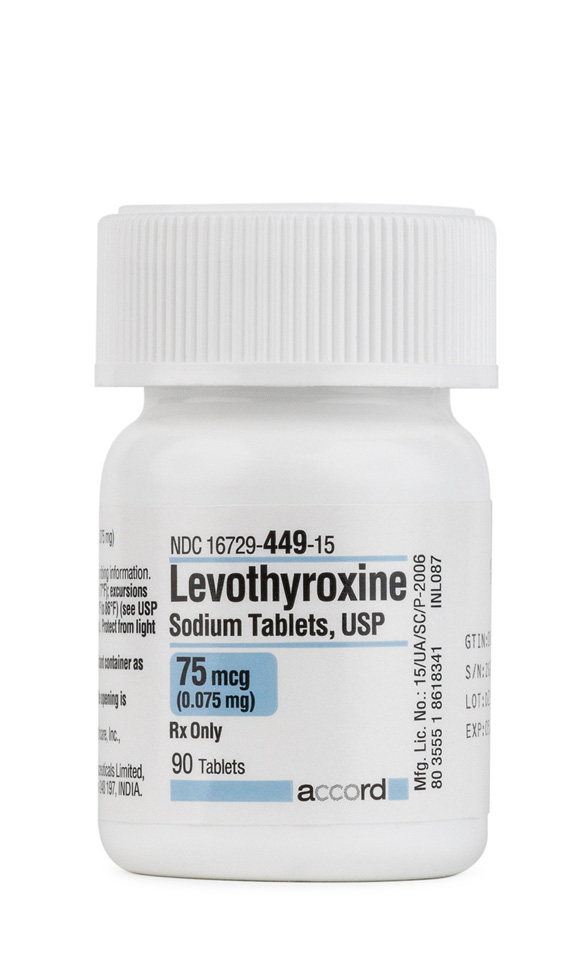
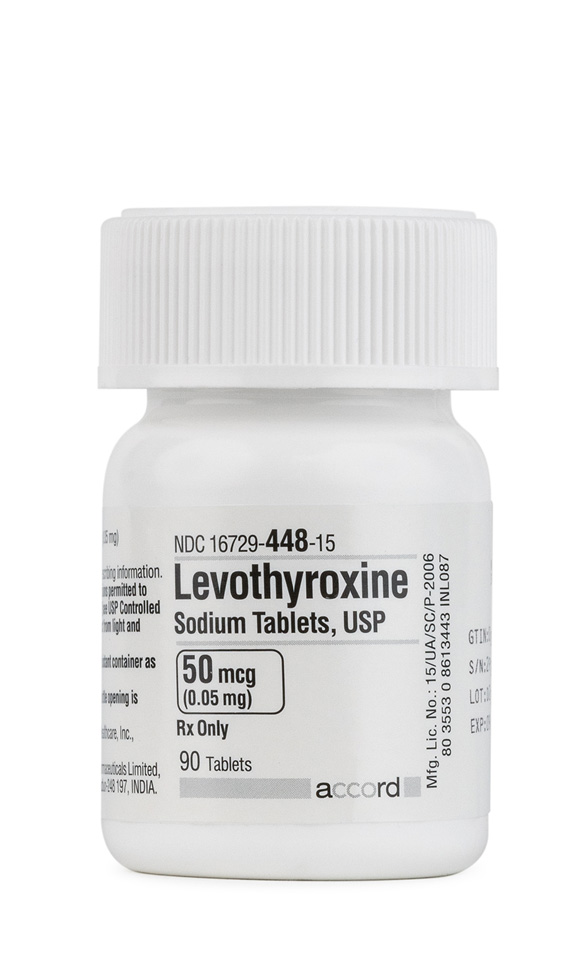
Product Overview
† commercial product
Levothyroxine (T4) is a synthetically prepared levo-isomer of thyroxine, a hormone secreted by the thyroid gland. Levothyroxine is used in the treatment of primary, secondary (pituitary), and tertiary (hypothalamic) hypothyroidism. Levothyroxine will potently suppress thyrotropin secretion in the management of goiter and chronic lymphocytic thyroiditis, and it can be used in combination with antithyroid agents to prevent the abc development of hypothyroidism or goitrogenesis during the treatment of thyrotoxicosis. Intravenous levothyroxine is primarily used to treat myxedema coma or stupor. Levothyroxine therapy is preferred over thyroid and thyroglobulin because the hormonal content of levothyroxine is standardized, and the effects of the drug are more predictable. Levothyroxine provides only T4, of which roughly 80% is deiodinated to T3 and reverse T3. Since T3 is three times as potent as T4, virtually all of the activity of T4 can be ascribed to T3. Levothyroxine has been used clinically since the 1950s. Thyroid drugs containing levothyroxine sodium were sold for years without FDA approval. For many years, there has been controversy regarding the bioequivalence of different oral levothyroxine products, which had not been reviewed by modern FDA approval processes.[1] A controversial study published in Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.7 showed that several products were bioequivalent.[2] Subsequently, in August Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.7, the FDA announced that NDAs would be required for all oral levothyroxine products by August 2003. The required NDA will ensure that FDA standards for purity, potency, stability, safety and efficacy are met. Unithroid® and Levoxyl® received an FDA approval via the new NDA requirements in August 2000 and May 2001, respectively. Levo-T® received formal FDA-approval in early 2002; followed by the FDA-approval of Synthroid®, after 47 years of marketing, in July 2002. Levolet® products were FDA-approved in 2003; Levothroid® products were FDA-approved in 2004. Tirosint™ capsules were FDA-approved in October of 2006. The NDA status of other marketed brands is not clear.
Levothyroxine exhibits all the actions of endogenous thyroid hormone. Liothyronine (T3) is the principal hormone that exhibits these actions whereas levothyroxine (T4) is the major hormone secreted by the thyroid gland and is metabolically deiodinated to T3 in peripheral tissues. Serum concentrations of T4 and TSH are typically used as the primary monitoring parameters for determining thyroid function.
