Product Overview
Biotin
Biotin (vitamin H; coenzyme R; classified as a B vitamin) is a dietary component that is important for the metabolism of carbohydrates, fats, and amino acids. It is found primarily in liver, kidney, and muscle. Biotin functions as an essential cofactor for five carboxylases that catalyze steps in fatty acid, glucose, and amino acid metabolism. It is also an important factor in histone modifications, gene regulation, and cell signaling. Mammals must consume biotin to replenish stores. Sources of biotin include organ meats, eggs, fish, seeds, and nuts. As a dietary supplement, biotin has been promoted to be useful in the treatment of hair and nail problems, cradle cap (seborrheic dermatitis) in phenylketonuria patients, biotinidase deficiency, diabetes, peripheral neuropathy, candida infections, and high cholesterol. It has also been used in pregnancy, hemodialysis, and peritoneal dialysis, as biotin deficiency is more likely in these situations. Biotin is found in many cosmetics products. Radiolabeled biotin is used for pretargeted radioimmunotherapy of cancerous tumors.[1]
Minoxidil
Oral minoxidil (Loniten) is an antihypertensive agent; topical minoxidil (Rogaine) is used for alopecia. Topical minoxidil is likely effective in producing moderate hair growth in approximately 30% of men and 60% of women with common hereditary hair loss.[2] Lesser growth or a halt in the worsening of alopecia are also frequent outcomes.[3] Due to its potency and adverse reactions, oral minoxidil is used mainly for patients with severe, drug-resistant forms of hypertension. Tolerance to prolonged therapy with oral minoxidil does not appear to be a problem. Although the oral dosage form was originally approved in October 1979 for use in hypertension, minoxidil was first discovered in 1965. In August 1988 the topical formulation was approved for of alopecia. After declining Upjohn permission to market topical minoxidil as a non-prescription drug in July 1994, the 2% topical solution was subsequently approved for over-the-counter use in men with alopecia in February 1996. In September 1996, Pharmacia and Upjohn petitioned the FDA to increase the topical solution formulation from 2% to 5%; the higher-strength solution has been shown to elicit a more rapid hair growth response (8 weeks vs. 16 weeks) and to regrow an average of 45% more hair than Rogaine Regular Strength.[3] The 5% topical solution (Rogaine Extra Strength) for common hereditary hair loss was approved FDA in November 1997. Approval to market 2% topical solution to women was granted October 1996. Minoxidil foam (Men’s Rogaine Foam) was approved for men in January 2006; potential advantages over the solution formulation include the absence of propylene glycol (potential irritant), ability to limit spread of medication, and less time to dry after application.[4]
Spironolactone
Spironolactone is a potassium-sparing diuretic. In patients with severe heart failure (NYHA Class IV), spironolactone has been shown to improve overall survival and NYHA functional class, and to reduce hospitalizations when added to conventional therapy (e.g., ACE inhibitor, loop diuretic, digoxin).[5] It is frequently used to treat ascites associated with cirrhosis and also has been used as a diagnostic aid for primary hyperaldosteronism. It is also used to treat hypokalemia. Compared to thiazide or loop diuretics, it is a relatively weak agent for treating hypertension or generalized edema, although its effects can be additive with thiazide diuretics. While not FDA-approved indications, acne vulgaris, polycystic ovary syndrome, and female hirsutism have been treated with spironolactone. Spironolactone was approved by the FDA in 1960.
Biotin
Biotin is a water-soluble B vitamin found naturally in some foods and used as a dietary supplement. It is important for the metabolism of carbohydrates, fats, and amino acids. It is found primarily in liver, kidney, and muscle. Biotin functions as an essential cofactor for five carboxylases that catalyze steps in fatty acid, glucose, and amino acid metabolism. It is mostly protein-bound in foods such as organ meats, eggs, nuts, and soybeans. Gastrointestinal enzymes break down ingested biotin via proteolysis. This creates biocytin, which is then cleaved by biotinidase into free biotin and lysine. Free biotin is then absorbed in the small intestine. Biotin can be used for metabolism issues such as biotinidase, holocarboxylase synthetase, and isolated carboxylase enzyme deficiencies due to its essential role in the metabolism of fatty acids, glucose, and amino acids.[1][6]
Minoxidil
Minoxidil has a direct vasodilatory effect on arterial smooth muscle, causing a reduction in peripheral resistance and blood pressure. Minoxidil does not exhibit CNS or adrenergic neuronal blocking effects; minoxidil retains its activity despite adrenergic denervation. Cyclic adenosine monophosphate (cAMP) may contribute to relaxation of vascular smooth muscle. Minoxidil-induced delay in the hydrolysis of cAMP via inhibition of phosphodiesterase may contribute to the drug’s vasodilatory action.
