Product Overview
† commercial product
Diethylpropion hydrochloride is a sympathomimetic amine that has been used for more than six decades as a short-term adjunct to caloric restriction and lifestyle modification in adults with exogenous obesity. As the N,N-diethyl analog of cathinone, it is structurally related to amphetamine but possesses a more favorable central-to-peripheral activity ratio, yielding anorectic effects with comparatively milder psychostimulant activity. Clinically, the drug is supplied as immediate-release 25 mg tablets taken three times daily and as extended-release 75 mg tablets administered once daily; both formulations are prescription-only and classified as Schedule IV under the U.S. Controlled Substances Act, reflecting a recognized though lower potential for abuse relative to Schedule II stimulants. Pharmacokinetic studies show rapid gastrointestinal absorption, hepatic N-de-ethylation, and urinary elimination of active aminoketone metabolites within 48 h. In practice, prescribers limit therapy to a few weeks to mitigate tolerance, and treatment is discontinued if the patient fails to lose at least 4 lb in the first month.[1]
Although not approved for pediatric use, diethylpropion has occasionally been studied in adolescents under specialist supervision. Because it shares mechanistic features with other sympathomimetic anorectics, baseline cardiovascular evaluation is customary before initiation, particularly in patients with underlying hypertension or valvular abnormalities. The prescribing information emphasizes that the compound is intended to complement-not replace-nutritional, behavioral, and exercise interventions, and that abrupt cessation after prolonged high-dose exposure could precipitate fatigue or depressive mood. Commercially manufactured tablets are typically white, biconvex, and film-coated; compounded versions must conform to United States Pharmacopeia assays for content uniformity and dissolution. All dispensing must occur through pharmacies operating under section 503A of the Federal Food, Drug, and Cosmetic Act, and labels must carry the caution that safety and efficacy for long-term weight management have not been established by the Food and Drug Administration.[2]
Immediate-release tablets are typically initiated at 25 mg taken orally three times daily, one hour before meals, with an optional 25 mg dose in mid-afternoon if appetite resurges. Extended-release 75 mg tablets are swallowed intact once each morning to provide all-day coverage; chewing or crushing defeats the controlled-delivery matrix and risks rapid absorption with exaggerated sympathomimetic effects. Therapy extending beyond 12 weeks is not recommended, and guidelines advise discontinuation if the patient fails to lose at least 5% of baseline weight within that interval.[13]
Pharmacokinetic modeling indicates linear exposure over the usual dose range, with no accumulation in normal renal function. However, in individuals with acidic urine the parent compound is reabsorbed more readily, potentially prolonging systemic presence; dosing adjustments are not formally required, but clinicians should counsel patients regarding concurrent ascorbic-acid ingestion, which may lower urinary pH.[14] Evening administration is discouraged because plasma peaks three to four hours post-dose can impair sleep initiation.
Diethylpropion acts primarily by increasing synaptic concentrations of norepinephrine and, to a lesser extent, dopamine within hypothalamic feeding centers. It achieves this through vesicular release and reuptake inhibition, thereby amplifying catecholaminergic signaling that promotes satiety and blunts hunger perception. Electrophysiologic data demonstrate heightened firing of pro-opiomelanocortin neurons and concomitant suppression of neuropeptide Y expression, neurochemical changes that collectively decrease caloric intake.[3] This central action is complemented by modest peripheral β-adrenergic stimulation, resulting in transient elevations of metabolic rate and thermogenesis but also posing theoretical risks of tachycardia and hypertension in susceptible individuals.
Extended-release tablets employ a non-eroding hydrophilic matrix that provides biphasic drug liberation: an initial diffusion-controlled burst followed by zero-order release over 12 h. Steady-state pharmacokinetics reveal mean peak plasma concentrations near 150 ng/mL, with apparent elimination half-lives for active metabolites between four and six hours; parental compound usually constitutes less than 2 % of the urinary excreted dose.[4] Tolerance to the anorectic effect emerges in some patients as hypothalamic receptors down-regulate, a phenomenon observed in rodent models after two weeks of continuous exposure and mirrored clinically by diminishing weight-loss trajectories. Abrupt dose escalation is discouraged, as higher sympathetic stimulation increases the likelihood of adverse cardiovascular events without restoring efficacy.