In general, thyroid hormones influence the growth and maturation of tissues, increase energy expenditure, and affect the turnover of essentially all substrates. These effects are mediated through control of DNA transcription and, ultimately, protein synthesis. Thyroid hormones play an integral role in both anabolic and catabolic processes and are particularly important to the development of the central nervous system in newborns. They regulate cell differentiation and proliferation, and aid in the myelination of nerves and the development of axonal and dendritic processes in the nervous system. Thyroid hormones, along with somatotropin, are responsible for regulating growth, particularly of bones and teeth. Thyroid hormones also decrease cholesterol concentrations in the liver and the bloodstream, and have a direct cardiostimulatory action. Cardiac consumption is increased by the administration of thyroid hormone, resulting in an increased cardiac output. Administration of exogenous thyroid hormone to patients with hypothyroidism increases the metabolic rate by enhancing protein and carbohydrate metabolism, increasing gluconeogenesis, facilitating the mobilization of glycogen stores, and increasing protein synthesis. In response to reestablishing physiologic levels of thyroid hormone, thyroid-stimulating hormone (TSH) concentrations correct if the primary disorder is at the level of the thyroid.
The release of T3 and T4 from the thyroid gland into the systemic circulation is regulated by TSH (thyrotropin), which is secreted by the anterior pituitary gland. Thyrotropin release is controlled by the secretion of thyroid-releasing hormone (TRH) from the hypothalamus and by a feedback mechanism dependent on the concentrations of circulating thyroid hormones. When circulating T3 and T4 levels increase, TRH and TSH decrease. Because of this feedback mechanism, the administration of pharmacologic doses of exogenous thyroid hormone to patients with a normal thyroid suppresses endogenous thyroid hormone secretion.
Your health care provider needs to know if you have any of these conditions: angina; blood clotting problems; diabetes; dieting or on a weight loss program; fertility problems; heart disease; high levels of thyroid hormone; pituitary gland problem; previous heart attack; an unusual or allergic reaction to levothyroxine, thyroid hormones, other medicines, foods, dyes, or preservatives; pregnant or trying to get pregnant; breast-feeding.
Levothyroxine capsules (Tirosint) are contraindicated for use in anyone unable to swallow a capsule, generally including young children < 6 years of age. Do not cut or crush the capsules.[9]
Levothyroxine tablets are contraindicated for use in patients with untreated subclinical or overt thyrotoxicosis of any etiology; parenteral levothyroxine and levothyroxine capsules should also not be used in patients with these conditions. Use caution when administering levothyroxine to patients with autonomous thyroid tissue to prevent precipitation of thyrotoxicosis. In addition, administer levothyroxine with caution to patients with nontoxic diffuse goiter or nodular thyroid disease in order to prevent precipitation of thyrotoxicosis; this is especially important in patients with these conditions that also are older or have heart disease. For any of these patients, if the serum TSH is already suppressed, levothyroxine should not be administered.[10]
Administration of oral levothyroxine to patients with uncontrolled adrenal insufficiency can cause adrenal crisis and thus administration is contraindicated. Although not specifically contraindicated, parenteral levothyroxine should also not be used in patients with this condition. Adrenal insufficiency should be corrected with replacement glucocorticoids prior to initiation of treatment. Failure to correct the insufficiency may precipitate an acute adrenal crisis when levothyroxine is initiated. Symptoms of adrenal insufficiency can be unmasked or exacerbated by the administration of thyroid hormones.[10]
Other causes of hypothyroidism (e.g., morphologic hypogonadism and nephroses) should be ruled out prior to beginning treatment with levothyroxine. Patients with hypothyroidism secondary to hypopituitarism are likely to have suppressed adrenal function as well, which should be corrected prior to initiating thyroid replacement therapy. Symptoms of hypopituitarism can be unmasked or exacerbated by the administration of thyroid hormones.[10]
Oral levothyroxine is contraindicated in patients with an acute myocardial infarction. All levothyroxine dosage formulations are cardiostimulatory and should be used with great caution in patients with angina pectoris or other preexisting cardiac disease, including uncontrolled hypertension, cardiac arrhythmias, coronary artery disease, or a previous myocardial infarction; do not use levothyroxine therapy in patients with heart disease and nontoxic diffuse goiter or nodular thyroid disease if the serum TSH concentration is suppressed. Many authorities recommend lower initial dosages and slower titration of thyroid hormones in patients with heart disease. If adverse cardiac symptoms develop or worsen, reduce or withhold levothyroxine and cautiously restart at a lower dose. Over-treatment with thyroid hormones may cause cardiac stimulation and lead to increased heart rate, cardiac wall thickening and increased cardiac contractility, which may precipitate angina or cardiac arrhythmias. Concomitant administration of levothyroxine with sympathomimetic agents in patients with coronary artery disease may precipitate coronary insufficiency and associated symptoms. Patients with coronary artery disease who are receiving thyroid hormones may be at a higher risk for developing arrhythmias, particularly during surgery.[10]
Caution should be used in geriatric patients since they may be more sensitive to the cardiac effects of thyroid replacement. In elderly patients with nontoxic diffuse goiter or nodular thyroid disease, levothyroxine should not be used if the serum TSH concentration is already suppressed. In general, lower initial dosages and slower titration are recommended in elderly patients. Overall, thyroid hormone requirements in the elderly are typically 25% lower than in younger adults. Individualization of dosing is recommended.
Symptoms of diabetes mellitus can be unmasked or exacerbated by the administration of thyroid agents. The use of levothyroxine may require alteration in the dosage of antidiabetic regimens. Blood glucose should be monitored closely during concomitant therapy. In addition, withdrawal of thyroid hormones may cause hypoglycemia in susceptible patients.
Thyroid agents should not be used for obesity treatment or for the purpose of weight loss. Normal doses of levothyroxine are not effective in reducing weight in euthyroid patients. Larger doses may produce serious or even life-threatening toxicity, particularly when given in association with sympathetic amines that are used for their anorectic effects.
