Product Overview
Lipo Sculpt Cream is a customized, prescription-only, transdermal formulation intended to support localized adipose reduction in adults pursuing medically supervised body-recomposition strategies. It is compounded exclusively in a 503A pharmacy and supplied as three related 60 mL preparations: (1) Lipo Sculpt Cream containing 0.5 % aminophylline, (2) Lipo Sculpt Max with 0.5 % aminophylline + 5 % 7-keto DHEA, and (3) Lipo Sculpt Lean with 0.5 % aminophylline + 2.5 % 7-keto DHEA + 0.25 % phenylephrine HCl. These strengths reflect concentrations investigated in controlled and observational studies of topical lipolysis and thermogenesis.[1]
Unlike over-the-counter cosmetics, each batch is prepared against a physician order under USP <795> non-sterile compounding standards. No component is FDA-approved for topical fat reduction; prescribers therefore rely on emerging clinical data, pharmacologic plausibility, and professional judgment. Reviews of aminophylline creams show modest but reproducible reductions in thigh or waist circumference when paired with caloric control and exercise, though outcomes are heterogeneous.[2] Commentary in the medical press cautions that expectations must be tempered and therapy individualized.[3]
Because compounded topical agents bypass first-pass hepatic metabolism, systemic exposure can occur even when applied to limited surface area. Clinicians should counsel patients regarding appropriate dosing frequency, occlusion, and the need to discontinue at the first sign of cutaneous intolerance. Regular reevaluation of weight-management goals, lifestyle factors, and metabolic parameters is essential to sustain results and to avoid overreliance on pharmacologic aids.[3]
Unless otherwise directed, a thin layer (≈ 1 mL) is gently massaged into the target area twice daily for up to 12 weeks, not exceeding 2 g aminophylline daily. The 0.5 % strength was selected because studies comparing 0.5 % to higher concentrations found no incremental benefit and a lower risk of irritation.[16] Hands should be washed after application, and occlusive wraps should be avoided unless instructed by the prescriber.
Aminophylline is a theophylline-ethylenediamine complex that acts as a non-selective phosphodiesterase inhibitor, raising intracellular cyclic-AMP. In adipocytes, cAMP activates hormone-sensitive lipase, catalyzing triglyceride hydrolysis and promoting free-fatty-acid release⁴. In addition, aminophylline antagonizes A₂-adenosine receptors, further potentiating catecholamine-stimulated lipolysis.[4]
7-Keto DHEA (3-acetyl-7-oxo-dehydroepiandrosterone) is an endogenous metabolite of DHEA that cannot be converted back to sex hormones. Human and animal data indicate that 7-keto up-regulates thermogenic mitochondrial enzymes such as malic enzyme and glycerol-3-phosphate dehydrogenase, increasing resting metabolic rate without androgenic effects.[5] A systematic review reports variable but generally favorable impacts on body-composition metrics when 7-keto is combined with caloric restriction.[5]
Randomized trials demonstrate that oral or transdermal 7-keto boosts basal metabolic rate by approximately 5-7 % and augments weight loss relative to placebo when combined with diet and exercise⁶. Although exact percutaneous kinetics remain under investigation, in vitro diffusion studies suggest that ethanol-liposomal bases enhance dermal penetration, allowing delivery to subcutaneous fat pads. Synergistically, phenylephrine, an α₁-adrenergic agonist, induces transient vasoconstriction that may reduce dermal edema and concentrate lipolytic mediators at the application site, while its own cAMP-independent pathway augments mobilization of adipose-associated water.[6]
Use is contraindicated in individuals with known hypersensitivity to methylxanthines, ethylenediamine, aminophylline, or any cream excipient. Case reports describe systemic contact dermatitis and “baboon syndrome” following aminophylline exposure, underscoring the need for careful history and patch testing in atopic patients.[7]
Phenylephrine-containing versions are contraindicated in patients receiving monoamine-oxidase inhibitors or in those with uncontrolled hypertension, serious cardiovascular disease, or narrow-angle glaucoma; α-adrenergic stimulation can precipitate hypertensive crises or ocular hypertensive events.[8]
Topical aminophylline can theoretically interact with systemic CYP1A2 inhibitors. Ciprofloxacin markedly elevates serum theophylline concentrations; even low transdermal uptake could add to that burden, warranting monitoring or alternative antibiotics.[9]
Phenylephrine shares class interactions with sympathomimetics; concomitant use with other vasoconstrictors or MAO-inhibiting antidepressants increases pressor responses.[10] To date, no clinically significant drug-drug interactions have been reported with topical 7-keto DHEA, but caution is advised when patients use systemic hormone-replacement therapies given limited data.