Therapy is contraindicated in patients with advanced arteriosclerosis, moderate-to-severe hypertension, hyperthyroidism, glaucoma, agitated states, or a history of substance-use disorder. Individuals receiving monoamine oxidase inhibitors must discontinue those agents for at least fourteen days before diethylpropion to avoid hypertensive crisis. Cardiac valvulopathy and primary pulmonary hypertension, albeit rare, have been documented after prolonged appetite-suppressant use; therefore, diethylpropion is avoided in patients with echocardiographic evidence of structural heart disease.[5]
Genetic susceptibility factors further complicate risk assessment: case reports link bone morphogenetic protein receptor type II mutations to heightened vulnerability for drug-induced pulmonary hypertension, suggesting that undiagnosed carriers may face disproportionate hazards even at recommended doses. In addition, diethylpropion should not be administered concurrently with other sympathomimetics such as phentermine, pseudoephedrine, or attention-deficit medications, as additive catecholaminergic activity may precipitate arrhythmia or cerebrovascular insult.[6]
Pharmacodynamic interaction with monoamine oxidase inhibitors constitutes the most serious concern; concurrent use can trigger rapid accumulation of norepinephrine, culminating in malignant hypertension, hyperthermia, or serotonergic features. Patients must observe a two-week wash-out interval when switching between these classes.[7] Less severe but clinically relevant interactions include potentiation of pressor response to adrenergic blockers withdrawn abruptly, attenuation of antihypertensive efficacy of β-blockers via reflex sympathetic drive, and potential additive insomnia when combined with other central stimulants or high-dose caffeine.
Clinical policy guidelines also caution against co-administration with serotonergic agents such as selective serotonin reuptake inhibitors, not because of classic serotonin-syndrome synergy but owing to overlapping adverse-event profiles of anxiety, tremor, and palpitations.[8] Ethanol may amplify diethylpropion-induced impairment of motor coordination, and prescribers advise patients to avoid operating heavy machinery until individual sensitivity is known. Despite metabolic involvement of hepatic microsomal enzymes, clinically meaningful CYP-mediated interactions are minimal, as the drug undergoes primary carbonyl reduction and N-de-ethylation via nonspecific reductases.
Common dose-related reactions include dry mouth, insomnia, irritability, restlessness, and mild elevation of blood pressure. These typically emerge during the first week of therapy and often abate as patients acclimate. Less frequent events encompass dizziness, nausea, constipation, and mydriasis. Post-marketing surveillance highlights rare but serious complications such as myocardial infarction, cerebrovascular accident, and seizure, predominantly in individuals exceeding recommended dosages or combining diethylpropion with other stimulants.[9]
Clinical reviews underscore a potential association between chronic anorectic exposure and valvular heart disease, hypothesized to involve 5-HT₂B receptor activation on valvular interstitial cells; although direct evidence for diethylpropion is scant, clinicians remain vigilant, particularly in women of child-bearing age who may have unrecognized mitral-valve prolapse. Elevations in pulmonary arterial pressure have also been reported, necessitating discontinuation if new-onset dyspnea, edema, or syncope appears. Psychiatric adverse effects-mood swings, euphoria, dysphoria-occur primarily at supra-therapeutic levels and resolve after drug withdrawal.[10]
Animal studies conducted at doses several-fold higher than human exposure did not reveal teratogenicity, and epidemiologic data in humans have not established a causal link between diethylpropion and congenital anomalies. Nevertheless, weight-loss pharmacotherapy offers no benefit during gestation, and appetite suppressants may compromise fetal nutrition by reducing maternal caloric intake. Consequently, diethylpropion is generally avoided unless potential benefits clearly outweigh risks.[11]
Should inadvertent exposure occur, neonatal withdrawal-manifesting as jitteriness, respiratory distress, or poor feeding-has been described when mothers consume high sympathomimetic doses close to delivery. Supportive care is usually sufficient, but neonatologists should monitor infants for autonomic instability over the first 72 h postpartum.[12] Lactating women are counseled that the drug and metabolites pass into breast milk, and although quantities are small, theoretical concerns about infant irritability or growth suppression favor alternative postpartum weight-management strategies.