Levothyroxine use is only justified for treatment of female or male infertility if such infertility is accompanied by hypothyroidism.
Long-term use of levothyroxine has been associated with decreased bone mineral density, particularly in postmenopausal females on greater than replacement doses or in women receiving suppressive doses. Patients should be given the minimum dose necessary for desired clinical and biochemical response to limit risks for osteoporosis.[10]
Levothyroxine is classified in FDA pregnancy risk category A.[11] Thyroid hormones undergo minimal placental transfer and human experience does not indicate adverse fetal effects; do not discontinue needed replacement during pregnancy. Also, hypothyroidism diagnosed during pregnancy should be promptly treated. Measure TSH during each trimester to gauge adequacy of thyroid replacement dosage since during pregnancy thyroid requirements may increase. Immediately after obstetric delivery, dosage should return to the pre-pregnancy dose, monitor a serum TSH 6-8 weeks postpartum to assess for needed adjustments.
Thyroid hormones, like levothyroxine, are generally compatible with breast-feeding; minimal amounts of thyroid hormones are excreted in breast milk. The American Academy of Pediatrics considers the use of levothyroxine to be usually compatible with breast-feeding due to a lack of reported adverse effects in nursing infants.[12] It should be noted that in general, adequate thyroid replacement doses are needed to maintain normal lactation; levothyroxine is often the drug of choice to treat hypothyroidism during pregnancy and lactation. Comparisons of the levels of TSH and other thyroid function tests between breast-fed and bottle-fed infants have been published.[13][14][15] Breast milk does not provide sufficient levothyroxine (T4) or liothyronine (T3) to prevent the effects of congenital hypothyroidism; therefore serum levels of TSH in breast-fed hypothyroid infants are markedly elevated.[13][14] Euthyroid babies who were breast-fed did not have differences in TSH levels when compared to euthyroid babies receiving formula feedings.[15][16]
Use caution when administering the Levoxyl brand of levothyroxine tablets to patients with dysphasia or other conditions that compromise the ability to swallow. Choking, gagging, tablets getting stuck in the throat, and dysphagia have been reported, mainly when the intact tablets were not taken with water. Counsel patients to take the tablet with water.[17]
This list may not include all possible contraindications.
Possible interactions include: amiodarone; antacids; anti-thyroid medicines;calcium supplements; carbamazepine; cholestyramine; colestipol; digoxin; female hormones, including contraceptive or birth control pills; iron supplements; ketamine; liquid nutrition products like Ensure; medicines for colds and breathing difficulties; medicines for diabetes; medicines for mental depression; medicines or herbals used to decrease weight or appetite; phenobarbital or other barbiturate medications; phenytoin; prednisone or other corticosteroids; rifabutin; rifampin; soy isoflavones;sucralfate; theophylline; warfarin.
NOTE: Many drugs affect thyroid hormone pharmacokinetics, metabolism, or in vivo pharmacodynamics; such drugs may alter the therapeutic response to thyroid hormone replacement. The following medication list is not complete, consult specialized resources for drug-thyroidal axis interactions that may occur.
Antithyroid agents should generally not be administered with the thyroid hormones due to their opposing effects. However, in selected cases some clinicians coadminister T4 (e.g., levothyroxine) to circumvent drug-induced hypothyroidism when large suppressive doses of antithyroid agents are administered for long periods of time. However, clinical and biochemical euthyroid status may usually be maintained with careful titration of the antithyroid agent dosage alone.[11] In addition, iodide and drugs that contain pharmacological amounts of iodine including radiopaque contrast agents that contain iodine (e.g., iohexol, ioversol, iopamidol, and iodixanol) may cause either hypothyroidism or hyperthyroidism in previously euthyroid patients. Patients receiving levothyroxine and drugs that contain iodine should be monitored for changes in thyroid function.[11]
Certain foods, beverages, and enteral feedings can inhibit the absorption of thyroid hormones.[6][11][18] To minimize the risk of an interaction, thyroid hormones should be administered on an empty stomach with a glass of water at least 30-60 minutes prior to food or enteral feedings. Foods that may decrease thyroid hormone absorption include soybean flour and soy-based infant formulas or enteral feedings, as well as high fiber diets, cottonseed meal, and walnuts. In addition to decreasing the oral absorption of thyroid hormones, limited data indicate that soy containing foods and supplements may also influence thyroid physiology. Concentrated soy isoflavones (e.g., genistein and daidzein) may interfere with thyroid peroxidase catalyzed iodination of thyroglobulin, resulting in a decreased production of thyroid hormones and an increased secretion of TSH endogenously.[19] More studies are required to assess the exact mechanism of this interaction. Caution should be used in administering soy isoflavone supplements concurrently with thyroid hormones.[11] Limited data show that coffee has the potential to impair T4 intestinal absorption. In one report, T4 intestinal absorption was evaluated after the administration of 200 mcg L-thyroxine (L-T4) swallowed with coffee/espresso, water, or water followed 60 minutes later by coffee/espresso. Researchers found that administration with coffee/espresso significantly lowered average serum T4 (p<0.001) and peak serum T4 concentrations (p<0.05) when compared to L-T4 taken with water alone. Coffee/espresso taken 60 minutes after L-T4 ingestion had no significant effect on T4 intestinal absorption. It is prudent to remind patients that thyroid hormones should be separated from food and beverages (other than water), including coffee, by at least 30-60 minutes.[18] The bile-acid sequestrants cholestyramine and colestipol are well-known to cause drug interactions by binding and decreasing the oral administration of many drugs.[20][21] Cholestyramine and colestipol have been shown to decrease the absorption of levothyroxine. To minimize this interaction, administer levothyroxine at least 4 hours before or after cholestyramine or colestipol.[11] Oral aluminum hydroxide, magnesium salts, calcium salts, calcium carbonate, and antacids, containing any of these electrolyte salts have been reported to chelate oral levothyroxine within the GI tract when administered simultaneously, leading to decreased thyroid hormone absorption. Some case reports have described clinical hypothyroidism resulting from coadministration of levothyroxine with oral calcium supplements and aluminum hydroxide. To minimize this interaction, administer levothyroxine at least 4 hours before or after antacids or other drugs containing aluminum, magnesium, or calcium.