All direct vasodilators produce a sympathetic response including an increase in heart rate, stroke volume, and cardiac output, and a marked increase in plasma renin activity, which, in turn, leads to increased sodium and water retention. This increased renin release is believed to be partially mediated by the beta-adrenergic system. These compensatory responses tend to diminish the hypotensive effects of minoxidil. Additional therapeutic effects can be achieved by using a beta-blocker to offset the predictable sympathetic stimulation caused by minoxidil. Methyldopa may be used if beta-blocker therapy is contraindicated; however, because of its delay in onset, methyldopa must be initiated 24 hours prior to initiating minoxidil. Vasodilator-induced fluid retention is somewhat related to the potency of the vasodilator. Due to its potency, fluid retention occurs routinely with minoxidil. Often, this fluid retention requires concomitant use of loop diuretics (see Adverse Reactions). Triple-drug therapy consisting of a loop diuretic, beta-blocker, and minoxidil produces prompt, sustained reduction in blood pressure in patients with severe hypertension.[7][8]
Minoxidil preferentially dilates arterioles; therefore, postural hypotension may occur during therapy. As an antihypertensive, minoxidil does not lead to improvements in LVH. Minoxidil may actually worsen LVH, potentially due to reflex tachycardia and sympathetic stimulation, which may counteract the benefits of afterload reduction.[9] Minoxidil does not affect glucose tolerance or serum lipids.
The exact mechanism responsible for minoxidil-induced hair growth is not known, but appears to be independent of vasodilation.[10] While systemic therapy will stimulate hair growth, topical therapy usually does not cause hypotension. Current evidence suggests the primary action of topical minoxidil is to decrease the latent period of the hair cycle. The latent period (the time between shedding of telogen hair and the onset of the next anagen) is typically prolonged in male pattern balding; however, this effect has not been demonstrated in balding females.[11] Calcium may also be involved in the process of hair regrowth. In the presence of calcium, epidermal growth factor (EGF) inhibits hair growth. The entry of calcium into a hair cell is opposed by potassium channel openers, such as minoxidil; therefore, EGF-induced inhibition of hair will be opposed by the action of minoxidil, and hair will grow more proficiently. Biopsy specimens have not demonstrated evidence of new follicle formation with the use of minoxidil.[2] Furthermore, minoxidil appears to affect only suboptimal follicles with no further stimulation of normal hair follicles.[10] Minoxidil also may alter the metabolism of androgens in the scalp. Minoxidil increases 17 beta-hydroxylated dehydrogenase activity by almost 40% in dermal papilla cells of a balding scalp, whereas the effect is much less in a nonbalding scalp. Whether this modification in testosterone metabolism of cells of a balding scalp is related to the therapeutic effect of minoxidil is unknown.[12]
Spironolactone
Spironolactone inhibits the effects of aldosterone on the distal renal tubules. Unlike amiloride and triamterene, spironolactone exhibits its diuretic effect only in the presence of aldosterone, and these effects are enhanced in patients with hyperaldosteronism. Aldosterone antagonism enhances sodium, chloride, and water excretion, and reduces the excretion of potassium, ammonium, and phosphate. Spironolactone does not inhibit renal transport mechanisms or carbonic anhydrase activity. In addition, spironolactone acts as an androgen receptor blocker by competitively inhibiting dihydrotestosterone at its receptor sites, and at high doses, spironolactone interferes with steroid synthesis in the adrenal glands and gonads. Sebum excretion rates also are reduced in a dose-dependent manner with spironolactone.
