Product Overview
Dehydroepiandrosterone (DHEA) is a C19 steroid also known as 5-androsten-3 beta-ol-17-one. DHEA and DHEAS (an active, sulfated form of DHEA), are endogenous hormones secreted by the adrenal cortex in primates and a few non-primate species in response to ACTH. DHEA is a steroid precursor of both androgens and estrogens, and thus is often called ‘the mother hormone’. Endogenous DHEA is thought to be important in several endocrine processes, but current medical use of DHEA is limited to controlled clinical trials. In 1997, Pharmadigm, Inc. received an orphan drug designation to enroll patients with thermal burns who require skin-grafting into trials using injectable DHEAS, known as PB-005. Researchers continue to investigate the role of both endogenous and exogenous DHEA in CNS, psychiatric, endocrine, gynecologic and obstetric, immune, and cardiovascular functions.[1] GeneLabs Technologies, Inc., submitted an NDA in September 2000 for its proprietary DHEA product, called prasterone (Prestara™, formerly known Aslera™ or GL-701). Prasterone appears to attentuate some symptoms of mild-to-moderate systemic lupus erythematosus (SLE) and may increase bone density based on evidence from two phase III studies in women; studies in men with SLE are ongoing. The FDA placed Prestara™ under a 6-month priority review status in October 2000; on April 19, 2001 the FDA stated that although the drug showed advantages over placebo in one study, the advantages were not statistically significant. Additional data were submitted to the FDA following a ‘not approvable’ letter on June 26, 2001. On September 2, 2002, the FDA issued an ‘approvable’ letter for the Prestara™ product, but the agency has asked for additional clinical trial data regarding the drug’s effects on bone mineral density before granting final approval for SLE. The manufacturer began a confirmatory phase III trial in early 2003; the primary endpoint will be measurement of bone mineral density of the lumbar spine; the trial is targeted for completion at the end of 2003. In October 2004, the manufacturer released information that Prestara™ therapy did not meet the primary end point in the confirmatory trial. In August 2003, Paladin Labs Inc., received orphan drug designation from the FDA for prasterone, dehydroepiandrosterone, DHEA, under the brand name Fidelin™, for adrenal insufficiency.
Exogenously administered DHEA is sold as a nutritional supplement in health and drug stores and many older individuals are using it to ‘maintain the vitality of their youth’. There is currently no objective, well-controlled, large-scale, scientific evidence to back claims that taking DHEA combats the signs or symptoms of aging, diabetes, neurologic disease, sexual dysfunction, or heart disease.[2] Some athletes abuse DHEA believing that it can enhance the body’s synthesis of testosterone; the potential action of DHEA as an anabolic steroid has lead to the prohibition of supplementation in competitive sport, even though evidence of anabolic effects in athletes is lacking.[3] DHEA is also abused by athletes in an attempt to normalize the testosterone:epitestosterone ratio. However, the sensitivity and specificity of currently available testing for athletic ‘doping’ can readily identify the presence of banned substances, including testosterone. Because of DHEA’s complex physiologic actions, more than 500 scientific articles investigating it have been published since 1993. Many of the short-term trials of DHEA to date have lacked the rigor and statistical applications needed to support therapeutic claims. Most claims will need to be confirmed by large-scale, properly conducted, and controlled studies. In 1984, the FDA banned the non-prescription (OTC) sale of exogenous DHEA due to concern over hepatotoxicity (hepatitis and hepatic tumors) as noted in animal studies. The FDA formally relegated DHEA to a Category II OTC ingredient at that time (i.e., not generally recognized as safe and effective). However in 1994, the passage of the US Dietary Supplement Health and Education Act (DSHEA) allowed DHEA to be marketed as a nutritional or dietary supplement.
Endogenous DHEA is a complex hormone, and researchers still have much to discover in regards to its physiologic effects in males and females. Less is known regarding the mechanisms of action of exogenously administered DHEA.