[11][22][23] Polysaccharide-iron complex and other oral iron salts have been reported to chelate oral thyroid hormones within the GI tract when administered simultaneously, leading to decreased thyroid hormone absorption. Some case reports have described clinical hypothyroidism resulting from coadministration of thyroid hormones with oral iron supplements.[24] To minimize the risk of interaction, oral thyroid hormones should be administered at least 4 hours before or after the ingestion of iron supplements.[11] Sucralfate has been reported to chelate oral thyroid hormones within the GI tract when administered simultaneously, leading to decreased thyroid hormone absorption. To minimize the risk of interaction, oral thyroid hormones should be administered at least 4 hours before or after the ingestion of sucralfate.[11] Simethicone has been reported to chelate oral levothyroxine within the GI tract when administered simultaneously, leading to decreased thyroid hormone absorption. To minimize the risk of interaction, oral thyroid hormones should be administered at least 4 hours before or after the ingestion of simethicone.[11] Cation exchange resins like sodium polystyrene sulfonate (i.e., Kayexalate®) can bind levothyroxine in the GI tract and inhibit T4 absorption.[11] Administer thyroid hormones at least 4 hours apart from any of these agents. Sympathomimetic amines should be used with caution in patients with thyrotoxicosis since these patients are unusually responsive to sympathomimetic amines. Based on the cardiovascular stimulatory effects of sympathomimetic drugs, the concomitant use of sympathomimetics and thyroid hormones can enhance the effects on the cardiovascular system.[11][25] Patients with coronary artery disease have an increased risk of coronary insufficiency from either agent. Concomitant use of these agents may increase this risk further. In addition, dopamine at a dose of >= 1 mcg/kg/min and dopamine agonists (e.g., apomorphine, bromocriptine, levodopa, pergolide, pramipexole, ropinirole, rotigotine) may result in a transient reduction in TSH secretion. The reduction in TSH secretion is not sustained; hypothyroidism does not occur.[11]
Drugs that possess hepatic enzyme-inducing properties, such as barbiturates, carbamazepine, hydantoins (i.e., fosphenytoin, phenytoin, or ethotoin), rifabutin, rifampin, can increase the catabolism of levothyroxine and other thyroid hormones.[11][26][27][28] Clinicians should be alert for a decreased response to thyroid hormones if any of these agents are used during thyroid hormone therapy.
Addition of levothyroxine to antidiabetic or insulin therapy may result in increased dosage requirements of the antidiabetic agents.[11] Thyroid hormones can affect the diabetic state. This represents a pharmacodynamic interaction and not necessarily a pharmacokinetic one, and blood sugars should be carefully monitored when thyroid therapy is added, dosages are changed, or if thyroid hormones are discontinued.
Ketamine should be administered cautiously to patients receiving levothyroxine because concomitant use can cause marked hypertension and tachycardia.[11]
The administration of estrogens and oral contraceptives can increase circulating concentrations of thyroxine-binding globulin. Increased amounts of thyroxine-binding globulin may result in a reduced clinical response to levothyroxine.[11] Some hypothyroid patients on estrogen may require larger doses of levothyroxine.
The effects of indandione- or coumarin-derivative anticoagulants can be altered when thyroid agents are administered concomitantly. It has been shown that by accelerating the metabolic degradation of vitamin K-dependent clotting factors, hyperthyroidism augments the response to warfarin.[29] It is possible that exogenously administered thyroid hormone also can augment the response to oral anticoagulants, such as warfarin or dicumarol.[11] INRs should be monitored carefully in patients receiving warfarin and levothyroxine concomitantly and the dose of the anticoagulant should be adjusted as needed.
The metabolism of corticosteroids and corticotropin (ACTH) are increased in patients with hyperthyroidism and decreased in patients with hypothyroidism. Additionally, short-term administration of large corticosteroid doses (i.e., dexamethasone) may decrease serum T3 concentrations by 30%, and long-term corticosteroid therapy may result in decreased thyroid binding globulin production, causing slightly decreased T3 and T4 concentrations.[11] Therefore, caution should be taken when initiating, changing or discontinuing thyroid agents.
Amiodarone has a complex effect on the metabolism of thyroid hormones and can alter thyroid function tests in many patients. Since approximately 37% of amiodarone (by weight) is iodine, maintenance doses of 200-600 mg of amiodarone/day result in ingestion of 75-225 mg/day of organic iodide, resulting in much higher total iodine stores in the body. In addition, amiodarone decreases T4 5′-deiodinase activity, which decreases the peripheral conversion of T4 to T3, leading to decreased serum T3. Serum T4 levels are usually normal but may be slightly increased. TSH concentrations usually increase during amiodarone therapy, but after 3 months of continuous administration, TSH concentrations often return to normal. However, amiodarone can cause hypothyroidism or hyperthyroidism, including life-threatening thyrotoxicosis. Therefore, patients receiving levothyroxine and amiodarone should be monitored for changes in thyroid function; because of the slow elimination of amiodarone and its metabolites, abnormal thyroid function tests may persists for weeks or months after amiodarone drug discontinuation.[11][30]
Decreased digoxin clearance occurs with hypothyroidism; when corrected with thyroid hormone, clearance returns to normal. Hypothyroid patients may have an increased risk for digitalis toxicity. When thyroid hormone therapy is added, however, an increase in the digoxin dose may be necessary.[11]
Thyroid hormones may increase receptor sensitivity and enhance the effects of tricyclic antidepressants and related drugs (e.g., amoxapine, maprotiline).[11][31][32] Older literature describes a variety of responses when tricyclic antidepressants are used concomitantly with thyroid hormones. The combinations appear to increase receptor sensitivity to catecholamines.[11] Thyroid hormones may accelerate the onset of action of tricyclic antidepressants; however, several case reports have described cardiovascular toxicity as a result of this drug combination; other reports describe no interaction. Although this drug combination appears to be safe, clinicians should be aware of the remote possibility of exaggerated cardiovascular side effects such as arrhythmias and CNS stimulation.