Tablets should be stored in tight, light-resistant containers at controlled room temperature-between 20 °C and 25 °C with brief excursions permitted to 15-30 °C-per current good manufacturing practices. The compound is hygroscopic; excessive humidity accelerates degradation of the extended-release polymer and may compromise drug-release kinetics, so desiccant packets are often included in commercial bottles.[15]
Compounded lots prepared under 503A must follow beyond-use dating of not more than six months unless stability-indicating assays justify extension. Freezing is contraindicated because thermal stress may induce microcracking of the sustained-release matrix, leading to dose dumping upon thaw. Pharmacists advise patients to keep the medication in its original container, away from direct sunlight or bathroom moisture, and to discard unused tablets after the printed expiration date to avoid subpotent dosing.[16]
- DrugBank Online. (2025). Diethylpropion: Uses, Interactions, Mechanism of Action. https://go.drugbank.com/drugs/DB00937
- DailyMed. (2019). Diethylpropion hydrochloride tablet, 25 mg-prescribing information. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=4fdbc049-6497-4ea0-8788-d2b2963328f7
- Medicine.com. (2020, February 9). Diethylpropion: Dosage, Mechanism/Onset of Action, Half-Life. https://www.medicine.com/drug/diethylpropion/hcp
- RSL Educational Series. (2024). Appetite Stimulants and Suppressants. https://www.iipseries.org/assets/docupload/rsl20249CE43BEA498317C.pdf
- Drugs.com. (2025). Diethylpropion extended-release: package insert. https://www.drugs.com/pro/diethylpropion-extended-release.html
- Gaine, S. (2003). Primary pulmonary hypertension after amfepramone exposure. European Respiratory Journal, 22(3), 560-563. https://publications.ersnet.org/content/erj/22/3/560
- HelloPharmacist. (2025). Linezolid and diethylpropion interaction details. https://hellopharmacist.com/drug-interactions/drugs/linezolid/diethylpropion-with-linezolid
- Health Net. (2025). Clinical Policy CP.CPA.328 Diethylpropion. https://www.healthnet.com/content/dam/centene/policies/pharmacy-policies/CP.CPA.328.pdf
- Drugs.com. (2025). Diethylpropion side effects: common, severe, long term. https://www.drugs.com/sfx/diethylpropion-side-effects.html
- Yanovski, J., & Yanovski, S. (2014). Long-term drug treatment for obesity. JAMA, 311(1), 74-86. https://jamanetwork.com/journals/jama/fullarticle/1774038
- Drugs.com. (2024). Diethylpropion use during pregnancy. https://www.drugs.com/pregnancy/diethylpropion.html
- American Academy of Pediatrics. (2012). Neonatal drug withdrawal. Pediatrics, 129(2), e540-e560. https://publications.aap.org/pediatrics/article/129/2/e540/32573
- DailyMed. (2022). Diethylpropion hydrochloride extended-release tablets, 75 mg-labeling. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=dab53f4f-68d4-4477-a2b6-ad44a956332b
- Parry, J. (1973). Metabolism and excretion of diethylpropion in man. Journal of Pharmacy and Pharmacology, 25(2), 119-126. https://academic.oup.com/jpp/article/25/2/119/6200938
- U.S. Food and Drug Administration. (2004). Diethylpropion hydrochloride labeling. https://www.accessdata.fda.gov/drugsatfda_docs/label/2004/11722s029,12546s032lbl.pdf
- ScienceDirect Topics. (2021). Diethylpropion overview. https://www.sciencedirect.com/topics/chemistry/diethylpropion