CNS actions: Both DHEA and DHEAS may be synthesized de-novo by the central nervous system, and concentrations of DHEA and DHEAS are higher in the brain than in other organs. The two neurohormones appear to have excitatory activity at both GABA and NMDA receptors.[1]
Dermatologic actions after burn injury: Animal studies have suggested that DHEA and DHEAS expedite the re-epithelialization of donor skin-graft sites.[4]
Endocrine actions: Endogenous DHEA is synthesized by the conversion of cholesterol via CYP11A1 to pregnenolone, followed by CYP17 conversion to DHEA and then to DHEAS via dehydroepiandrosterone sulfatransferase. The synthesis of DHEA occurs exclusively in the adrenal cortex in women, while in men 10-25% of DHEA is synthesized by the testes and roughly 80% of the DHEA comes from the adrenal glands. DHEA is converted via hydrosteroid dehydrogenases and aromatase into androstenedione, testosterone, and estradiol by peripheral tissues. DHEA is of only minor importance as an androgenic substance itself. The production rate of DHEA by the body changes dramatically throughout life, typically peaking at adrenarche, the adrenal contribution to the onset of puberty. In males, DHEA serum levels are high in neonates right after birth, rapidly fall within 5 months, then begin to rise at the age of 9 years. Endogenous DHEA concentration then peaks again in males at roughly the 20th-30th years of life. In females, DHEA serum levels are high in neonates right after birth, rapidly fall within 5 months, then begin to rise at the age of 7 years. Endogenous DHEA concentration then peaks again in females at roughly the 20th and 40th year of life. DHEA levels decline steadily after the fifth decade in both males and females. DHEAS concentrations in males and females follow similar patterns. The administration of DHEA supplements results in different hormonal concentration changes in males and females; the actions are dependent on the dose, formulation and route of administration, and age of the person receiving the DHEA.[1]
Hemostasis: Inhibition of platelet aggregation by exogenous DHEA has been demonstrated in vivo in humans; DHEA either prolonged or completely inhibited the rate of arachidonate-stimulated platelet aggregation after 14 days of administration. The degree of inhibition of platelet aggregation was noted to be time and dose dependent.[5]
Immunologic actions: Because SLE occurs more frequently in women than men and because SLE is known to worsen during pregnancy, a hormonal etiology is suspected for this disease. DHEA up-regulates interleukin-2 (IL-2) production by T-lymphocytes in murine lupus models and reverses the clinical autoimmune disease. Lower endogenous levels of DHEA and DHEAS have been noted in both male and female patients with lupus at the time of diagnosis. Chronic corticosteroid treatment, which may cause adrenal atrophy, contributes to reduced DHEA levels in these patients. Supplementation of DHEA in SLE may augment immune system activity and potentially offset the undesired effects of chronic corticosteroid use in these patients.[6] Exact mechanisms of DHEA on immune function are not yet clear. DHEA has been shown to increase the numbers of natural killer cells in aging women. Serum DHEA levels are observed to be reduced in patients with AIDS or age-related immunodeficiency, suggesting that DHEA may serve as a marker of the integrity of the immune system. No studies to date have shown that DHEA supplementation augments currently available therapies for AIDS.[1]
Your health care provider needs to know if you have any of these conditions: breast cancer (men or women); cancer of the lining of the uterus (endometrial cancer); diabetes or high blood sugar; immune system problems; infertility; liver disease; post-menopause; prostate cancer or an enlarged prostate gland; rheumatoid arthritis; uterine cancer; vaginal bleeding or menstrual problems; vaginal cancer; an unusual or allergic reaction to progesterone, DHEA, soy, other medicines, foods, dyes, or preservatives; pregnant or trying to get pregnant; breast-feeding. Visit your doctor or health care professional for regular checks on your progress. Women should inform their doctor if they wish to become pregnant or think they might be pregnant. There is a potential for serious side effects to an unborn child. DHEA use is banned in competitive sports. Both college (NCAA) and olympic (USOC) committees do not allow DHEA use among athletes.
NOTE: DHEA has not yet been evaluated by the Food and Drug Administration. Nutritional supplement products containing DHEA are not intended to diagnose, treat, cure, or prevent any disease. Consumers should also be informed that rigid quality control standards are not required for nutraceuticals and substantial variability can occur in both the potency and the purity of these products.
Dehydroepiandrosterone (free and sulfate) test systems measure dehydroepiandrosterone (DHEA) and its sulfate (DHEAS) in urine, serum, plasma, and amniotic fluid. These measurements are used in the diagnosis and treatment of DHEA-secreting adrenal cancers. It is unclear at this time if supplementation with DHEA would result in false-positives of these tests.
