]
The timing of melatonin administration plays a crucial role in therapeutic effectiveness and may vary depending on the specific sleep disorder being treated.[149] For patients with difficulty falling asleep, melatonin is typically administered 30 minutes to 3 hours before desired bedtime.[150] The optimal timing may need to be individualized based on the patient’s natural melatonin production patterns and specific circadian rhythm characteristics.[151] Patients with delayed sleep phase disorder may require earlier administration times to help advance their sleep-wake cycle.[152]
For circadian rhythm disorders such as jet lag, melatonin dosing strategies may differ significantly from those used for primary sleep disorders.[153] Jet lag protocols typically involve lower doses (0.5 to 3 mg) timed according to the destination time zone.[154] The 10 mg dose may be excessive for jet lag management and could potentially worsen circadian disruption or cause excessive sedation.[155] Healthcare providers should carefully consider the appropriateness of higher doses for circadian rhythm applications.[156]
Shift work sleep disorder presents unique dosing challenges that may require modified administration strategies.[157] Workers transitioning between different shift schedules may need varying melatonin doses and timing protocols to help adjust their circadian rhythms.[158] The 10 mg dose might be appropriate for some shift workers, particularly those having difficulty adapting to night shift schedules.[159] However, careful consideration must be given to timing administration to avoid sedation during required waking hours.[160]
Elderly patients may require special dosing considerations due to age-related changes in melatonin metabolism and increased sensitivity to sedating medications.[161] Older adults typically have reduced endogenous melatonin production and may benefit from supplementation, but they may also be more susceptible to side effects.[162] Lower starting doses are generally recommended for elderly patients, with careful upward titration as needed.[163] The 10 mg dose may be too high for many elderly patients and could increase risks of falls, cognitive impairment, or other adverse effects.[164]
Patients with hepatic impairment require careful dose adjustments due to reduced melatonin clearance.[165] The extensive hepatic metabolism of melatonin means that patients with liver disease may experience prolonged drug effects and increased risk of accumulation.[166] Healthcare providers should consider significant dose reductions in patients with any degree of hepatic impairment and monitor closely for signs of excessive sedation or other adverse effects.[167]
Duration of treatment represents another important consideration in melatonin therapy.[168] While short-term use for specific situations like jet lag is well-established, the safety and efficacy of long-term melatonin supplementation remain areas of ongoing research.[169] Some patients may require chronic treatment for persistent sleep disorders, while others may benefit from intermittent or seasonal use.[170] Healthcare providers should regularly reassess the need for continued treatment and consider periodic drug holidays to evaluate ongoing necessity.[171]
Melatonin’s primary mechanism of action involves binding to specific melatonin receptors located throughout the central nervous system and peripheral tissues.[15] The two main melatonin receptor subtypes, designated MT1 and MT2, are G-protein coupled receptors that mediate the majority of melatonin’s physiological effects.[16] MT1 receptors are primarily associated with sleep induction and maintenance, while MT2 receptors play a more significant role in circadian rhythm regulation and phase shifting.[17] These receptors are predominantly found in the suprachiasmatic nucleus of the hypothalamus, which serves as the body’s master circadian clock, as well as in various other brain regions including the hippocampus, cortex, and brainstem.[18]
Upon binding to MT1 receptors, melatonin initiates a cascade of intracellular signaling events that ultimately result in decreased neuronal firing and reduced alertness.[19] This receptor activation leads to inhibition of adenylyl cyclase activity, resulting in decreased cyclic adenosine monophosphate levels and subsequent modulation of protein kinase A activity.[20] The net effect of these molecular changes is a reduction in neuronal excitability and promotion of sleep-conducive brain states.[21] Additionally, melatonin binding to MT1 receptors may influence calcium channel activity and potassium channel conductance, further contributing to its sleep-promoting effects.[22]
The MT2 receptor-mediated effects of melatonin are particularly important for circadian rhythm regulation and phase adjustment.[23] Activation of MT2 receptors in the suprachiasmatic nucleus can shift the timing of the circadian clock, either advancing or delaying the sleep-wake cycle depending on the timing of melatonin administration.[24] This phase-shifting capability makes melatonin particularly valuable in treating circadian rhythm disorders such as jet lag and shift work sleep disorder.[25] The magnitude and direction of phase shifts induced by exogenous melatonin depend on several factors, including the dose, timing of administration relative to the individual’s endogenous circadian phase, and the patient’s sensitivity to melatonin.[26]
Beyond its direct receptor-mediated effects, melatonin demonstrates significant antioxidant properties that may contribute to its therapeutic benefits.[27] Unlike many other antioxidants, melatonin can cross cellular membranes freely and access intracellular compartments, including mitochondria, where it may help protect against oxidative damage.[28] This antioxidant activity occurs through both direct free radical scavenging and indirect mechanisms involving the upregulation of antioxidant enzymes such as superoxide dismutase, catalase, and glutathione peroxidase.[29] The neuroprotective effects of melatonin may be particularly relevant in age-related sleep disorders and neurodegenerative conditions where oxidative stress plays a contributing role.[30]
Melatonin also exhibits immunomodulatory properties that may influence various aspects of immune function.[31] The hormone can affect both innate and adaptive immune responses, with effects that may vary depending on the dose, timing, and duration of administration.[32] Some research suggests that melatonin may enhance certain immune functions while suppressing excessive inflammatory responses, though the clinical significance of these effects in the context of sleep disorders remains an area of ongoing investigation.[33] The complex interplay between sleep, circadian rhythms, and immune function suggests that melatonin’s therapeutic benefits may extend beyond direct sleep promotion to include broader health maintenance effects.[34]
Several absolute and relative contraindications exist for melatonin supplementation that healthcare providers must carefully consider before prescribing melatonin capsules.[35] Patients with known hypersensitivity or allergic reactions to melatonin or any components of the formulation should not receive this medication.[36] Allergic reactions to melatonin, while relatively uncommon, can range from mild skin reactions to more severe systemic responses requiring immediate medical attention.[37]
Autoimmune disorders represent another important contraindication category for melatonin supplementation.[38] The immunomodulatory effects of melatonin may potentially exacerbate certain autoimmune conditions or interfere with immunosuppressive treatments.[39] Patients with conditions such as rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, or other autoimmune disorders should be carefully evaluated before melatonin therapy initiation.[40] The theoretical risk of immune system stimulation could potentially worsen disease activity or reduce the effectiveness of immunosuppressive medications.[41]
Severe hepatic impairment constitutes a significant contraindication due to melatonin’s extensive hepatic metabolism.[42] Patients with advanced liver disease may experience altered melatonin clearance, potentially leading to prolonged half-life and increased risk of adverse effects.[43] The primary metabolic pathway for melatonin involves cytochrome P450 enzymes, particularly CYP1A2, which may be significantly impaired in patients with severe hepatic dysfunction.[44] Healthcare providers should exercise extreme caution when considering melatonin therapy in patients with any degree of liver impairment and may need to consider alternative treatment approaches.[45]
Pregnancy and lactation represent important contraindication considerations due to limited safety data regarding melatonin use during these periods.[46] While melatonin is naturally produced during pregnancy and may play important roles in fetal development, the safety of exogenous melatonin supplementation has not been adequately established.[47] The hormone can cross the placental barrier and may potentially influence fetal circadian rhythm development, though the long-term consequences of such exposure remain unknown.[48] Similarly, melatonin is present in breast milk, and the effects of supplemental melatonin on nursing infants have not been thoroughly studied.[49]
Pediatric populations require special consideration regarding melatonin contraindications.[50] While melatonin is sometimes used in children with specific sleep disorders or neurodevelopmental conditions, concerns exist regarding potential effects on pubertal development and reproductive hormone function.[51] The developing endocrine system may be particularly sensitive to exogenous melatonin, and long-term safety data in pediatric populations remain limited.[52] Healthcare providers should carefully weigh potential benefits against unknown risks when considering melatonin therapy in children and adolescents.[53]
Patients with seizure disorders may represent a relative contraindication category due to conflicting evidence regarding melatonin’s effects on seizure activity.[54] While some studies suggest potential anticonvulsant properties, others indicate that melatonin might lower seizure threshold in susceptible individuals.[55] The complex relationship between sleep, circadian rhythms, and seizure activity necessitates careful consideration and potentially specialized neurological consultation before initiating melatonin therapy in patients with epilepsy or other seizure disorders.[56]
Melatonin demonstrates several clinically significant drug interactions that require careful consideration and monitoring when prescribing melatonin capsules.[57] The most important interactions involve medications that affect cytochrome P450 enzyme systems, particularly CYP1A2, which is the primary pathway for melatonin metabolism.[58] Drugs that inhibit or induce these enzymes can significantly alter melatonin’s pharmacokinetic profile and potentially affect therapeutic outcomes or increase the risk of adverse effects.[59]
Fluvoxamine, a selective serotonin reuptake inhibitor with potent CYP1A2 inhibitory activity, can dramatically increase melatonin plasma concentrations.[60] This interaction may result in enhanced and prolonged melatonin effects, potentially leading to excessive sedation, morning grogginess, or other concentration-related adverse events.[61] Healthcare providers should consider significant dose reductions when melatonin is co-administered with fluvoxamine or may need to select alternative treatment approaches.[62] Other medications with CYP1A2 inhibitory properties, including ciprofloxacin, zileuton, and certain antiarrhythmic drugs, may produce similar interactions requiring dose adjustments.[63]
Conversely, medications that induce CYP1A2 activity may accelerate melatonin metabolism and reduce its therapeutic effectiveness.[64] Smoking tobacco products represents one of the most significant CYP1A2 inducers, potentially requiring higher melatonin doses in patients who smoke cigarettes.[65] Other enzyme inducers, including certain anticonvulsants such as carbamazepine and phenytoin, may similarly reduce melatonin efficacy and necessitate dose adjustments.[66] Healthcare providers should carefully monitor treatment response in patients taking enzyme-inducing medications and be prepared to modify dosing regimens accordingly.[67]
Warfarin and other anticoagulant medications may interact with melatonin through complex mechanisms involving both pharmacokinetic and pharmacodynamic pathways.[68] Some case reports suggest that melatonin may enhance anticoagulant effects, potentially increasing bleeding risk in susceptible patients.[69] While the exact mechanism remains unclear, healthcare providers should exercise increased vigilance when monitoring coagulation parameters in patients receiving concurrent melatonin and anticoagulant therapy.[70] More frequent international normalized ratio monitoring may be appropriate when initiating or discontinuing melatonin in patients taking warfarin.[71]
Central nervous system depressants represent another important interaction category that may result in additive sedative effects when combined with melatonin.[72] Medications such as benzodiazepines, barbiturates, opioid analgesics, and certain antihistamines may produce enhanced sedation when used concurrently with melatonin.[73] While this interaction may sometimes be therapeutically beneficial in carefully managed situations, it also increases the risk of excessive sedation, impaired cognitive function, and potentially dangerous activities such as driving.[74] Healthcare providers should counsel patients about these risks and consider dose modifications when combining melatonin with other sedating medications.[75]
Antihypertensive medications, particularly beta-blockers, may interact with melatonin through effects on endogenous melatonin production.[76] Beta-blockers can suppress natural melatonin synthesis by blocking adrenergic stimulation of the pineal gland.[77] This suppression may create a rationale for melatonin supplementation in patients taking beta-blockers who experience sleep disturbances, though the optimal dosing and timing strategies in this population require further research.[78] Healthcare providers should be aware of this interaction and consider its potential implications when evaluating sleep complaints in patients taking beta-blocking agents.[79]
Immunosuppressive medications may potentially interact with melatonin due to the hormone’s immunomodulatory properties.[80] While specific clinical evidence remains limited, theoretical concerns exist regarding melatonin’s potential to counteract immunosuppressive effects in organ transplant recipients or patients with autoimmune conditions.[81] Healthcare providers should exercise caution when considering melatonin therapy in patients taking immunosuppressive medications and may need to consult with specialists regarding appropriate monitoring strategies.[82]
Melatonin supplementation is generally well-tolerated by most patients, though various side effects may occur with different frequencies and severities.[83] The most commonly reported adverse effects are typically mild and transient, often resolving with continued use or dose adjustments.[84] However, healthcare providers should thoroughly discuss potential side effects with patients and establish appropriate monitoring protocols to ensure safe and effective treatment.[85]