The addition of sertraline to patients stabilized on levothyroxine has resulted in increased levothyroxine requirements. Patients should be monitored for changes in thyroid function if sertraline is added or deleted.[11]
Correction of hypothyroidism to the euthyroid state may precipitate certain drug interactions. For example, hypothyroidism causes decreased clearance of theophylline, which returns to normal in the euthyroid state. Theophylline dosage adjustments may be needed with thyroid hormone replacement.[11]
Because thyroid hormones cause cardiac stimulation including increased heart rate and increased contractility, the effects of beta-blockers may be reduced by thyroid hormones.[11] The reduction of effects may be especially evident when a patient goes from a hypothyroid to a euthyroid state or when excessive amounts of thyroid hormone are given to the patient. In addition, because liothyronine (T3) has more pronounced cardiovascular side effects when compared to levothyroxine (T4), the effects on beta-blockers may be more common in patients treated with liothyronine.[33]
Thyroid hormones are susceptible to drug interactions with buffers/antacids containing aluminum or calcium, which may chelate thyroid hormones within the GI tract and decrease oral thyroid hormone absorption.[11] Certain didanosine, ddI formulations contain buffers (e.g., chewable/dispersible tablets and oral powder for solution) or are mixed with antacids (e.g., pediatric oral powder for solution).[34] Thyroid hormones should be administered at least 4 hours before or after the administration of these didanosine formulations to minimize an interaction. The delayed-release didanosine capsules (e.g., Videx® EC) do not contain a buffering agent and are not expected to interact with thyroid hormones.
Closely monitor the thyroid status of any patient taking thyroid hormones concurrently with indinavir. Hyperthyroidism was reported in a patient when indinavir was added to a stable levothyroxine dosing regimen. Indinavir inhibits UDP-glucuronosyl transferase, which may have decreased the metabolism of the thyroid hormone and may explain the increased thyroxine levels observed.[35] Patients receiving levothyroxine should be carefully monitored when indinavir is started; if hyperthyroidism is detected, reducing the levothyroxine dose should reestablish a euthyroid state. Theoretically, similar interactions may occur between indinavir and other thyroid hormones, given that both T4 and T3 are metabolized to some degree via hepatic UDP-glucuronosyl transferase.
Raloxifene may delay and reduce the oral absorption of levothyroxine (T4). In a case report, a patient with chronic but treated hypothyroidism was taking a stable dose of levothyroxine. The patient required increasing doses of levothyroxine when raloxifene was coadministered; the TSH level remained elevated and serum T4 remained decreased despite an increase in oral levothyroxine dosage. An absorption interaction was suspected and the patient rechallenged on two occasions; a decrease in serum T4 was observed whenever raloxifene and levothyroxine were administered concurrently. The patient’s levothyroxine dosage requirements returned to baseline and the TSH value normalized when levothyroxine and raloxifene were administered 12 hours apart rather than simultaneously. The mechanism for the observed interaction is unknown. In theory, raloxifene might cause malabsorption of any thyroid hormone containing T4 (e.g., desiccated thyroid, levothyroxine, liotrix) if administered at the same time. Patients prescribed raloxifene while taking these thyroid hormones should be advised to take the drugs at separate times (e.g., 12 hours apart) until more data are available.[36]
Long-term aminoglutethimide therapy may decrease serum T4 and T3 concentrations and increase TSH secretion, although concentrations remain within normal limits in most patients. Patients receiving aminoglutethimide and levothyroxine should be monitored for changes in thyroid function.[11]
The concomitant use of systemic tretinoin, ATRA and thyroid hormones should be done cautiously due to the potential for increased intracranial pressure and an increased risk of pseudotumor cerebri (benign intracranial hypertension).[37] Early signs and symptoms of pseudotumor cerebri include papilledema, headache, nausea, vomiting, and visual disturbances.[38][39]
In order to increase thyroid uptake and optimize exposure of thyroid tissue to the radionucleotide sodium iodide I-131, patients must discontinue all medications and supplements that may interfere with iodide uptake into thyroid tissue prior to therapy with sodium iodide I-131. Although various protocols are used, a procedure guideline published by the Society of Nuclear Medicine in February 2002 recommends that all T4 thyroid hormones, such as levothyroxine, be discontinued 4-6 weeks and that all T3 thyroid hormones, such as liothyronine, be discontinued 2 weeks prior to sodium iodide I-131 therapy.[40]
Serum trough cyclosporine concentrations appear to be reduced by concurrent oral cyclosporine and levothyroxine use. Among 10 patients who took Neoral® capsules twice daily for at least a year and oral levothyroxine 100 mcg daily for at least 3 months, the trough serum cyclosporine concentration was significantly lower as compared with values from 30 patients who only took cyclosporine. The mechanism of the interaction may be decreased oral cyclosporine absorption due to P-glycoprotein induction by levothyroxine.[41] Cyclosporine is a substrate of P-glycoprotein, and levothyroxine appears to be an inducer of P-glycoprotein.[28][42] In patients who take oral cyclosporine, carefully monitor cyclosporine concentrations with levothyroxine initiation or discontinuation.