The effect of DHEA on hormone-dependent tumors in males and females is unknown. Many hormonal agents with androgenic or estrogenic activity are contraindicated for use in persons with various hormonally-dependent neoplasms. Some data suggests an association between elevated endogenous DHEA and DHEAS serum concentrations and the development of breast cancer andovarian cancer in women. As with other hormones, DHEA supplementation in a woman with undiagnosed abnormal vaginal bleeding, endometrial cancer, endometrial hyperplasia, uterine cancer, or vaginal cancer is not recommended. DHEA may stimulate the growth of cancerous tissue and should not be used in male patients with either breast or prostate cancer. Male patients with symptoms of prostatic hypertrophy or erectile dysfunction that have not been medically evaluated should not take DHEA supplements. Because the incidence of some hormonally-dependent cancers naturally increases with age, “andropausal” men and post-menopausal women should approach DHEA supplementation with caution. It is recommended that a qualified healthcare prescriber’s recommendations be sought prior to DHEA supplementation.[7] Benefit versus risk should be determined individually. Women taking DHEA should receive an annual clinical breast examination and pelvic examination and regular mammograms as recommended by their healthcare professional. Men taking DHEA should receive annual physical examinations, including prostate examination or PSA levels, as recommended by their healthcare provider.
Dehydroepiandrosterone, DHEA is contraindicated for use in children <= 18 years of age. Because endogenous DHEA, DHEAS, and androstenedione serum concentrations are related to the onset of puberty, there is concern that the use of DHEA supplements in children or adolescents would interfere with natural growth and sexual maturation.
Females of childbearing age with infertility due to hyperandrogenism or chronic anovulation should not take DHEA supplements. The relationship of DHEA and DHEAS to ovulation and fertility is complex and still poorly understood. However, women with hirsutism and infertility or polycystic ovary syndrome (PCOS) are commonly found to have elevated endogenous DHEA or DHEAS serum concentrations on assay.[8] Women with higher serum levels of endogenous DHEAS and who are receiving fertility treatments have been noted to have higher rates of ovarian hyperstimulation syndrome (OHSS) associated with their treatments. DHEA may also induce changes in the normal menstrual cycle in women of childbearing age.
Dehydroepiandrosterone, DHEA should be considered a pregnancy category X drug, similar to other androgenic hormones. Studies of the role of endogenous fetal and maternal DHEA in pregnancy indicate that the ratio of DHEA or DHEAS to other hormones in the serum or placenta may influence the processes of fetal development, parturition, and labor. Endogenous DHEA and DHEAS appear to be important in the functional development of the adrenal cortex and other endocrine activities in the fetus; it is assumed that exogenous DHEA supplementation to a pregnant woman could potentially have deleterious effects on fetal development or viability. The androgenic effects of DHEA could potentially result in masculinization of a female fetus. No controlled trials of DHEA in primate or human gestation exist. Do not administer DHEA to a pregnant woman.
DHEA is a hormone and should not be supplemented in a lactating woman who is breast-feeding her infant. Most hormones are excreted in breast milk. Like other androgenic hormones, it is possible that DHEA could inhibit lactation. It is unknown what effect DHEA would have on the breast-feeding infant.
Dehydroepiandrosterone, DHEA should be considered contraindicated for use in patients with hepatic disease, hepatitis,hepatocellular cancer, or jaundice. In 1984, the FDA banned the non-prescription (OTC) sale of DHEA due to concern over its ability to cause hepatotoxicity. DHEA supplements are now able to be sold as “nutritional supplements” secondary to the US Dietary Supplement Health and Education Act (DSHEA) of 1994, and are no longer regulated as drugs outside of clinical trials. Transient drug-induced hepatitis has been reported in association with the use of DHEA nutritional supplements. Because both estrogens and androgens may exacerbate acute intermittent or variegate hepatic porphyria, DHEA, which has androgenic actions, should be used with caution in patients with these diseases.