Daytime sedation and morning grogginess represent the most frequently encountered side effects of melatonin supplementation.[86] These effects may be particularly pronounced in patients taking higher doses or those with slower melatonin metabolism.[87] The timing of melatonin administration plays a crucial role in minimizing these effects, with most experts recommending administration one to three hours before desired bedtime.[88] Patients experiencing persistent morning sedation may benefit from dose reduction or earlier administration timing.[89] In some cases, switching to immediate-release formulations rather than extended-release preparations may help reduce morning after-effects.[90]
Headaches occur in approximately 5 to 10 percent of patients taking melatonin supplements.[91] These headaches are typically mild to moderate in intensity and may resolve spontaneously with continued treatment.[92] The mechanism underlying melatonin-induced headaches remains unclear, though vascular effects or changes in neurotransmitter activity may contribute.[93] Patients experiencing persistent or severe headaches should be evaluated for other potential causes, and dose reduction or treatment discontinuation may be necessary.[94]
Gastrointestinal side effects, including nausea, abdominal discomfort, and diarrhea, may occur in some patients taking melatonin.[95] These effects are generally mild and may be minimized by taking melatonin with food or reducing the dose.[96] Rarely, more severe gastrointestinal symptoms may necessitate treatment discontinuation.[97] Patients with pre-existing gastrointestinal conditions may be at increased risk for these side effects and should be monitored accordingly.[98]
Mood-related side effects, including irritability, anxiety, and depression, have been reported in some patients taking melatonin.[99] While these effects are relatively uncommon, they may be more likely to occur in patients with pre-existing mood disorders or those taking higher doses.[100] The relationship between melatonin and mood is complex, with some studies suggesting potential antidepressant effects while others report mood-related adverse events.[101] Healthcare providers should carefully monitor patients with psychiatric histories and consider psychiatric consultation if significant mood changes occur during melatonin treatment.[102]
Dizziness and balance problems may occur in some patients, particularly elderly individuals who may be more sensitive to melatonin’s effects.[103] These symptoms may increase fall risk and require careful evaluation in older patients.[104] Dose reduction or treatment discontinuation may be necessary if dizziness persists or interferes with daily activities.[105] Patients should be counseled about potential dizziness and advised to use caution when changing positions or engaging in activities requiring balance.[106]
Sleep-related side effects, paradoxically, may include vivid dreams, nightmares, or sleep fragmentation in some patients.[107] These effects may be dose-related and could indicate that the prescribed dose is too high for the individual patient.[108] Adjusting the dose or timing of administration may help resolve these sleep disturbances.[109] In rare cases, melatonin may worsen certain sleep disorders or create new sleep problems requiring treatment modification.[110]
Hormonal effects represent a potential concern, particularly with long-term melatonin use.[111] Some studies suggest that melatonin may influence reproductive hormone levels, though the clinical significance of these effects remains unclear.[112] Patients of reproductive age should be informed about potential hormonal effects, and periodic monitoring may be appropriate for patients receiving long-term treatment.[113] Additionally, melatonin may affect growth hormone and cortisol levels, though these changes are typically not clinically significant in most patients.[114]
The use of melatonin during pregnancy presents complex considerations that require careful evaluation of potential benefits and risks.[115] Endogenous melatonin production naturally increases during pregnancy, with maternal melatonin levels rising significantly in the third trimester.[116] This natural increase suggests that melatonin plays important physiological roles during pregnancy, including potential effects on fetal development, maternal circadian rhythms, and pregnancy outcomes.[117] However, the safety and appropriate use of exogenous melatonin supplementation during pregnancy remain areas of ongoing research and clinical uncertainty.[118]
Current evidence regarding melatonin safety in pregnancy is limited and primarily based on animal studies and small human observational studies.[119] Animal research has generally not revealed major teratogenic effects of melatonin, and some studies suggest potential protective effects against pregnancy complications.[120] However, animal studies have limitations in their applicability to human pregnancy, and the doses used in research settings may not reflect typical clinical use patterns.[121] The lack of large-scale, controlled human studies means that definitive safety conclusions cannot be drawn regarding melatonin use during pregnancy.[122]
Melatonin readily crosses the placental barrier, allowing direct fetal exposure to exogenous melatonin supplementation.[123] This placental transfer raises important questions about potential effects on fetal circadian rhythm development and other aspects of fetal physiology.[124] The developing fetal brain contains melatonin receptors, and exposure to supplemental melatonin could theoretically influence normal neurodevelopmental processes.[125] However, the long-term consequences of prenatal melatonin exposure on child development remain largely unknown.[126]
Some research suggests that melatonin may have protective effects against certain pregnancy complications, including preeclampsia and intrauterine growth restriction.[127] The antioxidant properties of melatonin may help protect against oxidative stress that contributes to various pregnancy complications.[128] Additionally, melatonin’s effects on blood pressure regulation and placental function may theoretically provide benefits in high-risk pregnancies.[129] However, these potential benefits must be weighed against the uncertainty regarding safety and the availability of alternative treatments with more established safety profiles.[130]
Sleep disturbances are common during pregnancy, affecting up to 80 percent of pregnant women at some point during gestation.[131] These sleep problems may result from hormonal changes, physical discomfort, anxiety, or other pregnancy-related factors.[132] While melatonin might theoretically help address some of these sleep issues, healthcare providers typically recommend non-pharmacological approaches as first-line treatments for pregnancy-related sleep disturbances.[133] Sleep hygiene measures, cognitive behavioral therapy for insomnia, and environmental modifications may provide safer alternatives for managing sleep problems during pregnancy.[134]
Current professional guidelines generally recommend avoiding melatonin supplementation during pregnancy unless the potential benefits clearly outweigh the unknown risks.[135] The American College of Obstetricians and Gynecologists has not established specific recommendations regarding melatonin use in pregnancy, reflecting the limited available evidence.[136] Healthcare providers considering melatonin therapy for pregnant patients should engage in thorough informed consent discussions, exploring alternative treatment options and carefully documenting the rationale for any decision to use melatonin during pregnancy.[137]
Lactation presents similar considerations regarding melatonin safety and use.[138] Melatonin is naturally present in breast milk, with concentrations following a circadian pattern that may help establish infant sleep-wake rhythms.[139] However, the effects of supplemental maternal melatonin on nursing infants have not been adequately studied.[140] The potential for altered infant sleep patterns, developmental effects, or other consequences of increased melatonin exposure through breast milk remains unknown.[141] Healthcare providers should carefully consider these uncertainties when evaluating melatonin therapy requests from breastfeeding mothers.[142]
Proper storage and handling of melatonin capsules are essential for maintaining medication stability, potency, and safety throughout the prescribed treatment period.[172] The chemical stability of melatonin can be affected by various environmental factors, including temperature, humidity, light exposure, and oxygen contact, making appropriate storage conditions critical for preserving therapeutic effectiveness.[173] Healthcare providers should educate patients about proper storage requirements and provide clear instructions regarding handling procedures to ensure optimal medication quality.[174]
Melatonin capsules should be stored at room temperature, typically defined as 20 to 25 degrees Celsius (68 to 77 degrees Fahrenheit).[175] Extreme temperatures can adversely affect capsule integrity and drug stability, potentially leading to reduced potency or altered dissolution characteristics.[176] Patients should be advised to avoid storing medication in locations subject to temperature fluctuations, such as automobiles, bathrooms, or areas near heating or cooling vents.[177] Refrigeration is generally not required for melatonin capsules and may actually be detrimental due to potential moisture condensation issues.[178]
Protection from light exposure represents another critical storage requirement for melatonin preparations.[179] Melatonin demonstrates photosensitivity and can undergo degradation when exposed to direct sunlight or bright artificial lighting.[180] Capsules should be stored in their original containers, which are typically designed to provide adequate light protection.[181] Patients should avoid transferring capsules to clear containers or pill organizers that may not provide sufficient light barrier properties.[182] If pill organizers are necessary for medication management, opaque containers should be selected and stored in dark locations.[183]
Moisture control is essential for maintaining capsule integrity and preventing drug degradation.[184] Melatonin capsules should be stored in dry environments with low humidity levels.[185] The original container typically includes desiccant materials designed to absorb excess moisture and should not be removed.[186] Patients should be instructed to keep containers tightly closed when not in use and to avoid opening containers in humid environments such as bathrooms immediately after showering.[187] Any capsules that appear to have moisture damage, including changes in appearance, texture, or odor, should not be consumed and should be reported to the prescribing healthcare provider.[188]
Proper handling techniques can help prevent contamination and maintain medication quality.[189] Patients should wash and dry their hands thoroughly before handling capsules.[190] Capsules should be removed from containers using clean, dry hands rather than pouring them into wet or contaminated palms.[191] If a capsule is accidentally dropped or comes into contact with contaminated surfaces, it should be discarded rather than consumed.[192] Patients should avoid touching capsules unnecessarily, as oils and moisture from skin contact may affect capsule integrity over time.[193]
Container integrity plays a crucial role in maintaining medication stability throughout the storage period.[194] Original pharmacy containers are specifically selected to provide appropriate barrier properties against moisture, light, and oxygen.[195] Patients should inspect containers regularly for signs of damage, including cracks, broken seals, or compromised closures.[196] Damaged containers should be reported to the dispensing pharmacy for replacement.[197] Child-resistant closures should be properly secured after each use to maintain safety and prevent accidental ingestion by children or pets.[198]
Transportation and travel considerations may require special attention for patients who need to carry melatonin capsules away from home.[203] Medications should be transported in their original containers with clear labeling to facilitate identification and prevent confusion with other medications.[204] During travel, capsules should be protected from extreme temperatures and humidity, particularly during air travel where cargo compartments may experience temperature variations.[205] Patients traveling across time zones should consult with their healthcare providers regarding appropriate timing adjustments for melatonin administration.[206]
- Reiter, R. J., Tan, D. X., & Korkmaz, A. (2019). The circadian melatonin rhythm and its modulation: possible impact on hypertension. Journal of Hypertension, 27(Suppl 4), S17- S20. https://doi.org/10.1097/HJH.0b013e32832f7b1b
- Zisapel, N. (2018). New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. British Journal of Pharmacology, 175(16), 3190-3199. https://doi.org/10.1111/bph.14116
- Lerner, A. B., Case, J. D., Takahashi, Y., Lee, T. H., & Mori, W. (1958). Isolation of melatonin, the pineal gland factor that lightens melanocytes. Journal of the American Chemical Society, 80(10), 2587. https://doi.org/10.1021/ja01543a060
- Cardinali, D. P., Srinivasan, V., Brzezinski, A., & Brown, G. M. (2012). Melatonin and its analogs in insomnia and depression. Journal of Pineal Research, 52(4), 365-375. https://doi.org/10.1111/j.1600-079X.2011.00962.x
- Claustrat, B., & Leston, J. (2015). Melatonin: physiological effects in humans. Neurochirurgie, 61(2-3), 77-84. https://doi.org/10.1016/j.neuchi.2015.03.002
- U.S. Food and Drug Administration. (2019). Compounding and the FDA: Questions and answers. Retrieved from https://www.fda.gov/drugs/human-drug-compounding/compounding-and-fda-questions-and-answers
- International Academy of Compounding Pharmacists. (2018). 503A compounding regulations and guidelines. Compounding Today, 24(3), 15-22.
- Ferracioli-Oda, E., Qawasmi, A., & Bloch, M. H. (2013). Meta-analysis: melatonin for the treatment of primary sleep disorders. PLoS One, 8(5), e63773. https://doi.org/10.1371/journal.pone.0063773
- Fourtillan, J. B., Brisson, A. M., Gobin, P., Ingrand, I., Decourt, J. P., & Girault, J. (2000). Bioavailability of melatonin in humans after daytime administration of D(7) melatonin. Biopharmaceutics & Drug Disposition, 21(1), 15-22. https://doi.org/10.1002/1099- 081X(200001)21:1<15::AID-BDD215>3.0.CO;2-H
- Ma, X., Idle, J. R., Krausz, K. W., & Gonzalez, F. J. (2005). Metabolism of melatonin by human cytochromes p450. Drug Metabolism and Disposition, 33(4), 489-494. https://doi.org/10.1124/dmd.104.002410
- Waldhauser, F., Waldhauser, M., Lieberman, H. R., Deng, M. H., Lynch, H. J., & Wurtman, R. J. (1984). Bioavailability of oral melatonin in humans. Neuroendocrinology, 39(4), 307-313. https://doi.org/10.1159/000123992
- American Academy of Sleep Medicine. (2017). International classification of sleep disorders (3rd ed.). American Academy of Sleep Medicine.