- Qeios. (2020). Diethylpropion profile. https://www.qeios.com/read/78L3EB/pdf
- Connecticut Drug Control Division. (2025). Diethylpropion schedule information. https://portal.ct.gov/dcp/drug-control-division/drug-control/diethylpropion
- Half-Life Calculator. (2025). Diethylpropion half-life calculator. https://half-life-calculator.com/drug/diethylpropion
- BuzzRx. (2024). Diethylpropion ER-common questions. https://www.buzzrx.com/diethylpropion-hcl-er/common-questions
- Drugs.com. (2025). Diethylpropion monograph for professionals. https://www.drugs.com/monograph/diethylpropion.html
- Teichert, M. (2023). Long-term cardiovascular risk after sympathomimetic amine treatment. European Heart Journal Supplements, 44(S2), ehad655.2760. https://academic.oup.com/eurheartj/article/44/Supplement_2/ehad655.2760/7390816
- Vernon, G. (2020). Cardiovascular effects of stimulant therapies: review topic of the week. Journal of the American College of Cardiology, 75, 256-268. https://www.sciencedirect.com/science/article/pii/S0735109720357417
- Ghosh, M. N., & Parvathy, S. (1976). Tolerance pattern of anorexigenic drugs in rats. British Journal of Pharmacology, 57, 479-486. https://bpspubs.onlinelibrary.wiley.com/doi/epdf/10.1111/j.1476-5381.1976.tb10374.x
- RxMed. (2025). Tenuate (diethylpropion) product monograph. https://www.rxmed.com/b.main/b2.pharmaceutical/b2.1.monographs/CPS-_Monographs-_T/TENUATE.html
- Pennsylvania Department of Health. (2022). Neonatal abstinence syndrome report. https://www.pa.gov/content/dam/copapwp-pagov/en/health/documents/topics/documents/opioids/2020%20NAS%20REPORT.pdf
What pharmacologic class does diethylpropion belong to?
It is a central sympathomimetic amine classified as an anorectic agent.[17]
Is this medication a controlled substance?
Yes; it is listed as Schedule IV, indicating moderate but recognized abuse potential.[18]
How long does a single dose remain active?
Peak effects wane after about six hours, while metabolites may persist in plasma for roughly one day.[19]
What is the usual treatment duration?
Clinical policies limit use to twelve weeks unless otherwise justified by ongoing weight loss and careful monitoring.[20]
May the extended-release tablet be split or crushed?
No; altering the dosage form can cause rapid release and heightened side-effect risk.[21]
Does the drug increase the chance of heart problems?
Long-term sympathomimetic exposure has been associated with small but measurable elevations in heart-failure and stroke risk, mandating cardiovascular screening.[22]
Can it be taken alongside antidepressants?
Caution is advised; combined adrenergic stimulation may intensify anxiety, tremor, or hypertension.[23]
Will tolerance develop over time?
Partial tolerance to appetite suppression often appears after several weeks, at which point dose escalation is not recommended.[24]
What signs suggest misuse or dependency?
Escalating self-dosing, drug-seeking behavior, or using the tablets for euphoria rather than weight loss warrant discontinuation and evaluation.[25]
Is diethylpropion recommended within comprehensive obesity guidelines?
Expert panels consider it a low-certainty option when newer agents are inaccessible or contraindicated.[26]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
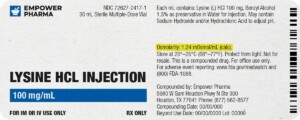
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.