Treatment of patients with diabetes mellitus with DHEA is currently not warranted. The role of endogenous DHEA in relationship to insulin resistance is not clear. DHEA and DHEAS may not be mediators of insulin action. Long-term trials evaluating the effectiveness and safety of exogenous DHEA supplementation in patients with diabetes are currently unavailable. Patients with diabetes mellitus who are pursuing the use of DHEA supplements should see a qualified health care professional.[9]
DHEA treatment of patients with human immunodeficiency virus (HIV) infection should be approached with caution. DHEA may possess immunomodulating effects, perhaps by enhancing the secretion of IL-2 from activated T cells as demonstrated in murine models. While this suggests that DHEA may play a role in the function of the immune system, the role of DHEA supplementation in the treatment of human HIV infection, especially acquired immunodeficiency syndrome (AIDS), has not yet been determined. Safety and efficacy have not been established.[10]
Most non-essential hormones are discontinued several weeks prior to major surgery where feasible. DHEA may inhibit platelet aggregation, an effect that may be important to consider during surgical procedures. The decision of when to resume DHEA after surgery would be based on the perceived additional risk from DHEA use and the need for DHEA therapy.
Soy oil is the raw product from which many DHEA supplements are manufactured. Cholesterol from soy oil is converted into DHEA. DHEA products should be used cautiously in patients with a history of allergies to soy-containing foods or who exhibit immediate-type soya lecithin hypersensitivity.
One of the functions of endogenous DHEA is to inhibit the enzyme glucose-6-phosphate dehydrogenase. Use DHEA with caution in patients with G6PD deficiency.
Prasterone (DHEA) should be used with caution in patients with bipolar disorder. One case report exists of the appearance of mania in a predisposed patient consuming large doses of a DHEA supplement on a routine basis. Until more information is known, clinicians should be aware that emotional lability or changes in mood may occur in selected patients.
NOTE: Many prasterone, dehydroepiandrosterone, DHEA preparations contain a variety of other ingredients, including minerals, vitamins, hormones and/or herbs, and each individual component may need to be evaluated for the presence of drug interactions. Only drug interactions pertaining to DHEA are discussed in this monograph.
Prasterone, dehydroepiandrosterone, DHEA is converted via hydrosteroid dehydrogenases and aromatase into androstenedione, testosterone, and estradiol by peripheral tissues.[11] DHEA is a weak androgen that has complex hormonal effects. It is unclear what actions prasterone, dehydroepiandrosterone, DHEA would have on other exogenous hormonal regimens (e.g., androgens, estrogens, oral contraceptives, or progestins). Either additive or antagonistic effects could potentially occur. The mechanisms or results of interactions with DHEA and other hormones may be multifactorial and dependent on the sex and age of the individual being treated, the indication for hormone use, the route by which DHEA is given, and the length of concomitant use. Concurrent use of DHEA with any of these hormonal regimens is not recommended at this time.
Prasterone, dehydroepiandrosterone, DHEA is converted via hydrosteroid dehydrogenases and aromatase into androstenedione, testosterone, and estradiol by peripheral tissues.[11] DHEA is a weak androgen that has complex hormonal effects. It is unclear what actions prasterone, dehydroepiandrosterone, DHEA would have on other exogenous hormonal regimens. It would seem prudent to not administer DHEA with infertility or hormonal cancer treatments such as GnRH analogs (cetrorelix, ganirelix, goserelin, histrelin, leuprolide, or triptorelin) since DHEA may theoretically interfere with these therapies.
Prasterone, dehydroepiandrosterone, DHEA is converted via hydrosteroid dehydrogenases and aromatase into androstenedione, testosterone, and estradiol by peripheral tissues.[11] DHEA is a weak androgen that has complex hormonal effects. The action of 5-alpha reductase inhibitors (i.e., dutasteride, finasteride) could potentially be antagonized by DHEA administration. 5-alpha-reductase inhibitors have anti-androgenic effects on the prostate gland that may be antagonized by the androgenic effects of DHEA on these tissues. Avoid concurrent use.
Drug interactions with Saw palmetto, Serenoa repens have not been specifically studied or reported. Saw palmetto extracts appear to have antiandrogenic effects.[12][13] The antiandrogenic effects of Saw palmetto, Serenoa repens would be expected to antagonize the actions of androgens; it would seem illogical for patients taking androgens to use this herbal supplement.