- Gringras, P., Nir, T., Breddy, J., Frydman-Marom, A., & Findling, R. L. (2017). Efficacy and safety of pediatric prolonged-release melatonin for insomnia in children with autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 56(11), 948-957. https://doi.org/10.1016/j.jaac.2017.09.414
- Sateia, M. J., Buysse, D. J., Krystal, A. D., Neubauer, D. N., & Heald, J. L. (2017). Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults. Journal of Clinical Sleep Medicine, 13(2), 307-349. https://doi.org/10.5664/jcsm.6470
- Dubocovich, M. L., & Markowska, M. (2005). Functional MT1 and MT2 melatonin receptors in mammals. Endocrine, 27(2), 101-110. https://doi.org/10.1385/ENDO:27:2:101
- Liu, J., Clough, S. J., Hutchinson, A. J., Adamah-Biassi, E. B., Popovska-Gorevski, M., & Dubocovich, M. L. (2016). MT1 and MT2 melatonin receptors: a therapeutic perspective. Annual Review of Pharmacology and Toxicology, 56, 361-383. https://doi.org/10.1146/annurev-pharmtox-010814-124742
- Jockers, R., Delagrange, P., Dubocovich, M. L., Markus, R. P., Renault, N., Tosini, G., … & Boutin, J. A. (2016). Update on melatonin receptors: IUPHAR Review 20. British Journal of Pharmacology, 173(18), 2702-2725. https://doi.org/10.1111/bph.13536
- Reppert, S. M., Weaver, D. R., & Ebisawa, T. (1994). Cloning and characterization of a mammalian melatonin receptor that mediates reproductive and circadian responses. Neuron, 13(5), 1177-1185. https://doi.org/10.1016/0896-6273(94)90055-8
- Pandi-Perumal, S. R., Trakht, I., Srinivasan, V., Spence, D. W., Maestroni, G. J., Zisapel, N., & Cardinali, D. P. (2008). Physiological effects of melatonin: role of melatonin receptors and signal transduction pathways. Progress in Neurobiology, 85(3), 335-353. https://doi.org/10.1016/j.pneurobio.2008.04.001
- Witt-Enderby, P. A., Bennett, J., Jarzynka, M. J., Firestine, S., & Melan, M. A. (2003). Melatonin receptors and their regulation: biochemical and structural mechanisms. Life Sciences, 72(20), 2183-2198. https://doi.org/10.1016/S0024-3205(03)00098-5
- Zlotos, D. P., Jockers, R., Cecon, E., Rivara, S., & Witt-Enderby, P. A. (2014). MT1 and MT2 melatonin receptors: ligand binding and activation. Journal of Medicinal Chemistry, 57(8), 3161-3185. https://doi.org/10.1021/jm4018913
- Nelson, C. S., Ikeda, M., Gompf, H. S., Robinson, M. L., Fuchs, N. K., Yoshioka, T., … & Saper, C. B. (2004). Acute melatonin synthesis requires arylalkylamine N-acetyltransferase in the rat pineal gland. Neuroscience Letters, 358(3), 159-162. https://doi.org/10.1016/j.neulet.2003.12.119
- Hunt, A. E., Al-Ghoul, W. M., Gillette, M. U., & Dubocovich, M. L. (2001). Activation of MT2 melatonin receptors in rat suprachiasmatic nucleus phase advances the circadian clock. American Journal of Physiology-Cell Physiology, 280(1), C110-C118. https://doi.org/10.1152/ajpcell.2001.280.1.C110
- Lewy, A. J., Wehr, T. A., Goodwin, F. K., Newsome, D. A., & Markey, S. P. (1980). Light suppresses melatonin secretion in humans. Science, 210(4475), 1267-1269. https://doi.org/10.1126/science.7434030
- Arendt, J., & Skene, D. J. (2005). Melatonin as a chronobiotic. Sleep Medicine Reviews, 9(1), 25-39. https://doi.org/10.1016/j.smrv.2004.05.002
- Burgess, H. J., Revell, V. L., & Eastman, C. I. (2008). A three pulse phase response curve to three milligrams of melatonin in humans. Journal of Physiology, 586(2), 639-647. https://doi.org/10.1113/jphysiol.2007.143180
- Reiter, R. J., Mayo, J. C., Tan, D. X., Sainz, R. M., Alatorre-Jimenez, M., & Qin, L. (2016). Melatonin as an antioxidant: under promises but over delivers. Journal of Pineal Research, 61(3), 253-278. https://doi.org/10.1111/jpi.12360
- Tan, D. X., Manchester, L. C., Terron, M. P., Flores, L. J., & Reiter, R. J. (2007). One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species? Journal of Pineal Research, 42(1), 28-42. https://doi.org/10.1111/j.1600-079X.2006.00407.x
- Rodriguez, C., Mayo, J. C., Sainz, R. M., Antolín, I., Herrera, F., Martín, V., & Reiter, R. J. (2004). Regulation of antioxidant enzymes: a significant role for melatonin. Journal of Pineal Research, 36(1), 1-9. https://doi.org/10.1046/j.1600-079X.2003.00092.x
- Hardeland, R. (2005). Antioxidative protection by melatonin: multiplicity of mechanisms from radical detoxification to radical avoidance. Endocrine, 27(2), 119-130. https://doi.org/10.1385/ENDO:27:2:119
- Carrillo-Vico, A., Lardone, P. J., Álvarez-Sánchez, N., Rodríguez-Rodríguez, A., & Guerrero, J. M. (2013). Melatonin: buffering the immune system. International Journal of Molecular Sciences, 14(4), 8638-8683. https://doi.org/10.3390/ijms14048638
- Maestroni, G. J. (2001). The immunotherapeutic potential of melatonin. Expert Opinion on Investigational Drugs, 10(3), 467-476. https://doi.org/10.1517/13543784.10.3.467
- Srinivasan, V., Mohamed, M., & Kato, H. (2012). Melatonin in bacterial and viral infections with focus on sepsis: a review. Recent Patents on Endocrine, Metabolic & Immune Drug Discovery, 6(1), 30-39. https://doi.org/10.2174/187221412799015317
- Besedovsky, L., Lange, T., & Haack, M. (2019). The sleep-immune crosstalk in health and disease. Physiological Reviews, 99(3), 1325-1380. https://doi.org/10.1152/physrev.00010.2018
- Buscemi, N., Vandermeer, B., Hooton, N., Pandya, R., Tjosvold, L., Hartling, L., … & Vohra, S. (2006). Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ, 332(7538), 385- 393. https://doi.org/10.1136/bmj.38731.532766.F6
- Andersen, L. P., Gögenur, I., Rosenberg, J., & Reiter, R. J. (2016). The safety of melatonin in humans. Clinical Drug Investigation, 36(3), 169-175. https://doi.org/10.1007/s40261- 015-0368-5
- McMahon, S. B., Ownby, D. R., Ownby, H. E., & Hadley, J. A. (2003). The atopic march: patterns of allergic disease development in childhood. Annals of Allergy, Asthma & Immunology, 91(2), 136-143. https://doi.org/10.1016/S1081-1206(10)62168-9
- Cutolo, M., Maestroni, G. J., Otsa, K., Aakre, O., Villaggio, B., Capellino, S., … & Straub, R. H. (2005). Circadian melatonin and cortisol levels in rheumatoid arthritis patients in winter time: a north and south Europe comparison. Annals of the Rheumatic Diseases, 64(2), 212-216. https://doi.org/10.1136/ard.2004.023416
- Maestroni, G. J. (1993). The immunoneuroendocrine role of melatonin. Journal of Pineal Research, 14(1), 1-10. https://doi.org/10.1111/j.1600-079X.1993.tb00497.x
- Pontes, G. N., Cardoso, E. C., Carneiro-Sampaio, M. M., & Markus, R. P. (2006). Injury switches melatonin production source from endocrine (pineal) to paracrine (phagocytes)- melatonin in human colostrum and colostrum phagocytes. Journal of Pineal Research, 41(2), 136-141. https://doi.org/10.1111/j.1600-079X.2006.00345.x
- Srinivasan, V., Spence, D. W., Pandi-Perumal, S. R., Trakht, I., & Cardinali, D. P. (2008). Therapeutic actions of melatonin in cancer: possible mechanisms. Integrative Cancer Therapies, 7(3), 189-203. https://doi.org/10.1177/1534735408322846
- Härtter, S., Grözinger, M., Weigmann, H., Röschke, J., & Hiemke, C. (2000). Increased bioavailability of oral melatonin after fluvoxamine coadministration. Clinical Pharmacology & Therapeutics, 67(1), 1-6. https://doi.org/10.1067/mcp.2000.103985
- Young, I. M., Leone, R. M., Francis, P., Stovell, P., & Silman, R. E. (1985). Melatonin is metabolized to N-acetyl serotonin and 6-hydroxymelatonin in man. Journal of Clinical Endocrinology & Metabolism, 60(1), 114-119. https://doi.org/10.1210/jcem-60-1-114
- Facciola, G., Hidestrand, M., von Bahr, C., & Tybring, G. (2001). Cytochrome P450 isoforms involved in melatonin metabolism in human liver microsomes. European Journal of Clinical Pharmacology, 56(12), 881-888. https://doi.org/10.1007/s002280000245
- Ozturk, G., Akbulut, K. G., & Guney, S. (2012). Melatonin, aging, and COVID-19: could melatonin be beneficial for COVID-19 treatment in elderly patients? Turkish Journal of Medical Sciences, 50(4), 1504-1512. https://doi.org/10.3906/sag-2005-356
- Voiculescu, S. E., Zygouropoulos, N., Zahiu, C. D., & Zagrean, A. M. (2014). Role of melatonin in embryo fetal development. Journal of Medicine and Life, 7(4), 488-492.
- Nakamura, Y., Tamura, H., Kashida, S., Takayama, H., Yamagata, Y., Karube, A., … & Sugino, N. (2001). Changes of serum melatonin level and its relationship to feto-placental unit during pregnancy. Journal of Pineal Research, 30(1), 29-33. https://doi.org/10.1034/j.1600-079X.2001.300104.x
- Torres-Farfan, C., Rocco, V., Monsó, C., Valenzuela, F. J., Campino, C., Germain, A., … & Valenzuela, G. J. (2006). Maternal melatonin effects on clock gene expression in a nonhuman primate fetus. Endocrinology, 147(10), 4618-4626. https://doi.org/10.1210/en.2006-0628
- Cubero, J., Narciso, D., Aparicio, S., Garau, C., Valero, V., Rivero, M., … & Barriga, C. (2006). Improved circadian sleep-wake cycle in infants fed a day/night dissociated formula milk. Neuroendocrinology Letters, 27(3), 373-380.
- Gringras, P., Nir, T., Breddy, J., Frydman-Marom, A., & Findling, R. L. (2017). Efficacy and safety of pediatric prolonged-release melatonin for insomnia in children with autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 56(11), 948-957. https://doi.org/10.1016/j.jaac.2017.09.414
- Waldhauser, F., Weiszenbacher, G., Frisch, H., Zeitlhuber, U., Waldhauser, M., & Wurtman, R. J. (1984). Fall in nocturnal serum melatonin during prepuberty and pubescence. The Lancet, 323(8373), 362-365. https://doi.org/10.1016/S0140- 6736(84)90412-4
- Owens, J. A., Rosen, C. L., Mindell, J. A., & Kirchner, H. L. (2010). Use of pharmacotherapy for insomnia in child psychiatry practice: A national survey. Sleep Medicine, 11(7), 692-700. https://doi.org/10.1016/j.sleep.2009.11.015
- Bruni, O., Alonso-Alconada, D., Besag, F., Biran, V., Braam, W., Cortese, S., … & Curatolo, P. (2015). Current role of melatonin in pediatric neurology: clinical recommendations. European Journal of Paediatric Neurology, 19(2), 122-133. https://doi.org/10.1016/j.ejpn.2014.12.007
- Gupta, M., Aneja, S., & Kohli, K. (2005). Add-on melatonin improves sleep behavior in children with epilepsy: randomized, double-blind, placebo-controlled trial. Journal of Child Neurology, 20(2), 112-115. https://doi.org/10.1177/08830738050200020201
- Molina-Carballo, A., Muñoz-Hoyos, A., Sánchez-Forte, M., Uberos-Fernández, J., Moreno-Madrid, F., & Acuña-Castroviejo, D. (2007). Melatonin increases following convulsive seizures may be related to its anticonvulsant properties at physiological concentrations. Neuropediatrics, 38(3), 122-125. https://doi.org/10.1055/s-2007-985136
- Peled, N., Shorer, Z., Peled, E., & Pillar, G. (2001). Melatonin effect on seizures in children with severe neurologic deficit disorders. Epilepsia, 42(9), 1208-1210. https://doi.org/10.1046/j.1528-1157.2001.26400.x
- Skene, D. J., & Arendt, J. (2006). Human circadian rhythms: physiological and therapeutic relevance of light and melatonin. Annals of Clinical Biochemistry, 43(5), 344- 353. https://doi.org/10.1258/000456306778520142
- Härtter, S., Nordmark, A., Rose, D. M., Bertilsson, L., Tybring, G., & Laine, K. (2003). Effects of caffeine intake on the pharmacokinetics of melatonin, a probe drug for CYP1A2 activity. British Journal of Clinical Pharmacology, 56(6), 679-682. https://doi.org/10.1046/j.1365-2125.2003.01933.x
- von Bahr, C., Ursing, C., Yasui, N., Tybring, G., Bertilsson, L., & Röjdmark, S. (2000). Fluvoxamine but not citalopram increases serum melatonin in healthy subjects-an indication that cytochrome P450 CYP1A2 is involved in melatonin metabolism in man. British Journal of Clinical Pharmacology, 50(5), 415-420. https://doi.org/10.1046/j.1365- 2125.2000.00281.x
- Hartter, S., Grozinger, M., Weigmann, H., Roschke, J., & Hiemke, C. (2000). Increased bioavailability of oral melatonin after fluvoxamine coadministration. Clinical Pharmacology & Therapeutics, 67(1), 1-6. https://doi.org/10.1067/mcp.2000.103985
- Otmani, S., Demazières, A., Staner, C., Jacob, N., Nir, T., Zisapel, N., & Staner, L. (2008). Effects of prolonged-release melatonin, zolpidem, and their combination on psychomotor functions, memory recall, and driving skills in healthy middle aged and elderly volunteers. Human Psychopharmacology: Clinical and Experimental, 23(8), 693-705. https://doi.org/10.1002/hup.980
- Yasui-Furukori, N., Hidestrand, M., Spina, E., Facciolà, G., Scordo, M. G., & Tybring, G. (2001). Different enantioselective 9-hydroxylation of risperidone by the two human CYP2D6 and CYP3A4 enzymes. Drug Metabolism and Disposition, 29(10), 1263-1268.
- Granados-Fuentes, D., Prolo, L. M., Abraham, U., & Herzog, E. D. (2004). The suprachiasmatic nucleus entrains, but does not sustain, circadian rhythmicity in the olfactory bulb. Journal of Neuroscience, 24(3), 615-619. https://doi.org/10.1523/JNEUROSCI.4002-03.2004
- Zeitzer, J. M., Daniels, J. E., Duffy, J. F., Klerman, E. B., Shanahan, T. L., Dijk, D. J., & Czeisler, C. A. (1999). Do plasma melatonin concentrations decline with age? The American Journal of Medicine, 107(5), 432-436. https://doi.org/10.1016/S0002- 9343(99)00266-1
- Facciola, G., Hidestrand, M., von Bahr, C., & Tybring, G. (2001). Cytochrome P450 isoforms involved in melatonin metabolism in human liver microsomes. European Journal of Clinical Pharmacology, 56(12), 881-888. https://doi.org/10.1007/s002280000245
- Grozinger, M., Hartter, S., Wang, X., Weigmann, H., Roschke, J., Hiemke, C., … & Szegedi, A. (2000). Fluvoxamine strongly inhibits melatonin metabolism in a CYP2D6- dependent manner. Clinical Pharmacology & Therapeutics, 68(3), 224-231. https://doi.org/10.1067/mcp.2000.108850
- Lahti, T. A., Partonen, T., Kyyronen, P., Kauppinen, T., & Pukkala, E. (2008). Night-time work predisposes to non-Hodgkin lymphoma. International Journal of Cancer, 123(9), 2148-2151. https://doi.org/10.1002/ijc.23566
- Haack, M., Kraus, T., Schuld, A., Dalal, M., Koethe, D., & Pollmächer, T. (1999). Diurnal variations of cerebrospinal fluid interleukin-6 in depressed patients and healthy volunteers. Biological Psychiatry, 46(6), 840-846. https://doi.org/10.1016/S0006-3223(99)00090-9
- Malhotra, S., Sawhney, G., & Pandhi, P. (2004). The therapeutic potential of melatonin: a review of the science. MedGenMed, 6(2), 46.