Local adverse effects from aminophylline include erythema, pruritus, burning, and rare eczematous eruptions; systemic tremor, insomnia, or tachycardia are unlikely but possible, especially with occlusive dressings.[11]
Short-term clinical trials of 7-keto DHEA reveal a favorable safety profile, with gastrointestinal upset, dizziness, or mild headache occurring at rates similar to placebo.[12]
Phenylephrine may cause transient blanching, stinging, or rebound vasodilation; systemic side effects such as palpitations, anxiety, or elevated blood pressure are uncommon but documented when excessive quantities are applied to compromised skin.[13]
Methylxanthines cross the placenta and have been assigned Pregnancy Category C; although occasional therapeutic use of theophylline is acceptable when benefits outweigh risks, elective exposure for cosmetic fat reduction is discouraged during pregnancy.[14]
Topical vasoconstrictors, including phenylephrine, can undergo systemic absorption sufficient to influence uteroplacental perfusion; ophthalmologic literature emphasizes judicious use and avoiding high-concentration formulas in pregnant patients.[15] In the absence of controlled data, all Lipo Sculpt variants should be avoided in pregnancy and lactation.
Under USP <795>, water-containing topical creams without published stability data receive a conservative beyond-use date (BUD) of 30 days at controlled room temperature (20 - 25 °C).[17]
Pharmacists may adjust BUD based on validated stability studies, container integrity, and preservative efficacy testing, but must document reasoning and ensure labeling complies with state board rules.[18]
Finished product should be stored upright, tightly closed, away from excess heat or direct sunlight; refrigeration is generally unnecessary and may increase viscosity. If color, odor, or texture changes occur, the preparation should be discarded regardless of labeled BUD.[19]
- Pérez, L., & Wu, H. (2023). The efficacy of topical aminophylline in local fat reduction: A systematic review. Frontiers in Endocrinology, 14, 1087614. https://doi.org/10.3389/fendo.2023.1087614
- Smith, M. J. (2007). Topical treatments for fat reduction. Medscape. https://www.medscape.org/viewarticle/563998
- Pfotenhauer, E. (2011, August 8). A cream to fight obesity is being ignored. KevinMD. https://www.kevinmd.com/2011/08/cream-fight-obesity.html
- Pure Encapsulations. (2021). 7-Keto® DHEA: Product information sheet. https://www.pureencapsulationspro.com/media/pdf_upload/PURE_PIS_7Keto_DHEA_final.pdf
- DuPont, J., & Rogalski, K. (2022). A systematic review of the impact of 7-keto-DHEA on body weight. Archives of Gynecology and Obstetrics, 306(6), 1435-1446. https://doi.org/10.1007/s00404-022-06884-8
- Zenk, J. L., et al. (2002). The effect of 7-Keto Naturalean™ on weight loss: A randomized, double-blind, placebo-controlled trial. Current Therapeutic Research, 63(8), 517-525. https://doi.org/10.1016/S0011-393X(02)80031-5
- Isaksson, M., & Ljunggren, B. (2002). Systemic contact dermatitis from ethylenediamine in an aminophylline preparation. Acta Dermato-Venereologica, 82(5), 375-377. https://doi.org/10.1080/000155502320624251
- Medicine.com. (2020). Phenylephrine (topical): Professional drug information. https://www.medicine.com/drug/phenylephrine-topical/hcp
- Drugs.com. (2024). Aminophylline and ciprofloxacin drug interactions. https://www.drugs.com/drug-interactions/aminophylline-with-ciprofloxacin-161-0-672-0.html
- Drugs.com. (2024). Phenylephrine topical interactions. https://www.drugs.com/drug-interactions/phenylephrine-topical.html
- Drugs.com. (2025). Aminophylline: Side effects. https://www.drugs.com/sfx/aminophylline-side-effects.html