The manufacturer for colesevelam suggests monitoring serum drug concentrations and/or clinical effects for those drugs for which alterations in serum blood concentrations have a clinically significant effect on safety or efficacy.[43] To minimize potential for interactions, consider administering oral drugs with a narrow therapeutic index, such as levothyroxine, at least hours before colesevelam. There have been rare reports of elevated thyroid stimulating hormone (TSH) concentrations in patients who have received colesevelam coadministered with thyroid hormone replacement therapy.[43]
Lithium therapy can result in goiter in up to 50% of patients, and subclinical or overt hypothyroidism in up to 20% of patients. Lithium decreases thyroid hormone synthesis and secretion leading to hypothyroidism after long-term use. Prevalence of hypothyroidism appears to be highest in women and in those patients over the age of 50, with a family history of hypothyroidism.[44] Patients receiving levothyroxine should be monitored for changes in thyroid function when lithium is either initiated or discontinued.[11]
Octreotide, at doses of > 100 mcg/day, may result in a transient reduction in TSH secretion. The reduction in TSH secretion is not sustained; hypothyroidism does not occur.[11]
Excessive use of thyroid hormones with growth hormone (somatropin, rh-GH) may accelerate epiphyseal closure. However, untreated hypothyroidism may interfere with growth response to somatropin. Patients receiving concomitant therapy should be monitored closely to ensure appropriate therapeutic response to somatropin.[11]
Patients treated with orlistat and levothyroxine should be monitored for changes in thyroid function; orlistat may interfere with the absorption of levothyroxine from the gastrointestinal tract.[45][46] A recommendation regarding the separation of levothyroxine and orlistat administration by at least 4 hours has not been made, but may be prudent.
Sevelamer could potentially decrease the oral absorption of other medications; the alteration can be clinically significant for drugs with a narrow therapeutic window such as the thyroid hormones.[47] In one study of normal volunteers, the subjects (n=7) ingested orally levothyroxine sodium, either taken separately or co-administered with sevelamer. Serum thyroxine was measured at intervals over a 6-hour period following drug ingestion. Sevelamer significantly (p <0.05) decreased the area under the serum thyroxine concentration curve. The authors concluded that patients should be advised to separate the time of ingestion of sevelamer from their thyroid hormone preparation.[48]
Administering levothyroxine 4 hours before or after sevelamer may minimize the potential for an interaction.[47] Chromium could potentially decrease the oral absorption of thyroid hormones. In one study of normal volunteers, the subjects (n=7) ingested orally levothyroxine sodium, either taken separately or co-administered with chromium picolinate. Serum thyroxine was measured at intervals over a 6-hour period following drug ingestion. Chromium picolinate significantly (p <0.05) decreased the area under the serum thyroxine concentration curve. The authors concluded that patients should be advised to separate the time of ingestion of chromium from their thyroid hormone preparation.[48] Administering levothyroxine 1 hours before or 3 hours after chromium picolinate ingestion, for example, should minimize the potential for an interaction.
This list may not include all possible drug interactions. Give your health care provider a list of all the medicines, herbs, non-prescription drugs, or dietary supplements you use. Also tell them if you smoke, drink alcohol, or use illegal drugs. Some items may interact with your medicine.
Some possible side effects include: changes in appetite; changes in menstrual periods; diarrhea; hair loss; headache; trouble sleeping; weight loss. This list may not describe all possible side effects. Call your doctor for medical advice about side effects.
Clinicians should monitor for signs and symptoms of hypothyroidism that could require an upward adjustment of the thyroid hormone (e.g., levothyroxine) dosage. Signs or symptoms of underdosage or hypothyroidism include: constipation, cold intolerance, dry skin (xerosis) or hair, fatigue, impaired intellectual performance or other mental status changes (e.g., depression), deepening of voice, lethargy, weight gain, tongue enlargement, and, eventually, myxedema coma.
Adverse reactions to levothyroxine are rare. Adverse reactions usually indicate inappropriate dosage of the hormone. Rare instances of allergic skin reactions such as urticaria (hives) or rash have been reported with the use of levothyroxine tablets; however, these reactions are thought to be due to inactive ingredients. Hypersensitivity to levothyroxine itself is not known to occur.[17]
In normal replacement dosages; adverse reactions to levothyroxine replacement are few; most patients tolerate therapy well and find symptomatic complaints due to hypothyroidism resolve with return to euthymia. Symptoms of adverse reactions may indicate over-replacement of hormone. Many of the signs and symptoms of excess thyroid hormone are subtle and insidious. Manifestations of excessive dosage or hyperthyroidism include anorexia, diaphoresis, diarrhea, dyspnea, elevated hepatic enzymes, emotional lability, fatigue, fever, flushing, headache, heat intolerance, hyperactivity, increased appetite, infertility, irritability, insomnia, menstrual irregularity (e.g., amenorrhea), muscle weakness, muscle cramps, nausea, vomiting, nervousness or anxiety, tremor, and weight loss. The clinician should be alert to constellations of symptoms that gradually worsen over time.[9][11][17][49]
Adverse reactions associated with levothyroxine such as alopecia are primarily those of hyperthyroidism due to therapeutic overdosage.[9][11][17]
Pseudotumor cerebri has been reported in pediatric patients receiving thyroid hormone replacement therapy; the exact incidence and causal relationship to levothyroxine therapy is unknown. Slipped capital femoral epiphysis has also been reported in children receiving levothyroxine. Over-treatment may result in craniosynostosis in infants and premature closure of the epiphyses in children with resultant compromised adult height (growth inhibition).[9][11][17]
Seizures have been reported rarely with the institution of levothyroxine therapy.[9][11][17][49]