- Lusardi, P., Piazza, E., & Fogari, R. (2000). Cardiovascular effects of melatonin in hypertensive patients well controlled by nifedipine: a 24-hour study. British Journal of Clinical Pharmacology, 49(5), 423-427. https://doi.org/10.1046/j.1365-2125.2000.00195.x
- Radogna, F., Diederich, M., & Ghibelli, L. (2010). Melatonin: a pleiotropic molecule regulating inflammation. Biochemical Pharmacology, 80(12), 1844-1852. https://doi.org/10.1016/j.bcp.2010.07.041
- Garfinkel, D., Laudon, M., Nof, D., & Zisapel, N. (1995). Improvement of sleep quality in elderly people by controlled-release melatonin. The Lancet, 346(8974), 541-544. https://doi.org/10.1016/S0140-6736(95)91382-3
- Richardson, G. S., Zee, P. C., Wang-Weigand, S., Rodriguez, L., & Peng, X. (2008). Circadian melatonin rhythm following treatment with ramelteon in adults with chronic insomnia. Journal of Pineal Research, 45(3), 295-304. https://doi.org/10.1111/j.1600- 079X.2008.00592.x
- Lemoine, P., Nir, T., Laudon, M., & Zisapel, N. (2007). Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. Journal of Sleep Research, 16(4), 372-380. https://doi.org/10.1111/j.1365-2869.2007.00613.x
- Paul, M. A., Gray, G. W., Lieberman, H. R., Love, R. J., Miller, J. C., Trouborst, M., & Arendt, J. (2010). Phase advance with separate and combined melatonin and light treatment. Psychopharmacology, 214(2), 515-523. https://doi.org/10.1007/s00213-010- 2059-5
- Stoschitzky, K., Sakotnik, A., Lercher, P., Zweiker, R., Maier, R., Liebmann, P., & Lindner, W. (1999). Influence of beta-blockers on melatonin release. European Journal of Clinical Pharmacology, 55(2), 111-115. https://doi.org/10.1007/s002280050604
- Scheer, F. A., Van Montfrans, G. A., van Someren, E. J., Mairuhu, G., & Buijs, R. M. (2004). Daily nighttime melatonin reduces blood pressure in male patients with essential hypertension. Hypertension, 43(2), 192-197. https://doi.org/10.1161/01.HYP.0000113293.15186.3b
- Grossman, E., Laudon, M., & Zisapel, N. (2006). Effect of melatonin on nocturnal blood pressure: meta-analysis of randomized controlled trials. Vascular Health and Risk Management, 2(4), 577-584. https://doi.org/10.2147/vhrm.2006.2.4.577
- Rechciński, T., Trzos, E., Wierzbowska-Drabik, K., Krzemińska-Pakuła, M., & Kurpesa, M. (2010). Melatonin for nondippers with coronary artery disease: assessment of blood pressure profile and heart rate variability. Hypertension Research, 33(1), 56-61. https://doi.org/10.1038/hr.2009.174
- Miller, S. C., Pandi-Perumal, S. R., Esquifino, A. I., Cardinali, D. P., & Maestroni, G. J. (2006). The role of melatonin in immuno-enhancement: potential application in cancer. International Journal of Experimental Pathology, 87(2), 81-87.
- Lissoni, P., Chilelli, M., Villa, S., Cerizza, L., & Tancini, G. (2003). Five years survival in metastatic non-small cell lung cancer patients treated with chemotherapy alone or chemotherapy and melatonin: a randomized trial. Journal of Pineal Research, 35(1), 12-15. https://doi.org/10.1034/j.1600-079X.2003.00032.x
- Srinivasan, V., Maestroni, G. J., Cardinali, D. P., Esquifino, A. I., Perumal, S. R. P., & Miller, S. C. (2005). Melatonin, immune function and aging. Immunity & Ageing, 2(1), 17. https://doi.org/10.1186/1742-4933-2-17
- Brzezinski, A. (1997). Melatonin in humans. New England Journal of Medicine, 336(3), 186-195. https://doi.org/10.1056/NEJM199701163360306
- Buscemi, N., Vandermeer, B., Hooton, N., Pandya, R., Tjosvold, L., Hartling, L., … & Vohra, S. (2005). The efficacy and safety of exogenous melatonin for primary sleep disorders: a meta-analysis. Journal of General Internal Medicine, 20(12), 1151-1158. https://doi.org/10.1111/j.1525-1497.2005.0243.x
- Seabra, M. L. V., Bignotto, M., Pinto Jr, L. R., & Tufik, S. (2000). Randomized, double blind clinical trial, controlled with placebo, of the toxicology of chronic melatonin treatment. Journal of Pineal Research, 29(4), 193-200. https://doi.org/10.1034/j.1600-079X.2000.290401.x
- Dollins, A. B., Zhdanova, I. V., Wurtman, R. J., Lynch, H. J., & Deng, M. H. (1994). Effect of inducing nocturnal serum melatonin concentrations in daytime on sleep, mood, body temperature, and performance. Proceedings of the National Academy of Sciences, 91(5), 1824-1828. https://doi.org/10.1073/pnas.91.5.1824
- Reid, K., Van den Heuvel, C., & Dawson, D. (1996). Day-time melatonin administration: effects on core temperature and sleep onset latency. Journal of Sleep Research, 5(3), 150- 154. https://doi.org/10.1046/j.1365-2869.1996.t01-1-00003.x
- Zhdanova, I. V., Wurtman, R. J., Lynch, H. J., Ives, J. R., Dollins, A. B., Morabito, C., … & Schomer, D. L. (1995). Sleep-inducing effects of low doses of melatonin ingested in the evening. Clinical Pharmacology & Therapeutics, 57(5), 552-558. https://doi.org/10.1016/0009-9236(95)90040-3
- Nave, R., Peled, R., & Lavie, P. (1995). Melatonin improves evening napping. European Journal of Pharmacology, 275(2), 213-216. https://doi.org/10.1016/0014-2999(94)00770-N
- Zhdanova, I. V., Wurtman, R. J., Regan, M. M., Taylor, J. A., Shi, J. P., & Leclair, O. U. (2001). Melatonin treatment for age-related insomnia. Journal of Clinical Endocrinology & Metabolism, 86(10), 4727-4730.
- Lemoine, P., & Zisapel, N. (2012). Prolonged-release formulation of melatonin (Circadin) for the treatment of insomnia. Expert Opinion on Pharmacotherapy, 13(6), 895- 905. https://doi.org/10.1517/14656566.2012.667076
- Arendt, J. (2005). Melatonin: characteristics, concerns, and prospects. Journal of Biological Rhythms, 20(4), 291-303. https://doi.org/10.1177/0748730405277492
- Carman, J. S., Post, R. M., Buswell, R., & Goodwin, F. K. (1976). Negative effects of melatonin on depression. The American Journal of Psychiatry, 133(10), 1181-1186. https://doi.org/10.1176/ajp.133.10.1181
- Dollins, A. B., Lynch, H. J., Wurtman, R. J., Deng, M. H., Kischka, K. U., Gleason, R. E., & Lieberman, H. R. (1993). Effects of illumination on human nocturnal serum melatonin levels and performance on tests of shift work. Health Psychology, 12(4), 319-326. https://doi.org/10.1037/0278-6133.12.4.319
- Herxheimer, A., & Petrie, K. J. (2002). Melatonin for the prevention and treatment of jet lag. Cochrane Database of Systematic Reviews, (2), CD001520. https://doi.org/10.1002/14651858.CD001520
- Wright, S. W., Lawrence, L. M., Wrenn, K. D., Haynes, M. L., Welch, L. W., & Schlack, H. M. (1998). Randomized clinical trial of melatonin after night-shift work: efficacy and neuropsychologic effects. Annals of Emergency Medicine, 32(3), 334-340. https://doi.org/10.1016/S0196-0644(98)70136-5
- Suhner, A., Schlagenhauf, P., Johnson, R., Tschopp, A., & Steffen, R. (1998). Comparative study to determine the optimal melatonin dosage form for the alleviation of jet lag. Chronobiology International, 15(6), 655-666. https://doi.org/10.3109/07420529808993201
- Petrie, K., Dawson, A. G., Thompson, L., & Brook, R. (1993). A double-blind trial of melatonin as a treatment for jet lag in international cabin crew. Biological Psychiatry, 33(7), 526-530. https://doi.org/10.1016/0006-3223(93)90007-Z
- Lewy, A. J., Ahmed, S., Jackson, J. M., & Sack, R. L. (1992). Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiology International, 9(5), 380-392. https://doi.org/10.3109/07420529209064550
- Dahlitz, M., Alvarez, B., Vignau, J., English, J., Arendt, J., & Parkes, J. D. (1991). Delayed sleep phase syndrome response to melatonin. The Lancet, 337(8750), 1121-1124. https://doi.org/10.1016/0140-6736(91)92787-3
- Sack, R. L., Lewy, A. J., Erb, D. L., Vollmer, W. M., & Singer, C. M. (1986). Human melatonin production decreases with age. Journal of Pineal Research, 3(4), 379-388. https://doi.org/10.1111/j.1600-079X.1986.tb00760.x
- Geoffriau, M., Brun, J., Chazot, G., & Claustrat, B. (1998). The physiology and pharmacology of melatonin in humans. Hormone Research in Paediatrics, 49(3-4), 136- 141. https://doi.org/10.1159/000023160
- Brusco, L. I., Márquez, M., & Cardinali, D. P. (1998). Melatonin treatment stabilizes chronobiologic and cognitive symptoms in Alzheimer’s disease. Neuroendocrinology Letters, 19(3), 111-115.
- Singer, C., Tractenberg, R. E., Kaye, J., Schafer, K., Gamst, A., Grundman, M., … & Thal, L. J. (2003). A multicenter, placebo-controlled trial of melatonin for sleep disturbance in Alzheimer’s disease. Sleep, 26(7), 893-901. https://doi.org/10.1093/sleep/26.7.893
- Haimov, I., Lavie, P., Laudon, M., Herer, P., Vigder, C., & Zisapel, N. (1995). Melatonin replacement therapy of elderly insomniacs. Sleep, 18(7), 598-603. https://doi.org/10.1093/sleep/18.7.598
- Hughes, R. J., & Badia, P. (1997). Sleep-promoting and hypothermic effects of daytime melatonin administration in humans. Sleep, 20(2), 124-131. https://doi.org/10.1093/sleep/20.2.124
- Kunz, D., Mahlberg, R., Müller, C., Tilmann, A., & Bes, F. (2004). Melatonin in patients with reduced REM sleep duration: two randomized controlled trials. Journal of Clinical Endocrinology & Metabolism, 89(1), 128-134. https://doi.org/10.1210/jc.2002-021057
- Garfinkel, D., Zisapel, N., Wainstein, J., & Laudon, M. (1999). Facilitation of benzodiazepine discontinuation by melatonin: a new clinical approach. Archives of Internal Medicine, 159(20), 2456-2460. https://doi.org/10.1001/archinte.159.20.2456
- Dagan, Y., Zisapel, N., Nof, D., Laudon, M., & Atsmon, J. (1997). Rapid reversal of tolerance to benzodiazepine hypnotics by treatment with oral melatonin: a case report. European Neuropsychopharmacology, 7(2), 157-160. https://doi.org/10.1016/S0924-977X(96)00401-6
- Kayumov, L., Brown, G., Jindal, R., Buttoo, K., & Shapiro, C. M. (2001). A randomized, double-blind, placebo-controlled crossover study of the effect of exogenous melatonin on delayed sleep phase syndrome. Psychosomatic Medicine, 63(1), 40-48. https://doi.org/10.1097/00006842-200101000-00006
- Luboshitzky, R., Shen-Orr, Z., Nave, R., Lavi, S., & Lavie, P. (2001). Melatonin administration alters semen quality in healthy men. Journal of Andrology, 22(5), 747-750. https://doi.org/10.1002/j.1939-4640.2001.tb02575.x
- Voordouw, B. C., Euser, R., Verdonk, R. E., Alberda, B. T., de Jong, F. H., Drogendijk, A. C., … & Cohen, M. (1992). Melatonin and melatonin-progestin combinations alter pituitary ovarian function in women and can inhibit ovulation. Journal of Clinical Endocrinology & Metabolism, 74(1), 108-117. https://doi.org/10.1210/jcem.74.1.1727807
- Bellipanni, G., Bianchi, P., Pierpaoli, W., Bulian, D., & Ilyia, E. (2001). Effects of melatonin in perimenopausal and menopausal women: a randomized and placebo controlled study. Experimental Gerontology, 36(2), 297-310. https://doi.org/10.1016/S0531-5565(00)00217-5
- Valcavi, R., Zini, M., Maestroni, G. J., Conti, A., & Portioli, I. (1993). Melatonin stimulates growth hormone secretion through pathways other than the growth hormone releasing hormone. Clinical Endocrinology, 39(2), 193-199. https://doi.org/10.1111/j.1365- 2265.1993.tb01773.x
- Reiter, R. J., Tan, D. X., Korkmaz, A., & Rosales-Corral, S. A. (2014). Melatonin and stable circadian rhythms optimize maternal, placental and fetal physiology. Human Reproduction Update, 20(2), 293-307. https://doi.org/10.1093/humupd/dmt054
- Kivela, A., Kauppila, A., Ylostalo, P., Vakkuri, O., & Leppaluoto, J. (1988). Seasonal, menstrual and circadian secretions of melatonin, gonadotropins and prolactin in women. Acta Physiologica Scandinavica, 132(3), 321-327. https://doi.org/10.1111/j.1748- 1716.1988.tb08336.x
- Voiculescu, S. E., Zygouropoulos, N., Zahiu, C. D., & Zagrean, A. M. (2014). Role of melatonin in embryo fetal development. Journal of Medicine and Life, 7(4), 488-492.