 Phentermine HCl / Topiramate Capsules
Phentermine HCl / Topiramate Capsules Phentermine HCl Capsules
Phentermine HCl Capsules Bella Capsules
Bella Capsules Lipo Burn Capsules
Lipo Burn Capsules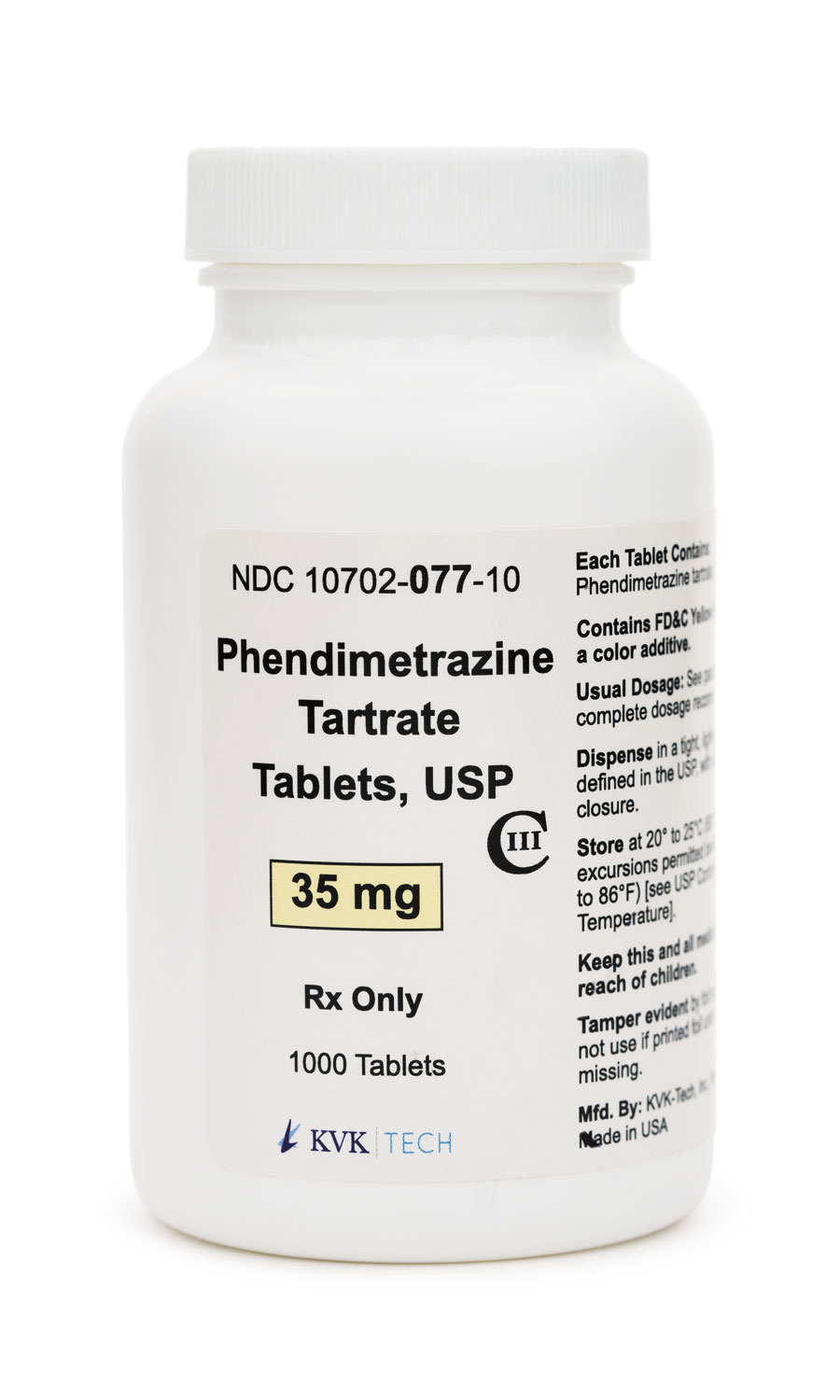 Phendimetrazine Tartrate Tablets
Phendimetrazine Tartrate Tablets Tirzepatide / Niacinamide Injection
Tirzepatide / Niacinamide Injection Cyanocobalamin (Vitamin B12) Injection
Cyanocobalamin (Vitamin B12) Injection