Corticosteroids blunt the adrenal secretion of endogenous DHEA and DHEAS, resulting in reduced DHEA and DHEAS serum concentrations. The impact of exogenous prasterone, dehydroepiandrosterone, DHEA administration on the safety or efficacy of chronic corticosteroid treatment regimens is not yet clear. The administration of DHEA to patients on corticosteroids should only be done under the observation of a qualified health care professional.[14]
Prasterone, dehydroepiandrosterone, DHEA appears to have anti-platelet effects, which may prolong bleeding times.[15] Inhibition of platelet aggregation by DHEA has been demonstrated in vivo in humans; the rate of arachidonate-stimulated platelet aggregation was prolonged or completely inhibited.[15] In addition, DHEA is converted to androgens and estrogens within the human body and thus may affect hemostasis via androgenic or estrogenic effects. Estrogens increase the production of clotting factors VII, VIII, IX, and X.[16] Androgens, such as testosterone, increase the synthesis of several anticoagulant and fibrinolytic proteins. Because of these potential, varied effects on coagulation, patients receiving DHEA concurrently with anticoagulants (e.g., warfarin or heparin) or other platelet inhibitors, including aspirin, ASA should be monitored for side effects or the need for dosage adjustments.
Concurrent use of antidiabetic agents with prasterone, dehydroepiandrosterone, DHEA is currently not warranted. The role of endogenous DHEA in relationship to insulin action or glucose intolerance is not clear. Endogenous levels of DHEA and DHEAS may be regulated by insulin and may not mediate insulin action. It is unclear what effect DHEA supplementation would have on glycemic control. Trials evaluating the effectiveness and safety of exogenous DHEA supplementation in combination with antidiabetic agents are currently unavailable.[17]
Prasterone, dehydroepiandrosterone, DHEA is converted via hydrosteroid dehydrogenases and aromatase into androstenedione, testosterone, and estradiol by peripheral tissues.[11] Prasterone or DHEA supplements should not be given concurrently with any aromatase inhibitors, as DHEA could interfere with the pharmacologic action of the aromatase inhibitor and compromise aromatase inhibitor effectiveness. Conversely, aromatase inhibitors (e.g., aminoglutethimide, anastrozole, exemestane, letrozole, testolactone, vorozole) could interfere with biotransformation of DHEA.
Prasterone, dehydroepiandrosterone, DHEA may inhibit the metabolism of triazolam, and other benzodiazepines (e.g., alprazolam, estazolam, midazolam) which undergo CYP3A4-mediated metabolism. In one study of elderly volunteers, half of the patients received DHEA 200 mg/day PO for 2 weeks, followed by a single dose of triazolam 0.25 mg. Triazolam clearance was reduced by close to 30% in the DHEA-pretreated patients vs. the control group; however, the effect of DHEA on CYP3A4 metabolism appeared to vary widely among subjects.[18] While more study is needed, benzodiazepine-induced CNS sedation and other adverse effects might be increased in some individuals if DHEA is co-administered.
Prasterone, dehydroepiandrosterone, DHEA is a weak androgen that has complex hormonal effects.[11] Androgens are known to stimulate erythropoiesis.[19] Despite the fact that endogenous generation of erythropoietin is depressed in patients with chronic renal failure, other tissues besides the kidney can synthesize erythropoietin, albeit in small amounts. Concurrent administration of androgens can increase the patient’s response to epoetin alfa, reducing the amount required to treat anemia. Because adverse reactions have been associated with an abrupt increase in blood viscosity, this drug combination should be avoided, if possible. Further evaluation of this combination needs to be made.
In vitro, both genistein and daidzein inhibit 5 alpha-reductase isoenzyme II, resulting in decreased conversion of testosterone to the potent androgen 5-alpha-dihydrotestosterone (DHT) and a subsequent reduction in testosterone-dependent tissue proliferation.[20] The action is similar to that of finasteride, but is thought to be less potent. Theoretically, because the soy isoflavones appear to inhibit type II 5-alpha-reductase, the soy isoflavones may counteract the activity of the androgens.
NOTE: Some prasterone, dehydroepiandrosterone, DHEA preparations are a combination of several hormones and/or herbs, and each individual component may need to be evaluated in the presence of adverse reactions. Only adverse reactions pertaining to DHEA are discussed in this monograph. Human side-effect data to date have been collected in non-systematic fashion via the FDA special nutritional adverse effect monitoring system (SNAEMS) or relatively small clinical trials.