- Hobson, S. R., Gurusinghe, S., Lim, R., Alers, N. O., Miller, S. L., Kingdom, J. C., & Wallace, E. M. (2018). Melatonin improves endothelial function in vitro and prolongs pregnancy in women with early-onset preeclampsia. Journal of Pineal Research, 65(3), e12508. https://doi.org/10.1111/jpi.12508
- Mendez, N., Halabi, D., Spichiger, C., Salazar, E. R., Vergara, K., Alonso-Alconada, D., … & Torres-Farfan, C. (2016). Gestational chronodisruption impairs hippocampal expression of NMDA receptor subunits Grin1b/Grin3a and spatial memory in the adult offspring. PLoS One, 11(2), e0150190. https://doi.org/10.1371/journal.pone.0150190
- Richter, H. G., Hansell, J. A., Raut, S., & Giussani, D. A. (2009). Melatonin improves placental efficiency and birth weight and increases the placental expression of antioxidant enzymes in undernourished pregnancy. Journal of Pineal Research, 46(4), 357-364. https://doi.org/10.1111/j.1600-079X.2009.00671.x
- Miller, S. L., Yawno, T., Alers, N. O., Castillo-Melendez, M., Supramaniam, V. G., VanZyl, N., … & Wallace, E. M. (2014). Antenatal antioxidant treatment with melatonin to decrease newborn neurodevelopmental deficits and brain injury caused by fetal growth restriction. Journal of Pineal Research, 56(3), 283-294. https://doi.org/10.1111/jpi.12121
- Aly, H., Elmahdy, H., El-Dib, M., Rowisha, M., Awny, M., El-Gohary, T., … & Blennow, M. (2015). Melatonin use for neuroprotection in perinatal asphyxia: a randomized controlled pilot study. Journal of Perinatology, 35(3), 186-191. https://doi.org/10.1038/jp.2014.186
- Okatani, Y., Okamoto, K., Hayashi, K., Wakatsuki, A., Tamura, S., & Sagara, Y. (1998). Maternal-fetal transfer of melatonin in pregnant women near term. Journal of Pineal Research, 25(3), 129-134. https://doi.org/10.1111/j.1600-079X.1998.tb00549.x
- Ferreira, D. S., Amaral, F. G., Mesquita, C. C., Barbosa, A. P., Lellis-Santos, C., Turati, A. O., … & Cipolla-Neto, J. (2012). Maternal melatonin programs the daily pattern of energy metabolism in adult offspring. PLoS One, 7(6), e38795. https://doi.org/10.1371/journal.pone.0038795
- Torres-Farfan, C., Valenzuela, F. J., Mondaca, M., Valenzuela, G. J., Krause, B., Herrera, E. A., … & Seron-Ferre, M. (2008). Evidence of a role for melatonin in fetal sheep physiology: direct actions of melatonin on fetal cerebral artery, brown adipose tissue and adrenal gland. Journal of Physiology, 586(16), 4017-4027. https://doi.org/10.1113/jphysiol.2008.154351
- Campino, C., Valenzuela, F. J., Torres-Farfan, C., Reynolds, H. E., Abarzua-Catalan, L., Arteaga, E., … & Seron-Ferre, M. (2011). Melatonin exerts direct inhibitory actions on ACTH responses in the human adrenal gland. Hormone and Metabolic Research, 43(5), 337-342. https://doi.org/10.1055/s-0031-1271693
- Lanoix, D., Beghdadi, H., Lafond, J., & Vaillancourt, C. (2008). Human placental trophoblasts synthesize melatonin and express its receptors. Journal of Pineal Research, 45(1), 50-60. https://doi.org/10.1111/j.1600-079X.2008.00555.x
- Tamura, H., Nakamura, Y., Korkmaz, A., Manchester, L. C., Tan, D. X., Sugino, N., & Reiter, R. J. (2009). Melatonin and the ovary: physiological and pathophysiological implications. Fertility and Sterility, 92(1), 328-343. https://doi.org/10.1016/j.fertnstert.2008.05.016
- Nakamura, Y., Tamura, H., Kashida, S., Takayama, H., Yamagata, Y., Karube, A., … & Sugino, N. (2001). Changes of serum melatonin level and its relationship to feto-placental unit during pregnancy. Journal of Pineal Research, 30(1), 29-33 https://doi.org/10.1034/j.1600-079X.2001.300104.x
- Sagrillo-Fagundes, L., Assuncao Salustiano, E. M., Yen, P. W., Soliman, A., & Vaillancourt, C. (2014). Melatonin in pregnancy: effects on brain development and CNS programming disorders. Current Pharmaceutical Design, 20(28), 4748-4756. https://doi.org/10.2174/1381612820666140130205900
- Pien, G. W., & Schwab, R. J. (2004). Sleep disorders during pregnancy. Sleep, 27(7), 1405-1417. https://doi.org/10.1093/sleep/27.7.1405
- Facco, F. L., Kramer, J., Ho, K. H., Zee, P. C., & Grobman, W. A. (2010). Sleep disturbances in pregnancy. Obstetrics & Gynecology, 115(1), 77-83. https://doi.org/10.1097/AOG.0b013e3181c4f8ec
- Mindell, J. A., Cook, R. A., & Nikolovski, J. (2015). Sleep patterns and sleep disturbances across pregnancy. Sleep Medicine, 16(4), 483-488. https://doi.org/10.1016/j.sleep.2014.12.006
- Okun, M. L., Hanusa, B. H., Hall, M., & Wisner, K. L. (2009). Sleep complaints in late pregnancy and the recurrence of postpartum depression. Behavioral Sleep Medicine, 7(2), 106-117. https://doi.org/10.1080/15402000902762394
- Committee on Obstetric Practice. (2013). Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. Obstetrics & Gynecology, 130(2), e102-e109. https://doi.org/10.1097/AOG.0000000000002237
- American College of Obstetricians and Gynecologists. (2019). Practice bulletin no. 202: gestational hypertension and preeclampsia. Obstetrics & Gynecology, 133(1), e1-e25. https://doi.org/10.1097/AOG.0000000000003018
- Ray, J. G., Vermeulen, M. J., Bharatha, A., Montanera, W. J., & Park, A. L. (2016). Association between MRI exposure during pregnancy and fetal and childhood outcomes. JAMA, 316(9), 952-961. https://doi.org/10.1001/jama.2016.12126
- Illnerova, H., Buresova, M., & Presl, J. (1993). Melatonin rhythm in human milk. Journal of Clinical Endocrinology & Metabolism, 77(3), 838-841. https://doi.org/10.1210/jcem.77.3.8370707
- Cohen Engler, A., Hadash, A., Shehadeh, N., & Pillar, G. (2012). Breastfeeding may improve nocturnal sleep and reduce infantile colic: potential role of breast milk melatonin. European Journal of Pediatrics, 171(4), 729-732. https://doi.org/10.1007/s00431-011- 1659-3
- Cubero, J., Valero, V., Sanchez, J., Rivero, M., Parvez, H., Rodriguez, A. B., & Barriga, C. (2005). The circadian rhythm of tryptophan in breast milk affects the rhythms of 6- sulfatoxymelatonin and sleep in newborn. Neuroendocrinology Letters, 26(6), 657-661.
- Aparicio, S., Garau, C., Esteban, S., Nicolau, M. C., Rivero, M., & Rial, R. (2007). Chrononutrition: use of dissociated day/night infant milk formulas to improve the development of the wake-sleep rhythms. Effects of tryptophan. Nutritional Neuroscience, 10(3-4), 137-143. https://doi.org/10.1080/10284150701722339
- Honkus, V. L. (1998). Breast milk jaundice. In Hematology/Oncology Clinics of North America (Vol. 12, No. 1, pp. 41-51). WB Saunders. https://doi.org/10.1016/S0889-8588(05)70528-4
- Auger, R. R., Burgess, H. J., Emens, J. S., Deriy, L. V., Thomas, S. M., & Sharkey, K. M. (2015). Clinical practice guideline for the treatment of intrinsic circadian rhythm sleep wake disorders: advanced sleep-wake phase disorder (ASWPD), delayed sleep-wake phase disorder (DSWPD), non-24-hour sleep-wake rhythm disorder (N24SWD), and irregular sleep-wake rhythm disorder (ISWRD). Journal of Clinical Sleep Medicine, 11(10), 1199-1236. https://doi.org/10.5664/jcsm.5100
- Buscemi, N., Vandermeer, B., Hooton, N., Pandya, R., Tjosvold, L., Hartling, L., … & Vohra, S. (2006). Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ, 332(7538), 385- 393. https://doi.org/10.1136/bmj.38731.532766.F6
- DeMuro, R. L., Nafziger, A. N., Blask, D. E., Menhinick, A. M., & Bertino Jr, J. S. (2000). The absolute bioavailability of oral melatonin. Journal of Clinical Pharmacology, 40(7), 781- 784. https://doi.org/10.1177/00912700022009422
- Buscemi, N., Vandermeer, B., Hooton, N., Pandya, R., Tjosvold, L., Hartling, L., … & Vohra, S. (2005). The efficacy and safety of exogenous melatonin for primary sleep disorders: a meta-analysis. Journal of General Internal Medicine, 20(12), 1151-1158. https://doi.org/10.1111/j.1525-1497.2005.0243.x
- van Geijlswijk, I. M., Korzilius, H. P., & Smits, M. G. (2010). The use of exogenous melatonin in delayed sleep phase disorder: a meta-analysis. Sleep, 33(12), 1605-1614. https://doi.org/10.1093/sleep/33.12.1605
- Zhdanova, I. V., Wurtman, R. J., Lynch, H. J., Ives, J. R., Dollins, A. B., Morabito, C., … & Schomer, D. L. (1995). Sleep-inducing effects of low doses of melatonin ingested in the evening. Clinical Pharmacology & Therapeutics, 57(5), 552-558. https://doi.org/10.1016/0009-9236(95)90040-3
- Burgess, H. J., Revell, V. L., & Eastman, C. I. (2008). A three pulse phase response curve to three milligrams of melatonin in humans. Journal of Physiology, 586(2), 639-647. https://doi.org/10.1113/jphysiol.2007.143180
- Zhdanova, I. V., Wurtman, R. J., Regan, M. M., Taylor, J. A., Shi, J. P., & Leclair, O. U. (2001). Melatonin treatment for age-related insomnia. Journal of Clinical Endocrinology & Metabolism, 86(10), 4727-4730. https://doi.org/10.1210/jcem.86.10.7901
- Lewy, A. J., Ahmed, S., Jackson, J. M., & Sack, R. L. (1992). Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiology International, 9(5), 380-392. https://doi.org/10.3109/07420529209064550
- Mundey, K., Benloucif, S., Harsanyi, K., Dubocovich, M. L., & Zee, P. C. (2005). Phase dependent treatment of delayed sleep phase syndrome with melatonin. Sleep, 28(10), 1271-1278. https://doi.org/10.1093/sleep/28.10.1271
- Herxheimer, A., & Petrie, K. J. (2002). Melatonin for the prevention and treatment of jet lag. Cochrane Database of Systematic Reviews, (2), CD001520. https://doi.org/10.1002/14651858.CD001520
- Eastman, C. I., Gazda, C. J., Burgess, H. J., Crowley, S. J., & Fogg, L. F. (2005). Advancing circadian rhythms before eastward flight: a strategy to prevent or reduce jet lag. Sleep, 28(1), 33-44. https://doi.org/10.1093/sleep/28.1.33
- Paul, M. A., Gray, G. W., Lieberman, H. R., Love, R. J., Miller, J. C., Trouborst, M., & Arendt, J. (2010). Phase advance with separate and combined melatonin and light treatment. Psychopharmacology, 214(2), 515-523. https://doi.org/10.1007/s00213-010- 2059-5
- Revell, V. L., Burgess, H. J., Gazda, C. J., Smith, M. R., Fogg, L. F., & Eastman, C. I. (2006). Advancing human circadian rhythms with afternoon melatonin and morning intermittent bright light. Journal of Clinical Endocrinology & Metabolism, 91(1), 54-59. https://doi.org/10.1210/jc.2005-1009
- Arendt, J. (2010). Shift work: coping with the biological clock. Occupational Medicine, 60(1), 10-20. https://doi.org/10.1093/occmed/kqp162
- Crowley, S. J., Lee, C., Tseng, C. Y., Fogg, L. F., & Eastman, C. I. (2003). Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work. Journal of Biological Rhythms, 18(6), 513-523. https://doi.org/10.1177/0748730403258422
- Sharkey, K. M., & Eastman, C. I. (2002). Melatonin phase shifts human circadian rhythms in a placebo-controlled simulated night-work study. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 282(2), R454-R463. https://doi.org/10.1152/ajpregu.00273.2001
- Wright Jr, K. P., Bogan, R. K., & Wyatt, J. K. (2013). Shift work sleep disorder: epidemiology and management. CNS Drugs, 27(5), 355-365. https://doi.org/10.1007/s40263-013-0057-1
- Karasek, M. (2004). Melatonin, human aging, and age-related diseases. Experimental Gerontology, 39(11-12), 1723-1729. https://doi.org/10.1016/j.exger.2004.04.012
- Monti, J. M., BaHammam, A. S., Pandi-Perumal, S. R., Bromundt, V., Spence, D. W., Cardinali, D. P., & Brown, G. M. (2013). Sleep and circadian rhythm dysregulation in schizophrenia. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 43, 209- 216. https://doi.org/10.1016/j.pnpbp.2012.12.021
- Haimov, I., Lavie, P., Laudon, M., Herer, P., Vigder, C., & Zisapel, N. (1995). Melatonin replacement therapy of elderly insomniacs. Sleep, 18(7), 598-603. https://doi.org/10.1093/sleep/18.7.598
- By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel. (2015). American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society, 63(11), 2227- 2246. https://doi.org/10.1111/jgs.13702
- Härtter, S., Grözinger, M., Weigmann, H., Röschke, J., & Hiemke, C. (2000). Increased bioavailability of oral melatonin after fluvoxamine coadministration. Clinical Pharmacology & Therapeutics, 67(1), 1-6. https://doi.org/10.1067/mcp.2000.103985
- Young, I. M., Leone, R. M., Francis, P., Stovell, P., & Silman, R. E. (1985). Melatonin is metabolized to N-acetyl serotonin and 6-hydroxymelatonin in man. Journal of Clinical Endocrinology & Metabolism, 60(1), 114-119. https://doi.org/10.1210/jcem-60-1-114
- Ma, X., Idle, J. R., Krausz, K. W., & Gonzalez, F. J. (2005). Metabolism of melatonin by human cytochromes p450. Drug Metabolism and Disposition, 33(4), 489-494. https://doi.org/10.1124/dmd.104.002410
- Rajaratnam, S. M., Middleton, B., Stone, B. M., Arendt, J., & Dijk, D. J. (2004). Melatonin advances the circadian timing of EEG sleep and directly facilitates sleep without altering its duration in extended sleep opportunities in humans. Journal of Physiology, 561(1), 339- 351. https://doi.org/10.1113/jphysiol.2004.073742
- Gorfine, T., & Zisapel, N. (2009). Late evening brain activation patterns and their relation to the internal biological time, melatonin, and homeostatic sleep debt. Human Brain Mapping, 30(2), 541-552. https://doi.org/10.1002/hbm.20525
- Arendt, J. (2000). Melatonin, circadian rhythms, and sleep. New England Journal of Medicine, 343(15), 1114-1116. https://doi.org/10.1056/NEJM200010123431510
- Lemoine, P., Nir, T., Laudon, M., & Zisapel, N. (2007). Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. Journal of Sleep Research, 16(4), 372-380. https://doi.org/10.1111/j.1365-2869.2007.00613.x
- Andersen, L. P., Gögenur, I., Rosenberg, J., & Reiter, R. J. (2016). The safety of melatonin in humans. Clinical Drug Investigation, 36(3), 169-175. https://doi.org/10.1007/s40261-015-0368-5
- Maharaj, D. S., Glass, B. D., Daya, S., & Maharaj, V. (2003). Melatonin: photostability of solid dosage forms. Journal of Pineal Research, 35(3), 215-221. https://doi.org/10.1034/j.1600-079X.2003.00077.x
- United States Pharmacopeial Convention. (2019). General chapter <797> pharmaceutical compounding-sterile preparations. USP 42-NF 37. United States Pharmacopeial Convention.