Excess levothyroxine therapy, as well as overt hyperthyroidism, can indirectly increase the workload on the heart leading to cardiovascular adverse effects. Hypertension may be a manifestation of excess thyroid hormone. In elderly patients and/or patients with underlying cardiac disease, excess thyroid hormone can produce symptoms including angina, heart failure, palpitations, peripheral edema, and sinus tachycardia. Patients with subclinical hyperthyroidism, either from excessive thyroid hormone replacement or other, may also be at an increased risk for atrial fibrillation. One study compared elderly patients (mean age 65 years) with subclinical hyperthyroidism to euthyroid subjects for 2 years; atrial fibrillation was initially recorded in 8 patients and 3 additional patients developed atrial fibrillation during follow-up; the data correspond to a total incidence of atrial fibrillation of 28% in subclinical hyperthyroidism patients compared to 10% in euthyroid subjects.[50] Some elderly patients may only exhibit cardiovascular signs and symptoms when hyperthyroid. The clinician should be alert to constellations of symptoms that gradually worsen over time. Cardiac symptoms usually resolve with correction of the excessive dosage. During the first 2 weeks of levothyroxine for congenital hypothyroidism, monitor neonates neonates carefully for cardiac overload, arrhythmias, and aspiration from avid suckling.[9][11][17][49]
Administration of levothyroxine resulting in suppressed serum thyrotropin (TSH) concentrations has been associated with bone loss and the potential increased risk for osteopenia and the premature development of osteoporosis. Because estrogen plays a protective role against bone loss, this increased risk is thought to be relevant in postmenopausal women receiving prolonged thyroid therapy. In a metananalysis, which pooled study data on the effects of slight over treatment with levothyroxine on pre- and postmenopausal women, a significant reduction in bone mass was observed in the postmenopausal study groups. Pooled study data contained skeletal measurements of the distal forearm, femoral neck, and lumbar spines of postmenopausal women. For all postmenopausal women, a theoretical bone consisting of 11.3% distal forearm, 42% femoral neck, and 46.7% lumbar spine was constructed (n = 317 measurements). Data showed that a postmenopausal woman at an average age of 61.2 years and treated with levothyroxine for 9.93 years (leading to suppressed serum TSH) would have an excess loss of bone mass of 9.02%; corresponding to an excess annual loss of 0.91% after 9.93 years of levothyroxine treatment as compared to healthy postmenopausal women.[50][51]
This list may not include all possible adverse reactions or side effects. Call your health care provider immediately if you are experiencing any signs of an allergic reaction: skin rash, itching or hives, swelling of the face, lips, or tongue, blue tint to skin, chest tightness, pain, difficulty breathing, wheezing, dizziness, red, a swollen painful area/areas on the leg.
Levothyroxine is classified in FDA pregnancy risk category A.[11] Thyroid hormones undergo minimal placental transfer and human experience does not indicate adverse fetal effects; do not discontinue needed replacement during pregnancy. Also, hypothyroidism diagnosed during pregnancy should be promptly treated. Measure TSH during each trimester to gauge adequacy of thyroid replacement dosage since during pregnancy thyroid requirements may increase. Immediately after obstetric delivery, dosage should return to the pre-pregnancy dose, monitor a serum TSH 6-8 weeks postpartum to assess for needed adjustments.
Thyroid hormones, like levothyroxine, are generally compatible with breast-feeding; minimal amounts of thyroid hormones are excreted in breast milk. The American Academy of Pediatrics considers the use of levothyroxine to be usually compatible with breast-feeding due to a lack of reported adverse effects in nursing infants.[12] It should be noted that in general, adequate thyroid replacement doses are needed to maintain normal lactation; levothyroxine is often the drug of choice to treat hypothyroidism during pregnancy and lactation. Comparisons of the levels of TSH and other thyroid function tests between breast-fed and bottle-fed infants have been published.[13][14][15] Breast milk does not provide sufficient levothyroxine (T4) or liothyronine (T3) to prevent the effects of congenital hypothyroidism; therefore serum levels of TSH in breast-fed hypothyroid infants are markedly elevated.[13][14] Euthyroid babies who were breast-fed did not have differences in TSH levels when compared to euthyroid babies receiving formula feedings.[15][16]
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond use date. Do not flush unused medications or pour down a sink or drain.
- Hamburger JI. Letter. Ann Intern Med 1984;101:140-1.
- Dong BJ, Hauck WW, Gambertoglio JG, et al. Bioequivalence of generic and brand-name levothyroxine products in the treatment of hypothyroidism. JAMA Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.7;277:1205-13.
- Fish LH, Schwartz HL, Cavanaugh J, et al. Replacement dose, metabolism, and bioavailability of levothyroxine in the treatment of hypothyroidism. N Engl J Med 1987;316:764-70.
- Blouin RA, Clifton GD, Adams MA, et al. Biopharmaceutical comparison of two levothyroxine sodium products. Clin Pharm 1989;8:588-92.
- Rennie D. Thyroid storm. JAMA Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.7;277:1238-43.
- Dickerson RN, Maish GO 3rd, Minard G, Brown RO. Clinical relevancy of the levothyroxine-continuous enteral nutrition interaction. Nutr Clin Pract. 2010;25:646-652.
- Hennessey JV, Wartofsky L. Thyroxine preparations. Ann Intern Med 1984;101:140.
- Stoffer SS, Szpunar WE. Potency of levothyroxine products. JAMA 1984;251:635-6.
- Tirosint (levothyroxine sodium capsule) package insert. Cranford, NJ: Akrimax Pharmaceuticals, LLC; 2013 Jan.
- Synthroid (levothyroxine) tablets. North Chicago, IL: Abbott Pharmaceuticals; 2012 Sep.
- Levothroid (levothyroxine sodium tablet) package insert. Shenandoah, IA: Lloyd Pharmaceutical; 2011 June.
- American Academy of Pediatrics (AAP) Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics 2001;108:776-89.
- Abbassi V, Steinour TA. Successful diagnosis of congenital hypothyroidism in four breast-fed neonates. J Pediatr 1980:97:259-61.
- Letarte J, Guyda H, Dussault JH, et al. Lack of protective effect of breast-feeding in congenital hypothyroidism: report of 12 cases. Pediatrics 1980;65:703-5.
- `Mizuta H, Amino N, Ichihara K, et al. Thyroid hormones in human milk and their influence on thyroid function of breast-fed babies. Pediatr Res 1983;17:468-71.
- Franklin R, O’Grady C, Carpenter L. Neonatal thyroid function: comparison between breast-fed and bottle-fed infants. J Pediatr 1985;106:124-6.
- Levoxyl (levothyroxine sodium tablet) package insert. Bristol, TN: King Pharmaceuticals, Inc.; 2008 Aug.