DHEA has been observed to cause reversible reductions in HDL cholesterol and total cholesterol in some clinical trials; other trials have not noted changes in the serum lipid profile. DHEA may also exhibit anti-platelet effects. The influence of these changes on the development of side effects, atherosclerosis, or other cardiac-related endpoints is unknown.
In one 3-month study of 28 women with SLE, the following ADRs were noted in the females receiving DHEA: acneiform rash (57%), hirsutism (14%), weight gain (14%), menstrual irregularity (7%), and emotional lability (7%). The statistical significance of these side effects relative to placebo was not determined.[21] Some events commonly associated with SLE and reported as adverse events in clinical trials were less frequent in patients treated with prasterone (GL701) compared with placebo, including muscle pain, nasal and oral ulceration, and hair loss.
Prasterone, DHEA is a hormone with androgenic actions, however, the incidence of androgenic side effects is not known. When androgens are given to women, they may cause virilization, manifested by clitoromegaly, reduced breast size, and deepening of the voice or voice hoarseness. If treatment is discontinued when these symptoms first appear, they usually subside. Prolonged treatment with androgenic substances can lead to irreversible masculinity, so the benefit of DHEA treatment should be offset against the risk of androgen-like side effects.
The effect of prasterone or DHEA supplementation on normal endocrine processes in women is not clear. Women should report any menstrual changes, including amenorrhea, unusual vaginal bleeding, dysmenorrhea, or abdominal bloating to their health care providers. Breast changes, including breast discharge, breast enlargement, breast tenderness, or galactorrhea should also be reported.
Prasterone (DHEA) has androgenic actions, and it is not clear what effect prasterone may have in male patients. Similar to female patients, male patients may experience worsening of acne vulgaris. Male patients may theoretically experience feminization during prolonged therapy with DHEA resulting from inhibition of gonadotropin secretion and conversion of testosterone to estrogens. Feminizing effects in males might include gynecomastia. Feminizing effects secondary to androgens are generally reversible. It is not clear if DHEA would affect testicular function or prostatic function. Symptoms of urinary retention or urinary urgency, prostate pain, or signs of an enlarged prostate in a male patient should prompt clinical evaluation.
Mild peripheral edema can occur with DHEA use as the result of increased fluid retention (in association with sodium retention) and may be associated with mild weight gain.
Prasterone (DHEA) may cause emotional lability. At least one case of possible DHEA-induced mania has been reported in the literature, in a patient predisposed to bipolar illness who was consuming doses >= 300 mg/day PO on a routine basis. There was a temporal association between the time of drug use and the appearance of manic symptoms. Clinicians should be alert to possible alterations in psychiatric status in patients taking this medication for supplemental or medicinal purposes.
Hepatic dysfunction can occur from use of androgenic steroids, especially the oral 17-alpha-alkylandrogens (e.g., methyltestosterone). DHEA does not contain the 17-alkyl group in its structure, however, transient cases of drug-induced hepatitis in humans have been reported in association with DHEA use; these have included a few reports to the FDA Special Nutritionals Adverse Event Monitoring System (SN/AEMS). Liver toxicity has not been reported in human studies, but elevated hepatic transaminases have been reported and confirmed upon rechallenge in some trials. In 1984, the FDA banned the non-prescription (OTC) sale of DHEA due to concern over hepatitis. Clastogenesis has been noted in hepatic tissues of animals exposed to DHEA. DHEA appears to act as a perisoxome proliferator, resulting in liver tumors and nodules in the periportal areas of the liver lobule in rats. DHEA should be discontinued in any patient developing signs or symptoms of potential liver problems, including elevated hepatic enzymes, continued nausea and vomiting, fatigue, jaundice, or severe abdominal pain; the patient should be evaluated.
In studies of male patients with HIV virus infection, side effects attributed to DHEA treatments and confirmed upon rechallenge included nasal congestion, fatigue, headache, and mild insomnia.[1]
Prasterone (DHEA) therapy is reported to cause libido increase. No objective evidence of this side effect exists at this time.