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. (2003). Stability testing of new drug substances and products Q1A(R2). ICH Harmonised Tripartite Guideline
- Maharaj, D. S., Glass, B. D., & Daya, S. (2003). Melatonin: degradation and metabolite identification. Journal of Pineal Research, 34(4), 257-262. https://doi.org/10.1034/j.1600- 079X.2003.00039.x
- U.S. Food and Drug Administration. (2016). Guidance for industry: container closure systems for packaging human drugs and biologics. Chemistry, Manufacturing, and Controls Documentation. FDA.
- World Health Organization. (2003). Stability testing of active pharmaceutical ingredients and finished pharmaceutical products. WHO Technical Report Series, No. 953, Annex 2.
- Maharaj, D. S., Anoopkumar-Dukie, S., Glass, B. D., Antunes, E. M., Lack, B., Walker, R. B., & Daya, S. (2002). The identification of the UV degradants of melatonin and their ability to scavenge free radicals. Journal of Pineal Research, 32(4), 257-261. https://doi.org/10.1034/j.1600-079X.2002.01866.x
- Bangha, E., Elsner, P., & Kistler, G. S. (1997). Suppression of UV-induced erythema by topical treatment with melatonin (N-acetyl-5-methoxytryptamine). Influence of the application time point. Dermatology Online Journal, 3(2), 4.
- International Association of Compounding Pharmacists. (2018). Compounding quality assurance guidelines. Professional Compounding Centers of America.
- National Association of Boards of Pharmacy. (2019). Model state pharmacy act and model rules of the national association of boards of pharmacy. NABP.
- Allen, L. V. (2016). The art, science, and technology of pharmaceutical compounding (4th ed.). American Pharmacists Association.
- Thompson, C. A. (2014). USP proposes new compounding standards. American Journal of Health-System Pharmacy, 71(14), 1186-1188. https://doi.org/10.2146/news140059
- U.S. Food and Drug Administration. (2013). Guidance for industry: interim policy on compounding using bulk drug substances under section 503A of the Federal Food, Drug, and Cosmetic Act. FDA.
- Handbook of Pharmaceutical Excipients. (2017). Pharmaceutical Press and American Pharmacists Association.
- International Pharmaceutical Excipients Council. (2015). Good manufacturing practices guide for pharmaceutical excipients. IPEC.
- Pharmacy Compounding Accreditation Board. (2018). Standards for the accreditation of pharmacy compounding. PCAB.
- United States Pharmacopeial Convention. (2018). General chapter <795> pharmaceutical compounding-nonsterile preparations. USP 41-NF 36.
- Centers for Disease Control and Prevention. (2019). Guidelines for hand hygiene in health-care settings. MMWR Recommendations and Reports, 51(RR-16), 1-45.
- Thompson, C. A. (2013). Compounding pharmacies report adverse events to FDA. American Journal of Health-System Pharmacy, 70(19), 1669-1670. https://doi.org/10.2146/news130079
- National Institute for Occupational Safety and Health. (2016). Criteria for a recommended standard: occupational exposure to hazardous drugs in healthcare settings. DHHS (NIOSH) Publication No. 2016-161.
- International Society for Pharmaceutical Engineering. (2017). Good practice guide: containment systems for the handling of highly potent compounds. ISPE.
- Glass Packaging Institute. (2018). Glass container guidelines for pharmaceutical applications. GPI Technical Bulletin.
- Plastic Industry Association. (2019). Guidelines for pharmaceutical packaging materials. PIA Technical Report.
- Child-Resistant Packaging Act of 1970. (2019). Code of Federal Regulations, Title 16, Part 1700.
- Drug Enforcement Administration. (2018). Disposal of controlled substances. Code of Federal Regulations, Title 21, Part 1317.
- Environmental Protection Agency. (2019). Guidelines for pharmaceutical waste management. EPA Office of Resource Conservation and Recovery.
- U.S. Food and Drug Administration. (2014). Guidance for industry: beyond use dating for non-sterile compounded drug preparations. FDA Draft Guidance.
- United States Pharmacopeial Convention. (2019). General information chapter <1191> stability considerations in dispensing practice. USP 42-NF 37.
- Institute for Safe Medication Practices. (2018). Guidelines for safe medication disposal. ISMP Medication Safety Alert.
- Drug Enforcement Administration. (2019). National prescription drug take back day. DEA Office of Diversion Control.
- International Air Transport Association. (2019). Dangerous goods regulations for pharmaceutical transportation. IATA DGR.
- Transportation Security Administration. (2019). Medication guidelines for air travel. TSA.
- International Civil Aviation Organization. (2018). Technical instructions for the safe transport of dangerous goods by air. ICAO Doc 9284.
- Aerospace Medical Association. (2017). Medical guidelines for airline travel (2nd ed.). Aviation, Space, and Environmental Medicine, 74(5), A1-A19.
- Zhdanova, I. V., Wurtman, R. J., Lynch, H. J., Ives, J. R., Dollins, A. B., Morabito, C., … & Schomer, D. L. (1995). Sleep-inducing effects of low doses of melatonin ingested in the evening. Clinical Pharmacology & Therapeutics, 57(5), 552-558. https://doi.org/10.1016/0009-9236(95)90040-3
- Reid, K., Van den Heuvel, C., & Dawson, D. (1996). Day-time melatonin administration: effects on core temperature and sleep onset latency. Journal of Sleep Research, 5(3), 150- 154. https://doi.org/10.1046/j.1365-2869.1996.t01-1-00003.x
- Fourtillan, J. B., Brisson, A. M., Gobin, P., Ingrand, I., Decourt, J. P., & Girault, J. (2000). Bioavailability of melatonin in humans after daytime administration of D(7) melatonin. Biopharmaceutics & Drug Disposition, 21(1), 15-22. https://doi.org/10.1002/1099- 081X(200001)21:1<15::AID-BDD215>3.0.CO;2-H
- Nave, R., Peled, R., & Lavie, P. (1995). Melatonin improves evening napping. European Journal of Pharmacology, 275(2), 213-216. https://doi.org/10.1016/0014-2999(94)00770-N
- Hughes, R. J., & Badia, P. (1997). Sleep-promoting and hypothermic effects of daytime melatonin administration in humans. Sleep, 20(2), 124-131. https://doi.org/10.1093/sleep/20.2.124
- Dollins, A. B., Zhdanova, I. V., Wurtman, R. J., Lynch, H. J., & Deng, M. H. (1994). Effect of inducing nocturnal serum melatonin concentrations in daytime on sleep, mood, body temperature, and performance. Proceedings of the National Academy of Sciences, 91(5), 1824-1828. https://doi.org/10.1073/pnas.91.5.1824
- Lewy, A. J., Ahmed, S., Jackson, J. M., & Sack, R. L. (1992). Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiology International, 9(5), 380-392. https://doi.org/10.3109/07420529209064550
- Sateia, M. J., Buysse, D. J., Krystal, A. D., Neubauer, D. N., & Heald, J. L. (2017). Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults. Journal of Clinical Sleep Medicine, 13(2), 307-349. https://doi.org/10.5664/jcsm.6470
- Mundey, K., Benloucif, S., Harsanyi, K., Dubocovich, M. L., & Zee, P. C. (2005). Phase dependent treatment of delayed sleep phase syndrome with melatonin. Sleep, 28(10), 1271-1278. https://doi.org/10.1093/sleep/28.10.1271
- Herxheimer, A., & Petrie, K. J. (2002). Melatonin for the prevention and treatment of jet lag. Cochrane Database of Systematic Reviews, (2), CD001520. https://doi.org/10.1002/14651858.CD001520
- Seabra, M. L. V., Bignotto, M., Pinto Jr, L. R., & Tufik, S. (2000). Randomized, double blind clinical trial, controlled with placebo, of the toxicology of chronic melatonin treatment. Journal of Pineal Research, 29(4), 193-200. https://doi.org/10.1034/j.1600-079X.2000.290401.x
- Lemoine, P., Nir, T., Laudon, M., & Zisapel, N. (2007). Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. Journal of Sleep Research, 16(4), 372-380. https://doi.org/10.1111/j.1365-2869.2007.00613.x
- Auger, R. R., Burgess, H. J., Emens, J. S., Deriy, L. V., Thomas, S. M., & Sharkey, K. M. (2015). Clinical practice guideline for the treatment of intrinsic circadian rhythm sleep wake disorders. Journal of Clinical Sleep Medicine, 11(10), 1199-1236. https://doi.org/10.5664/jcsm.5100
- American Academy of Sleep Medicine. (2014). International classification of sleep disorders (3rd ed.). American Academy of Sleep Medicine.
- Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J., & Hall, M. H. (2015). The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Medicine Reviews, 22, 23-36. https://doi.org/10.1016/j.smrv.2014.10.001
- Andersen, L. P., Gögenur, I., Rosenberg, J., & Reiter, R. J. (2016). The safety of melatonin in humans. Clinical Drug Investigation, 36(3), 169-175. https://doi.org/10.1007/s40261-015-0368-5
- American Association of Poison Control Centers. (2019). Annual report of the National Poison Data System. Clinical Toxicology, 57(12), 1220-1413. https://doi.org/10.1080/15563650.2019.1677022
- Brzezinski, A. (1997). Melatonin in humans. New England Journal of Medicine, 336(3), 186-195. https://doi.org/10.1056/NEJM199701163360306
- Pandi-Perumal, S. R., Trakht, I., Srinivasan, V., Spence, D. W., Maestroni, G. J., Zisapel, N., & Cardinali, D. P. (2008). Physiological effects of melatonin: role of melatonin receptors and signal transduction pathways. Progress in Neurobiology, 85(3), 335-353. https://doi.org/10.1016/j.pneurobio.2008.04.001
- National Capital Poison Center. (2018). Poison prevention and safety tips. NCPC Educational Materials.
- National Highway Traffic Safety Administration. (2017). Drug and alcohol crash risk. NHTSA Traffic Safety Facts. DOT HS 812 355.