- Natural Remedy Insider. (2024). 7-Keto DHEA side effects. https://naturalremedyinsider.com/7-keto-dhea-side-effects/
- Drugs.com. (2024). Phenylephrine topical: Side effects. https://www.drugs.com/sfx/phenylephrine-topical-side-effects.html
- Drugs.com. (2024). Theophylline use during pregnancy. https://www.drugs.com/pregnancy/theophylline.html
- University of Iowa. (2015). Use of ophthalmic medications in pregnancy. https://webeye.ophth.uiowa.edu/eyeforum/cases/229-drugs-in-pregnancy.htm
- Springer, M., & Cohen, A. (2010). Aminophylline 0.5 % cream efficacy in mesotherapy. In Mesotherapy solutions for inducing lipolysis and treating cellulite (pp. 287-296). Springer. https://doi.org/10.1007/978-3-642-20113-4_24
- U.S. Pharmacopeia. (2019). USP compounding standards and beyond-use dates fact sheet. https://www.usp.org/sites/default/files/usp/document/our-work/compounding/usp-bud-factsheet.pdf
- American Society of Health-System Pharmacists. (2021). The pharmacist guide to assigning a beyond-use date. https://www.ashp.org/-/media/assets/pharmacy-practice/resource-centers/compounding/docs/The-Pharmacist-Guide-to-Assigning-a-Beyond-Use-Date-_final.pdf
- U.S. Pharmacopeia. (2022). General chapter <795>: Pharmaceutical compounding-nonsterile preparations. https://ftp.uspbpep.com/v29240/usp29nf24s0_c795.html
- ASHP Publications. (2020). Stability considerations for compounded preparations. https://publications.ashp.org/previewpdf/display/book/9781585286812/ch015.xml?inlineView=true
- University of Illinois Veterinary Teaching Hospital. (2024). Establishing BUDs for topical formulations. https://answers.uillinois.edu/illinois.vetmedvth/page.php?id=130886
- Compounders Lab. (2023). What is water activity? https://compounderslab.com/application/files/5015/6106/5529/White-Paper_What-is-Water-Activity.pdf
- Verywell Health. (2024). 17 natural appetite suppressants for weight loss. https://www.verywellhealth.com/natural-appetite-suppressants-8730447
- Verywell Health. (2023). 10 natural appetite suppressants. https://www.verywellhealth.com/10-natural-appetite-suppressants-7970768
- Fernández, M., & Palomares, A. (2004). Enhancement of topical delivery of drugs via direct penetration by phenylephrine. International Journal of Pharmaceutics, 270(1-2), 241-248. https://doi.org/10.1016/j.ijpharm.2003.11.018
- Fraunfelder, F., & Meyer, S. (1990). Systemic effects of topical phenylephrine. JAMA Ophthalmology, 108(9), 1284-1286. https://doi.org/10.1001/archopht.1990.01070020090038
- WebMD. (2025). 7-Keto DHEA: Uses and dosing. https://www.webmd.com/vitamins/ai/ingredientmono-835/7-keto-dhea
- Hello Pharmacist. (2024). 7-Keto DHEA interaction check: Warfarin. https://hellopharmacist.com/drug-supplement-interactions/drug-herbal/7-keto-dhea-with-warfarin-sodium
- The Pain Source. (2013). Topical compounding creams used in pain management. https://thepainsource.com/topical-compounding-creams-used-in-pain-management/
- Life in the Fast Lane. (2024). Phenylephrine-critical care pharmacology note. https://litfl.com/phenylephrine/
How long can I keep a jar once opened?
The beyond-use date is 30 days at room temperature, unless your pharmacist assigns a shorter period based on specific ingredients.[20]
May I refrigerate the cream for a cooling effect?
Cold storage is not harmful but offers no proven stability advantage beyond the labeled 30 days; room temperature facilitates easier spreading.[21]
Why does water activity matter?
Higher water activity (> 0.60) supports microbial growth; USP <795> uses this parameter to limit BUD for creams and gels.[22]
Can I rely on this alone for weight loss?
No. Sustainable fat reduction still requires calorie control and physical activity; topical agents are adjuncts, not substitutes.[23]
Is 7-keto safer than regular DHEA?