The effect of DHEA on the progression of hormonally-dependent tumors in males or females, or the risk of secondary malignancy, such as breast cancer, is not known. One case-control study of women with ovarian cancer demonstrated higher serum androstenedione and DHEA/DHEAS levels in patients with ovarian tumors versus controls.[22] Whether DHEA supplementation would be associated with similar the serum hormonal profiles is unknown. Male breast cancer, prostate cancer and prostatic hypertrophy can develop due to endocrine epithelial cell growth during therapy with androgens. One case report has been published of a patient with advanced prostate cancer who was symptomatically treated with DHEA. The patient experienced a “flare” of his cancer during the treatment period.[23] A causal relationship has not been established. Widespread use of DHEA supplements in men or women should be discouraged until more is known about potential secondary malignancy risks.
Prasterone, dehydroepiandrosterone (DHEA) is an androgenic hormone and may potentially cause teratogenesis or changes the ability to conceive or carry a viable pregnancy. Dehydroepiandrosterone, DHEA should be considered contraindicated in pregnancy, similar to other androgenic hormones. It is assumed that exogenous DHEA supplementation to a pregnant woman could potentially have deleterious effects on fetal development or viability. No controlled trials of DHEA in primate or human gestation exist. If pregnancy is suspected, pregnancy should be ruled out before continuing DHEA use.
DHEA should be considered a pregnancy category X drug, similar to other androgenic hormones. Studies of the role of endogenous fetal and maternal DHEA in pregnancy indicate that the ratio of DHEA or DHEAS to other hormones in the serum or placenta may influence the processes of fetal development, parturition, and labor. Endogenous DHEA and DHEAS appear to be important in the functional development of the adrenal cortex and other endocrine activities in the fetus; it is assumed that exogenous DHEA supplementation to a pregnant woman could potentially have deleterious effects on fetal development or viability. The androgenic effects of DHEA could potentially result in masculinization of a female fetus. No controlled trials of DHEA in primate or human gestation exist. Do not administer DHEA to a pregnant woman.
DHEA is a hormone and should not be supplemented in a lactating woman who is breastfeeding her infant. Most hormones are excreted in breast milk. Like other androgenic hormones, it is possible that DHEA could inhibit lactation. It is unknown what effect DHEA would have on the breast-feeding infant.
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond use date. Do not flush unused medications or pour down a sink or drain.
- Kroboth PD, Slalek FS, Pittenger AL et al. DHEA and DHEA-S: a review. J Clin Pharmacol 1999;39:327-348.
- Skolnick AA. Medical news and perspectives-scientific verdict still out on DHEA. JAMA 1996;276:1365-1367.
- Kreider RB. Dietary supplements and the promotion of muscle growth with resistance exercise. Sports Med 1999;27:97-110.
- Araneo BA, Ryu SY, Barton S, et al. Dehydroepiandrosterone reduces progressive dermal ischemia caused by thermal injury. J Surg Res 1995;59:250-262.
- Jesse Rl, Loesser K, Eich DM, et al. Dehydroepiandrosterone inhibits human platelet aggregation in vitro and in vivo. Ann N Y Acad Sci 1995;774:281-290.
- 25801
- Katz S, Morales AJ. Dehydroepiandrosterone (DHEA) and DHEA-sulfate (DS) as therapeutic options in menopause. Semin Reprod Endocrinol 1998;16:161-170.
- Rosenfield RL. Ovarian and adrenal function in polycystic ovary syndrome. Endocrinol Metab Clin North Am 1999;28:265-293.
- Wellman M, Shane-McWhorter L, Orlando PL et al. The role of dehydroepiandrosterone in diabetes mellitus. Pharmacotherapy 1999;19:582-591.
- Centurelli MA, Abate MA. The role of dehydroepiandrosterone in AIDS. Ann Pharmacother 1997;31:639-642.
- Kroboth PD, Slalek FS, Pittenger AL et al. DHEA and DHEA-S: a review. J Clin Pharmacol 1999;39:327-48.
- Robbers JE, Tyler VE. Tyler’s Herbs of Choice: the Therapeutic Use of Phytomedicinals. Binghamton NY: Haworth Herbal Press, Inc.; 1999.
- German Commission E. Saw Palmetto berry, Sabal fructus, monograph Published March 2, 1989 and revised January 17, 1991. In: Blumenthal, M et al ., eds. The complete German Commission E Monographs -Therapeutic Guide to Alternative Medicines. Boston MA: Int
- Robinson B, Cutolo M. Should dehydroepiandrosterone replacement therapy be provided with chronic glucocorticoids? Rheumatology 1999;38:488-95.