- Gringras, P., Nir, T., Breddy, J., Frydman-Marom, A., & Findling, R. L. (2017). Efficacy and safety of pediatric prolonged-release melatonin for insomnia in children with autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 56(11), 948-957. https://doi.org/10.1016/j.jaac.2017.09.414
- Härtter, S., Grözinger, M., Weigmann, H., Röschke, J., & Hiemke, C. (2000). Increased bioavailability of oral melatonin after fluvoxamine coadministration. Clinical Pharmacology & Therapeutics, 67(1), 1-6. https://doi.org/10.1067/mcp.2000.103985
- von Bahr, C., Ursing, C., Yasui, N., Tybring, G., Bertilsson, L., & Röjdmark, S. (2000). Fluvoxamine but not citalopram increases serum melatonin in healthy subjects. British Journal of Clinical Pharmacology, 50(5), 415-420. https://doi.org/10.1046/j.1365- 2125.2000.00281.x
- Lusardi, P., Piazza, E., & Fogari, R. (2000). Cardiovascular effects of melatonin in hypertensive patients well controlled by nifedipine: a 24-hour study. British Journal of Clinical Pharmacology, 49(5), 423-427. https://doi.org/10.1046/j.1365-2125.2000.00195.x 232.Richardson, G. S., Zee, P. C., Wang-Weigand, S., Rodriguez, L., & Peng, X. (2008). Circadian melatonin rhythm following treatment with ramelteon in adults with chronic insomnia. Journal of Pineal Research, 45(3), 295-304. https://doi.org/10.1111/j.1600- 079X.2008.00592.x
- Garfinkel, D., Laudon, M., Nof, D., & Zisapel, N. (1995). Improvement of sleep quality in elderly people by controlled-release melatonin. The Lancet, 346(8974), 541-544. https://doi.org/10.1016/S0140-6736(95)91382-3
- Grozinger, M., Hartter, S., Wang, X., Weigmann, H., Roschke, J., Hiemke, C., … & Szegedi, A. (2000). Fluvoxamine strongly inhibits melatonin metabolism in a CYP2D6- dependent manner. Clinical Pharmacology & Therapeutics, 68(3), 224-231. https://doi.org/10.1067/mcp.2000.108850
- Stoschitzky, K., Sakotnik, A., Lercher, P., Zweiker, R., Maier, R., Liebmann, P., & Lindner, W. (1999). Influence of beta-blockers on melatonin release. European Journal of Clinical Pharmacology, 55(2), 111-115. https://doi.org/10.1007/s002280050604
- Institute for Safe Medication Practices. (2019). High-alert medications in acute care settings. ISMP Medication Safety Alert, 24(3), 1-6.
- U.S. Food and Drug Administration. (2018). MedWatch: the FDA safety information and adverse event reporting program. FDA Safety Communications.
- Otmani, S., Demazières, A., Staner, C., Jacob, N., Nir, T., Zisapel, N., & Staner, L. (2008). Effects of prolonged-release melatonin, zolpidem, and their combination on psychomotor functions, memory recall, and driving skills in healthy middle aged and
- elderly volunteers. Human Psychopharmacology: Clinical and Experimental, 23(8), 693- 705. https://doi.org/10.1002/hup.980
- Lemoine, P., & Zisapel, N. (2012). Prolonged-release formulation of melatonin (Circadin) for the treatment of insomnia. Expert Opinion on Pharmacotherapy, 13(6), 895- 905. https://doi.org/10.1517/14656566.2012.667076
- Paul, M. A., Gray, G. W., Lieberman, H. R., Love, R. J., Miller, J. C., Trouborst, M., & Arendt, J. (2010). Phase advance with separate and combined melatonin and light treatment. Psychopharmacology, 214(2), 515-523. https://doi.org/10.1007/s00213-010- 2059-5
- Leufkens, T. R., Ramaekers, J. G., de Weerd, A. W., Riedel, W. J., & Vermeeren, A. (2014). Residual effects of zopiclone 7.5 mg on highway driving performance in insomnia patients and healthy controls: a placebo controlled crossover study. Psychopharmacology, 231(14), 2785-2798. https://doi.org/10.1007/s00213-014-3490-9
- Rajaratnam, S. M., Polymeropoulos, M. H., Fisher, D. M., Roth, T., Scott, C., Birznieks, G., & Klerman, E. B. (2009). Melatonin agonist tasimelteon for transient insomnia after sleep-time shift: two randomised controlled multicentre trials. The Lancet, 373(9662), 482- 491. https://doi.org/10.1016/S0140-6736(08)61812-7
- National Institute for Occupational Safety and Health. (2015). Criteria for a recommended standard: occupational exposure to shift work. DHHS (NIOSH) Publication No. 2015-107.
- Transportation Security Administration. (2018). Medication guidelines for commercial drivers. TSA Commercial Vehicle Operations.
- Federal Motor Carrier Safety Administration. (2017). Medical examiner handbook. FMCSA-DOT Medical Programs.
- Occupational Safety and Health Administration. (2019). Guidelines for workplace safety and health programs. OSHA Publication 3885.
- Garfinkel, D., Zisapel, N., Wainstein, J., & Laudon, M. (1999). Facilitation of benzodiazepine discontinuation by melatonin: a new clinical approach. Archives of Internal Medicine, 159(20), 2456-2460. https://doi.org/10.1001/archinte.159.20.2456
- Dagan, Y., Zisapel, N., Nof, D., Laudon, M., & Atsmon, J. (1997). Rapid reversal of tolerance to benzodiazepine hypnotics by treatment with oral melatonin: a case report. European Neuropsychopharmacology, 7(2), 157-160. https://doi.org/10.1016/S0924-977X(96)00401-6
- Kunz, D., Mahlberg, R., Müller, C., Tilmann, A., & Bes, F. (2004). Melatonin in patients with reduced REM sleep duration: two randomized controlled trials. Journal of Clinical Endocrinology & Metabolism, 89(1), 128-134. https://doi.org/10.1210/jc.2002-021057
- Kayumov, L., Brown, G., Jindal, R., Buttoo, K., & Shapiro, C. M. (2001). A randomized, double-blind, placebo-controlled crossover study of the effect of exogenous melatonin on delayed sleep phase syndrome. Psychosomatic Medicine, 63(1), 40-48. https://doi.org/10.1097/00006842-200101000-00006
- Wright, S. W., Lawrence, L. M., Wrenn, K. D., Haynes, M. L., Welch, L. W., & Schlack, H. M. (1998). Randomized clinical trial of melatonin after night-shift work: efficacy and neuropsychologic effects. Annals of Emergency Medicine, 32(3), 334-340. https://doi.org/10.1016/S0196-0644(98)70136-5
- Arendt, J. (2005). Melatonin: characteristics, concerns, and prospects. Journal of Biological Rhythms, 20(4), 291-303. https://doi.org/10.1177/0748730405277492
- Schutte-Rodin, S., Broch, L., Buysse, D., Dorsey, C., & Sateia, M. (2008). Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine, 4(5), 487-504. https://doi.org/10.5664/jcsm.27286
- Morin, C. M., Bootzin, R. R., Buysse, D. J., Edinger, J. D., Espie, C. A., & Lichstein, K. L. (2006). Psychological and behavioral treatment of insomnia: update of the recent evidence. Sleep, 29(11), 1398-1414. https://doi.org/10.1093/sleep/29.11.1398
- Stepanski, E. J., & Wyatt, J. K. (2003). Use of sleep hygiene in the treatment of insomnia. Sleep Medicine Reviews, 7(3), 215-225. https://doi.org/10.1053/smrv.2001.0246
- Richardson, G. S. (2005). The human circadian system in normal and disordered sleep. Journal of Clinical Psychiatry, 66(Suppl 9), 3-9.
- Dubocovich, M. L., & Markowska, M. (2005). Functional MT1 and MT2 melatonin receptors in mammals. Endocrine, 27(2), 101-110. https://doi.org/10.1385/ENDO:27:2:101
- Winkelman, J. W. (2015). Insomnia disorder. New England Journal of Medicine, 373(15), 1437-1444. https://doi.org/10.1056/NEJMcp1412740
- Buscemi, N., Vandermeer, B., Hooton, N., Pandya, R., Tjosvold, L., Hartling, L., … & Vohra, S. (2006). Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ, 332(7538), 385- 393. https://doi.org/10.1136/bmj.38731.532766.F6
- Zhdanova, I. V., Wurtman, R. J., Regan, M. M., Taylor, J. A., Shi, J. P., & Leclair, O. U. (2001). Melatonin treatment for age-related insomnia. Journal of Clinical Endocrinology & Metabolism, 86(10), 4727-4730. https://doi.org/10.1210/jcem.86.10.7901
- van Geijlswijk, I. M., Korzilius, H. P., & Smits, M. G. (2010). The use of exogenous melatonin in delayed sleep phase disorder: a meta-analysis. Sleep, 33(12), 1605-1614. https://doi.org/10.1093/sleep/33.12.1605
- Garfinkel, D., Laudon, M., Nof, D., & Zisapel, N. (1995). Improvement of sleep quality in elderly people by controlled-release melatonin. The Lancet, 346(8974), 541-544. https://doi.org/10.1016/S0140-6736(95)91382-3
- Haimov, I., Lavie, P., Laudon, M., Herer, P., Vigder, C., & Zisapel, N. (1995). Melatonin replacement therapy of elderly insomniacs. Sleep, 18(7), 598-603. https://doi.org/10.1093/sleep/18.7.598
- Lemoine, P., Nir, T., Laudon, M., & Zisapel, N. (2007). Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. Journal of Sleep Research, 16(4), 372-380. https://doi.org/10.1111/j.1365-2869.2007.00613.x
- Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J., & Hall, M. H. (2015). The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Medicine Reviews, 22, 23-36. https://doi.org/10.1016/j.smrv.2014.10.001
- Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., … & Adams Hillard, P. J. (2015). National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 1(1), 40-43. https://doi.org/10.1016/j.sleh.2014.12.010
- Zeitzer, J. M., Dijk, D. J., Kronauer, R., Brown, E., & Czeisler, C. (2000). Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. Journal of Physiology, 526(3), 695-702. https://doi.org/10.1111/j.1469- 7793.2000.00695.x
- Chang, A. M., Aeschbach, D., Duffy, J. F., & Czeisler, C. A. (2015). Evening use of light emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences, 112(4), 1232-1237. https://doi.org/10.1073/pnas.1418490112
- Drake, C., Roehrs, T., Shambroom, J., & Roth, T. (2013). Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. Journal of Clinical Sleep Medicine, 9(11), 1195- 1200. https://doi.org/10.5664/jcsm.3170
- Youngstedt, S. D. (2005). Effects of exercise on sleep. Clinics in Sports Medicine, 24(2), 355-365. https://doi.org/10.1016/j.csm.2004.12.003
- Jacobson, B. H., Boolani, A., Dunklee, G., Shepardson, A., & Acharya, H. (2007). Effect of prescribed sleep surfaces on back pain and sleep quality in patients diagnosed with low back and shoulder pain. Applied Ergonomics, 42(1), 91-97. https://doi.org/10.1016/j.apergo.2010.05.004
- Harvey, A. G. (2002). A cognitive model of insomnia. Behaviour Research and Therapy, 40(8), 869-893. https://doi.org/10.1016/S0005-7967(01)00061-4
- Youngstedt, S. D., & Kline, C. E. (2006). Epidemiology of exercise and sleep. Sleep and Biological Rhythms, 4(3), 215-221. https://doi.org/10.1111/j.1479-8425.2006.00235.x
- Härtter, S., Nordmark, A., Rose, D. M., Bertilsson, L., Tybring, G., & Laine, K. (2003). Effects of caffeine intake on the pharmacokinetics of melatonin, a probe drug for CYP1A2 activity. British Journal of Clinical Pharmacology, 56(6), 679-682. https://doi.org/10.1046/j.1365-2125.2003.01933.x
- Landolt, H. P., Werth, E., Borbély, A. A., & Dijk, D. J. (1995). Caffeine intake (200 mg) in the morning affects human sleep and EEG power spectra at night. Brain Research, 675(1- 2), 67-74. https://doi.org/10.1016/0006-8993(95)00040-W
- Ebrahim, I. O., Shapiro, C. M., Williams, A. J., & Fenwick, P. B. (2013). Alcohol and sleep I: effects on normal sleep. Alcoholism: Clinical and Experimental Research, 37(4), 539-549. https://doi.org/10.1111/acer.12006
- Reiter, R. J., Manchester, L. C., & Tan, D. X. (2005). Melatonin in walnuts: influence on levels of melatonin and total antioxidant capacity of blood. Nutrition, 21(9), 920-924. https://doi.org/10.1016/j.nut.2005.02.005
- Bailey, D. G. (2010). Fruit juice inhibition of uptake transport: a new type of food-drug interaction. British Journal of Clinical Pharmacology, 70(5), 645-655. https://doi.org/10.1111/j.1365-2125.2010.03722.x
- Bent, S., Padula, A., Moore, D., Patterson, M., & Mehling, W. (2006). Valerian for sleep: a systematic review and meta-analysis. The American Journal of Medicine, 119(12), 1005- 1012. https://doi.org/10.1016/j.amjmed.2006.02.026
- Whitten, D. L., Myers, S. P., Hawrelak, J. A., & Wohlmuth, H. (2006). The effect of St John’s wort extracts on CYP3A: a systematic review of prospective clinical trials. British Journal of Clinical Pharmacology, 62(5), 512-526. https://doi.org/10.1111/j.1365- 2125.2006.02692.x
- Afaghi, A., O’Connor, H., & Chow, C. M. (2007). High-glycemic-index carbohydrate meals shorten sleep onset. The American Journal of Clinical Nutrition, 85(2), 426-430. https://doi.org/10.1093/ajcn/85.2.426
- National Center for Complementary and Integrative Health. (2019). Sleep disorders and complementary health approaches: what you need to know. NCCIH Publication No. D428.
- Silber, B. Y., & Schmitt, J. A. (2010). Effects of tryptophan loading on human cognition, mood, and sleep. Neuroscience & Biobehavioral Reviews, 34(3), 387-407. https://doi.org/10.1016/j.neubiorev.2009.08.005
- Schutte-Rodin, S., Broch, L., Buysse, D., Dorsey, C., & Sateia, M. (2008). Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine, 4(5), 487-504. https://doi.org/10.5664/jcsm.27286
- Burgess, H. J., Revell, V. L., & Eastman, C. I. (2008). A three pulse phase response curve to three milligrams of melatonin in humans. Journal of Physiology, 586(2), 639-647. https://doi.org/10.1113/jphysiol.2007.143180
- Zhdanova, I. V., Wurtman, R. J., Lynch, H. J., Ives, J. R., Dollins, A. B., Morabito, C., … & Schomer, D. L. (1995). Sleep-inducing effects of low doses of melatonin ingested in the evening. Clinical Pharmacology & Therapeutics, 57(5), 552-558. https://doi.org/10.1016/0009-9236(95)90040-3
- Stepanski, E. J., & Wyatt, J. K. (2003). Use of sleep hygiene in the treatment of insomnia. Sleep Medicine Reviews, 7(3), 215-225. https://doi.org/10.1053/smrv.2001.0246 288.American Academy of Sleep Medicine. (2014). International classification of sleep disorders (3rd ed.). American Academy of Sleep Medicine.