7-keto is not converted to sex steroids and therefore has fewer androgenic or estrogenic concerns, though data remain limited.[24]
Will phenylephrine raise my blood pressure?
Systemic absorption is minimal, but hypertensive spikes have been observed in pharmacokinetic studies with high-dose or compromised skin barriers.[25]
What cardiovascular risks exist?
Case series describe transient hypertension and reflex bradycardia after ocular phenylephrine; similar caution applies to large-area dermal use.[26]
How is the usual 7-keto dose chosen?
Oral studies use 100 mg twice daily; topical equivalents are extrapolated by area under the curve, but individualized titration is prudent.[27]
Does 7-keto interact with warfarin?
Current evidence shows no significant interaction, yet clinicians should monitor INR when supplements are added or discontinued.[28]
Are compounded creams more effective than oral products?
Transdermal delivery bypasses first-pass metabolism and can minimize GI side effects, but efficacy varies and depends on adherence and formulation science.[29]
What makes phenylephrine suitable for a cream base?
Its α₁-agonist activity produces localized vasoconstriction that may temporarily reduce superficial edema and enhance cosmetic appearance.[30]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Administration Instructions
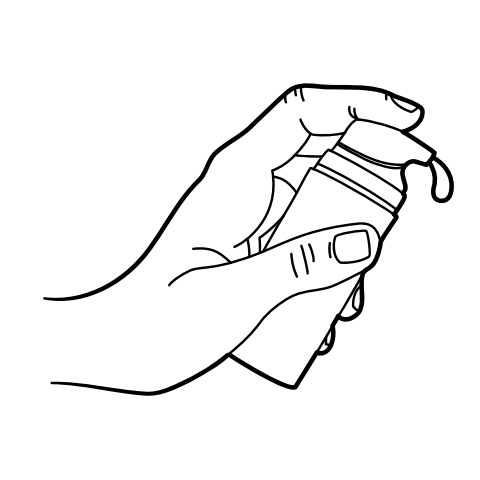
Pump Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.




 Lipo Injection
Lipo Injection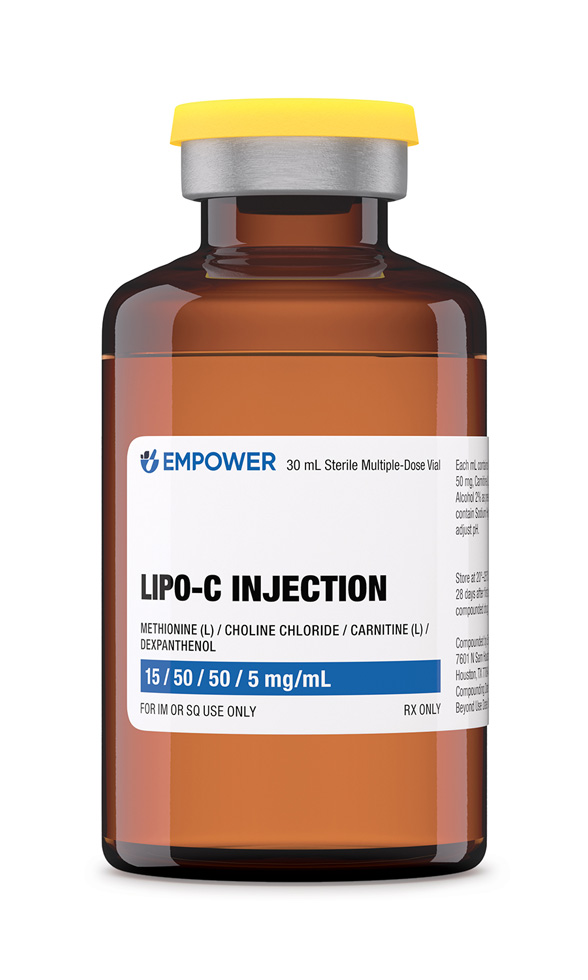 Lipo-C Injection
Lipo-C Injection Lipo Burn Capsules
Lipo Burn Capsules Cyanocobalamin (Vitamin B12) Injection
Cyanocobalamin (Vitamin B12) Injection Tirzepatide / Niacinamide Injection
Tirzepatide / Niacinamide Injection Testosterone Cypionate Injection
Testosterone Cypionate Injection