- Jesse Rl, Loesser K, Eich DM et al. Dehydroepiandrosterone inhibits human platelet aggregation in vitro and in vivo. Ann NY Acad Sci 1995;774:281-90.
- Premarin® (conjugated estrogens, equine) package insert. Philadelphia, PA: Wyeth Pharmaceuticals Inc.; 2003 Jul.
- Wellman M, Shane-McWhorter L, Orlando PL et al. The role of dehydroepiandrosterone in diabetes mellitus. Pharmacotherapy 1999;19:582-91.
- Frye RF, Kroboth PD, Folan MM, et al. Effect of DHEA on CYP3A4-mediated metabolism of triazolam (Abstract PI-82). Clin Pharmacol Ther 2000;67:109.
- Androderm® (testosterone transdermal system) package insert. Corona, CA: Watson Pharma, Inc.; 1999 Jan.
- Aldercreutz H, Mazur W. Phyto-estrogens and western diseases. Annals of Medicine 1997;29:95-120.
- VanVollenhoven RF, Engleman EG, McGuire JL. Dehydroepiandrosterone in systemic lupus erythematosus. Arthritis Rheum 1995;38:1826-1831.
- Helzlsouer KJ, Alberg AJ, Gordon GB, et al. Serum gonadotropins and steroid hormones and the development of ovarian cancer. JAMA 1995;274:1926-1930.
- Jones JA, Nguyen A, Straub M, et al. Use of DHEA in a patient with advanced prostate cancer: a case report and a review. Urology 1997;50:784-788.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
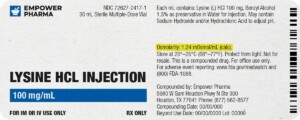
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.



 7-Keto DHEA Capsules
7-Keto DHEA Capsules DHEA / Pregnenolone Capsules
DHEA / Pregnenolone Capsules DHEA Troches
DHEA Troches DHEA Cream
DHEA Cream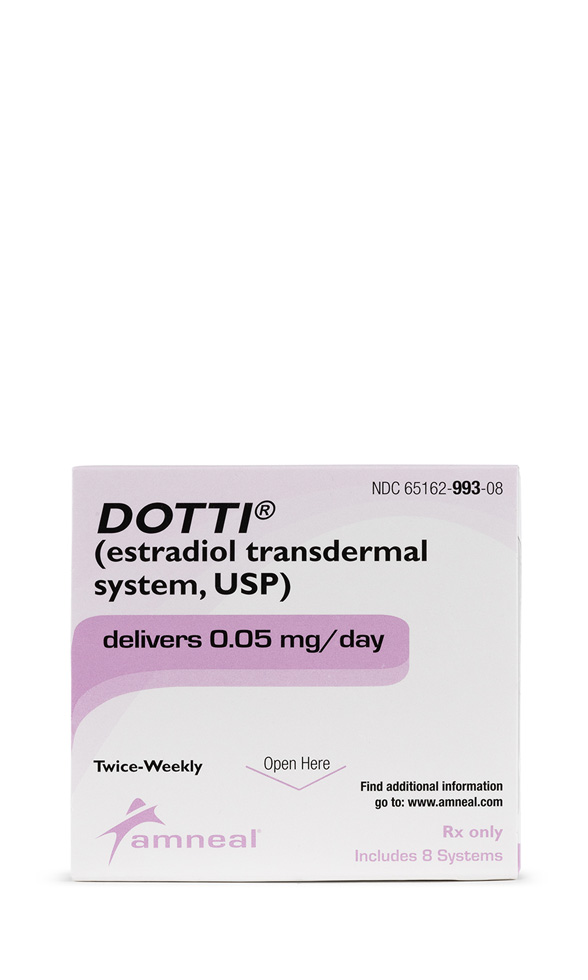 Estradiol Patch
Estradiol Patch Testosterone Cream
Testosterone Cream Testosterone Cypionate Injection
Testosterone Cypionate Injection Progesterone Injection
Progesterone Injection Testosterone Vaginal Cream
Testosterone Vaginal Cream Progesterone Cream
Progesterone Cream