- Ancoli-Israel, S., & Roth, T. (1999). Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. Sleep, 22(Suppl 2), S347-S353.
- Morin, C. M., LeBlanc, M., Daley, M., Gregoire, J. P., & Mérette, C. (2006). Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help seeking behaviors. Sleep Medicine, 7(2), 123-130. https://doi.org/10.1016/j.sleep.2005.08.008
- Wade, A. G., Ford, I., Crawford, G., McMahon, A. D., Nir, T., Laudon, M., & Zisapel, N. (2007). Efficacy of prolonged release melatonin in insomnia patients aged 55-80 years:
- quality of sleep and next-day alertness outcomes. Current Medical Research and Opinion, 23(10), 2597-2605. https://doi.org/10.1185/030079907X233098
- Morin, C. M., Vallières, A., Guay, B., Ivers, H., Savard, J., Mérette, C., … & Baillargeon, L. (2009). Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA, 301(19), 2005-2015. https://doi.org/10.1001/jama.2009.682
How long does it take for melatonin to start working, and how long do the effects last?
The onset of melatonin effects can vary significantly among individuals, but most people begin to experience drowsiness within 30 minutes to 2 hours after taking the medication.[207] The 10 mg dose may produce effects more quickly and intensely than lower doses, though individual sensitivity varies considerably.[208] The duration of melatonin effects typically ranges from 4 to 8 hours, depending on factors such as individual metabolism, age, concurrent medications, and overall health status.[209] Patients with slower metabolism may experience longer-lasting effects, potentially leading to morning grogginess.[210] The timing of administration plays a crucial role in optimizing therapeutic benefits while minimizing next-day sedation.[211] Healthcare providers typically recommend taking melatonin 1 to 3 hours before desired bedtime to allow adequate time for absorption and onset of effects.[212] Some patients may need to experiment with timing under medical supervision to find their optimal administration schedule.[213]
Can I take melatonin every night, or should it only be used occasionally?
The frequency of melatonin use depends on the specific condition being treated and individual patient factors.[214] For chronic sleep disorders such as delayed sleep phase syndrome or persistent insomnia, nightly use may be appropriate under medical supervision.[215] However, for situational sleep difficulties or jet lag, intermittent use is typically more appropriate.[216] Long-term safety data for nightly melatonin use remains limited, particularly for higher doses like 10 mg.[217] Some healthcare providers recommend periodic breaks from melatonin therapy to assess ongoing necessity and prevent potential tolerance development.[218] Patients should work closely with their healthcare providers to determine the most appropriate dosing frequency based on their specific circumstances.[219] Regular follow-up appointments allow for monitoring of treatment effectiveness and assessment of any emerging side effects or concerns.[220] The decision regarding frequency of use should also consider other sleep hygiene measures and non-pharmacological interventions that may reduce the need for medication.[221]
What should I do if I accidentally take too much melatonin?
Melatonin overdose is generally not considered life-threatening, but taking excessive amounts can lead to prolonged sedation and other uncomfortable side effects.[222] If someone accidentally takes significantly more melatonin than prescribed, they should contact their healthcare provider or poison control center for guidance.[223] Symptoms of melatonin overdose may include excessive drowsiness, confusion, headache, nausea, and difficulty waking up the following morning.[224] In cases of significant overdose, medical evaluation may be necessary to monitor for complications and provide supportive care.[225] Patients should be advised to store melatonin capsules securely to prevent accidental ingestion by children or confused individuals.[226] If excessive sedation occurs after taking too much melatonin, patients should avoid driving or operating machinery until effects have completely resolved.[227] Prevention of accidental overdose involves careful attention to dosing instructions and avoiding taking additional doses if the initial dose seems ineffective on a particular night.[228]
Can melatonin interact with my other medications, and what should I watch for?
Melatonin can interact with various medications, and patients should always inform their healthcare providers about all medications and supplements they are taking.[229] The most significant interactions involve medications that affect liver enzymes responsible for melatonin metabolism.[230] Blood-thinning medications like warfarin may have enhanced effects when combined with melatonin, potentially increasing bleeding risk.[231] Medications that cause drowsiness, including prescription sleep aids, anxiety medications, and certain pain medications, may have additive sedating effects with melatonin.[232] Patients taking these combinations should be particularly cautious about activities requiring alertness.[233] Some antidepressants, particularly fluvoxamine, can dramatically increase melatonin levels in the blood.[234] Beta-blockers used for high blood pressure or heart conditions may suppress natural melatonin production, potentially affecting the response to supplemental melatonin.[235] Patients should watch for signs of excessive sedation, morning grogginess, dizziness, or any unusual bleeding or bruising.[236] Any concerning symptoms should be reported to healthcare providers promptly.[237]
Is it safe to drive or operate machinery after taking melatonin?
Driving or operating machinery after taking melatonin can be dangerous due to the medication’s sedating effects.[238] The 10 mg dose is particularly likely to cause significant drowsiness that may impair reaction time, concentration, and motor coordination.[239] Patients should avoid driving for at least 4 to 6 hours after taking melatonin, and longer if they experience persistent drowsiness.[240] The impairment from melatonin may be subtle and not immediately apparent to the user, making it particularly hazardous.[241] Morning-after effects are possible, especially with higher doses, and patients should assess their alertness level before engaging in activities requiring full attention.[242] Individual sensitivity varies significantly, and some patients may experience impairment for longer periods than others.[243] Patients should be especially cautious when first starting melatonin therapy or when doses are adjusted.[244] Alternative transportation arrangements should be made if there is any doubt about alertness or ability to drive safely.[245] Employers should be informed if job duties involve operating machinery or require high levels of attention and coordination.[246]
Can melatonin cause dependence or withdrawal symptoms?
Current evidence suggests that melatonin does not cause physical dependence in the same way as traditional sleep medications.[247] However, some patients may develop psychological dependence or feel unable to sleep without taking melatonin.[248] True withdrawal symptoms are not typically reported when melatonin is discontinued, though some patients may experience return of original sleep difficulties.[249] The rebound insomnia that occurs after stopping melatonin is generally considered a return to baseline sleep problems rather than a withdrawal effect.[250] Some patients may experience temporary sleep disruption when discontinuing long-term melatonin use, particularly if underlying sleep disorders have not been addressed.[251] Gradual tapering rather than abrupt discontinuation may help minimize any sleep disturbances when stopping melatonin.[252] Healthcare providers can help develop appropriate discontinuation strategies based on individual circumstances.[253] Addressing underlying causes of sleep problems through sleep hygiene, stress management, and other interventions may reduce reliance on melatonin supplementation.[254] Patients should not feel concerned about physical addiction potential with melatonin use.[255]
How does melatonin compare to prescription sleep medications?
Melatonin differs significantly from traditional prescription sleep medications in terms of mechanism of action, side effect profile, and dependency potential.[256] Unlike benzodiazepines or Z-drugs that enhance GABA activity, melatonin works through specific melatonin receptors to promote natural sleep processes.[257] This difference in mechanism generally results in fewer side effects and less risk of tolerance or dependence.[258] However, melatonin may be less effective than prescription sleep aids for severe insomnia or acute sleep disturbances.[259] The onset of action for melatonin is typically slower and more variable than prescription sleep medications.[260] Melatonin is particularly effective for circadian rhythm disorders, which may not respond well to traditional sleep aids.[261] The side effect profile of melatonin is generally milder, with fewer reports of morning hangover effects, cognitive impairment, or next-day drowsiness compared to prescription alternatives.[262] However, individual responses vary, and some patients may find prescription medications more effective for their specific sleep problems.[263] The choice between melatonin and prescription sleep aids should be based on careful evaluation of the patient’s specific condition, medical history, and treatment goals.[264]
What lifestyle changes can enhance the effectiveness of melatonin?
Several lifestyle modifications can significantly enhance melatonin’s effectiveness and improve overall sleep quality.[265] Maintaining consistent sleep and wake times helps reinforce natural circadian rhythms and may improve melatonin’s effectiveness.[266] Creating a dark, cool, and quiet sleep environment supports both natural melatonin production and the effects of supplemental melatonin.[267] Limiting exposure to bright lights, particularly blue light from electronic devices, in the evening can help maintain natural melatonin production patterns.[268] Avoiding caffeine, alcohol, and large meals close to bedtime can improve sleep quality and prevent interference with melatonin’s effects.[269] Regular exercise during the day can improve sleep quality and may enhance responsiveness to melatonin, though vigorous exercise should be avoided close to bedtime.[270] Stress management techniques such as meditation, deep breathing, or progressive muscle relaxation can complement melatonin’s sleep-promoting effects.[271] Establishing a consistent bedtime routine signals the body to prepare for sleep and may work synergistically with melatonin supplementation.[272] Limiting daytime naps, particularly late in the day, can help maintain appropriate sleep drive and improve nighttime sleep quality.[273]
Are there any foods or supplements that interact with melatonin?
Certain foods and dietary supplements can potentially interact with melatonin or affect its absorption and effectiveness.[274] Caffeine consumption, particularly in the afternoon or evening, can counteract melatonin’s sleep-promoting effects.[275] Alcohol may initially cause drowsiness but can disrupt sleep quality and interfere with melatonin’s ability to maintain sleep throughout the night.[276] Foods high in natural melatonin, such as tart cherries, may complement supplemental melatonin but could potentially increase overall melatonin exposure.[277] Grapefruit and grapefruit juice can affect the metabolism of many medications, though specific interactions with melatonin are not well-established.[278] Other supplements with sedating properties, such as valerian root, passionflower, or kava, may have additive effects with melatonin.[279] St. John’s wort may potentially affect melatonin metabolism through its effects on liver enzymes.[280] High-protein meals close to bedtime may interfere with melatonin absorption, while foods containing tryptophan may complement its effects.[281] Patients should discuss all dietary supplements and significant dietary habits with their healthcare providers to identify potential interactions.[282] Timing of food intake relative to melatonin administration may affect absorption and should be considered when optimizing treatment effectiveness.[283]
What should I do if melatonin doesn’t seem to be working for me?
If melatonin appears ineffective, several factors should be evaluated before concluding that the treatment is unsuccessful.[284] The timing of administration may need adjustment, as taking melatonin too close to bedtime or too early may reduce effectiveness.[285] Dosage may need modification, though higher doses are not always more effective and may actually worsen sleep in some patients.[286] Lifestyle factors such as light exposure, caffeine intake, stress levels, and sleep environment should be assessed and optimized.[287] Underlying medical conditions, including sleep apnea, restless leg syndrome, or mood disorders, may interfere with melatonin’s effectiveness and require separate treatment.[288] Medication interactions should be reviewed, as certain drugs may reduce melatonin’s effectiveness or counteract its benefits.[289] The duration of treatment may be insufficient, as some patients require several weeks of consistent use before experiencing optimal benefits.[290] Alternative formulations, such as immediate-release versus extended-release preparations, may be more appropriate for specific sleep problems.[291] If melatonin remains ineffective after appropriate optimization, other treatment approaches, including prescription sleep medications, cognitive behavioral therapy for insomnia, or referral to a sleep specialist, may be necessary.[292]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Mirtazapine Tablets
Mirtazapine Tablets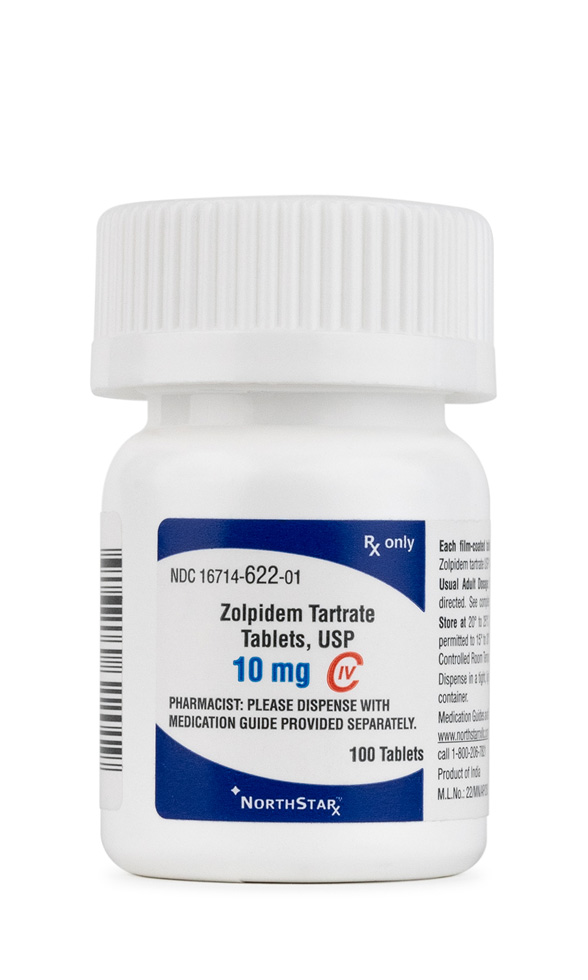 Zolpidem Tartrate Tablets
Zolpidem Tartrate Tablets NAD+ Injection (Lyo)
NAD+ Injection (Lyo) NAD+ Nasal Spray
NAD+ Nasal Spray Oxytocin Nasal Spray
Oxytocin Nasal Spray