- Benvenga S, Bartolone L, Pappalardo MA, et al. Altered intestinal absorption of L-thyroxine caused by coffee. Thyroid 2008;18:293-301.
- Divi RL, Chang HC, Doerge Dr. Anti-thyroid isoflavones from soybean; isolation, characterization, and mechanisms of action. Biochem Pharmacol Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.7;54:1087-96.
- Questran® and Questran® Light (cholestyramine) package insert. Spring Valley, NY: Par Pharmaceutical Inc; 2002 July.
- Colestid® and Flavored Colestid® (colestipol) package insert. Kalamazoo, MI: Pharmacia & Upjohn Company; 2002 July.
- Sperber AD, Liel Y. Evidence for interference with the intestinal absorption of levothyroxine sodium by aluminum hydroxide. Arch Int Med Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.2;152:183.
- Singh N, Weisler SL, Hershman JM. The acute effect of calcium carbonate on the intestinal absorption of levothyroxine. Thyroid 2001;11:967-71.
- Campbell N. Ferrous sulfate reduces thyroxine efficacy in patients with hypothyroidism. Ann Int Med Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.2;117:1010.
- Hoffman BB, Lefkowitz RJ. Catecholamines and sympathomimetic drugs. Gilman AG, Rall TW, Nies AS, Taylor P, (eds.) In: Goodman and Gilman’s Pharmacological Basis of Therapeutics. 8th ed., New York, Pergamon Press. Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.0. 187-91.
- Finch CK, Chrisman CR, Baciewicz AM, et al. Rifampin and rifabutin drug interactions: an update. Arch Intern Med 2002;162:985-92.
- Dilantin® Kapseals® (extended phenyotin sodium capsules, USP) package insert. Morris Plains, NJ: Parke Davis; Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.9 Aug.
- Hansten P, Horn J. The Top 100 Drug Interactions: A Guide to Patient Management. includes table of CYP450 and drug transporter substrates and modifiers (appendices). H & H Publications, LLP 2014 edition.
- Gericke KR. Possible interaction between warfarin and fluconazole. Pharmacotherapy 1993;13:508-9.
- Cordarone® (amiodarone) package insert. Philadelphia, PA: Wyeth Laboratories; 2007 Mar.
- Amoxapine package insert. Corona, CA: Watson Laboratories, Inc.; 2007 Aug.
- Ludiomil (maprotiline hydrochloride) package insert. Summit, NJ: Ciba-Geigy Corporation; 1996 Nov.
- Cytomel® (liothyronine) package insert. St. Louis, MO: Jones Pharma Incorporated; 2001 Nov.
- Videx® (didanosine chewable/dispersible buffered tablets and pediatric powder for oral solution) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2006 Jan.
- Lanzafame M, Trevenzoli M, Faggian F, et al. Interaction between levothyroxine and indinavir in a patient with HIV infection. Infection 2002;30:54-5.
- Siraj ES, Gupta MK, Reddy SK. Raloxifene causing malabsorption of levothyroxine. Arch Intern Med 2003;163:1367-70.
- Vesanoid® (tretinoin) capsules package insert. Nutley, NJ: Roche Laboratories Inc.; 2004 Oct.
- Griffin JP. A review of the literature on benign intracranial hypertension associated with medication. Adverse Drug React Toxicol Rev 1992;11:41-57. Review.
- Lee AG. Pseudotumor cerebri after treatment with tetracycline and isotretinoin for acne. Cutis 1995;55:165-8. Review.
- Meier DA, Brill DR, Becker DV, et al. Society of Nuclear Medicine procedure guideline for therapy of thyroid disease with iodide-131 (sodium iodide). Retrieved January 26, 2006. Available on the World Wide Web at http://interactive.snm.org/docs/Therapy%20of%20Thyroid%20Disease%20with%20Iodine-131%20v2.0.pdf
- Jin M, Shimada T, Shintani M, et al. Long-term levothyroxine treatment decreases the oral bioavailability of cyclosporin A by inducing P-glycoprotein in small intestine. Drug Metab Pharmacokinet 2005;20:324-30.
- Siegmund W, Altmannsberger S, Paneitz A, et al. Effect of levothyroxine administration on intestinal P-glycoprotein expression: consequences for drug disposition. Clin Pharmacol Ther 2002;72:256-64.
- Welchol® (colesevelam) tablets package insert. Parsipanny, NJ: Daiiki Sankyo; 2006 Sept.
- Freeman MP, Freeman SA. Lithium: clinical considerations in internal medicine. Am J Med 2006;119:478-81.
- Filippatos TD, Derdemezis CS, Gazi IR, et al. Orlistat-associated adverse effects and drug interactions. A critical review. Drug Saf 2008;31:53-65.
- Tirosint™ (levothyroxine sodium) package insert. Institut Biochimique SA (IBSA): Switzerland; 2007 Dec.
- Renagel® (sevelamer) package insert. Cambridge, MA: Genzyme Corporation; 2004 Feb.
- Kalarickal J, Pearlman G, Carlson HE. New medications which decrease levothyroxine absorption. Thyroid 2007;17:763-5.
- Levothyroxine injection package insert. Schaumburg, IL: APP Pharmaceuticals, LLC; 2012 Dec.
- Samuels MH. Subclinical thyroid disease in the elderly. Thyroid 1998;8:803-13.
- Faber J, Galloe AM. Changes in bone mass during prolonged subclinical hyperthyroidism due to L-thyroxine treatment: a meta-analysis. Eur J Endocrinol 1994;130:350-6.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.




 Liothyronine Sodium / Levothyroxine Sodium Capsules
Liothyronine Sodium / Levothyroxine Sodium Capsules Liothyronine Sodium Capsules
Liothyronine Sodium Capsules Thyroid Tablets
Thyroid Tablets Testosterone Cream
Testosterone Cream Testosterone Cypionate Injection
Testosterone Cypionate Injection Progesterone Injection
Progesterone Injection Testosterone Vaginal Cream
Testosterone Vaginal Cream