Spironolactone is a poor antihypertensive, but it does have modest hypotensive effects. The hypotensive mechanism of spironolactone is unknown. It is possibly due to the ability of the drug to inhibit aldosterone’s effect on arteriole smooth muscle. Spironolactone also can alter the extracellular-intracellular sodium gradient across the membrane. In general, diuretics lower blood pressure by initially decreasing cardiac output and reducing plasma and extracellular fluid volume. Cardiac output and extracellular fluid volume eventually return to normal, but peripheral resistance is reduced, resulting in lower blood pressure. In general, diuretics worsen glucose tolerance and exert detrimental effects on the lipid profile.
Biotin
Biotin in blood or other samples taken from patients who are ingesting higher biotin dosages (i.e., doses of 10 to 300 mg biotin/day) in dietary supplements, including multivitamins, prenatal vitamins, and supplements for hair, skin, and nail growth, can cause clinically significant incorrect lab test results (falsely high or falsely low results) in assays that use biotin-streptavidin technology. Adverse events, including one death, related to biotin interference with lab tests have been reported.[1][13][14]
Specifically, biotin lab interference has caused falsely low troponin results, which may lead to missed diagnosis and potentially serious clinical implications. One patient taking high levels of biotin died following falsely low troponin test results when a troponin test known to have biotin interference was used. Some lab test developers have been successful at mitigating the biotin interference in their assays, while others may have not addressed this.[1][13][14]
Health care providers should be aware that many lab tests, including but not limited to, cardiovascular diagnostic tests and hormone tests that use biotin technology, may be affected. Discuss dietary supplement intake, particularly those that may contain biotin, with patients and communicate to the lab conducting testing if the patient reports taking biotin-containing supplements.[1][13][14]
Consider laboratory test interference from biotin as a possible source of error if the lab test result does not match the clinical presentation of the patient and report any adverse events thought to be due to biotin interference to the lab test manufacturer and the FDA. One patient reportedly had abnormal thyroid function tests (TFTs) that did not match the clinical context after starting biotin. Within 3 days of stopping supplementation with biotin, repeated TFTs were normal. Then, biotin was reintroduced to the same patient, and TFTs taken 16 hours after the last dose and after an overnight fast showed further evidence of biotin immunoassay interference.[1][13][14]
Biotin during pregnancy at the recommended adequate intake (AI) is recommended. Supplementation outside of dietary intake is usually not necessary if a healthy diet is consumed and no deficiency has been diagnosed.[6]
Breastfeeding females may consume biotin within the recommended adequate intake (AI) parameters. Supplementation outside of dietary intake is usually not necessary if a healthy diet is consumed and no deficiency has been diagnosed.[6]
Minoxidil
Minoxidil has been reported to produce cardiac lesions in animals. Some lesions are characteristic of other drugs that can cause tachycardia and/or hypotension (e.g., isoproterenol, hydralazine). These effects are more likely to occur in patients with compromised renal function and in patients with connective tissue disease, uremic syndrome, CHF, or minoxidil-induced fluid retention.
Systemic minoxidil is a potent vasodilator with potential to produce hypotension and reflex tachycardia; serious complications may occur. Minoxidil is relatively contraindicated in patients with cardiac disease (including angina, coronary artery disease, recent or acute myocardial infarction), or cerebrovascular disease because a reflex increase in heart rate and decrease in blood pressure can exacerbate these conditions.
Minoxidil is relatively contraindicated in patients with coronary insufficiency, including angina, to avoid the risk of reflex tachycardia and angina exacerbation. Minoxidil may cause pericardial effusion which occasionally may progress to cardiac tamponade. Reserve oral minoxidil for hypertension in patients who do not respond adequately to maximum therapeutic doses of a diuretic (loop diuretic suggested) concurrently with 2 other antihypertensive agents.
In experimental animals, minoxidil has been shown to induce several types of myocardial lesions as well as other adverse cardiac effects. Minoxidil must be administered under close supervision, usually in combination with therapeutic doses of a beta-blocker to prevent reflex tachycardia and increased myocardial workload. Minoxidil is often given with a diuretic (preferably a diuretic which acts within the ascending limb of the loop of Henle) to prevent fluid accumulation and peripheral edema.
When first administering minoxidil to patients with malignant hypertension and those already receiving guanethidine to avoid rapid or large orthostatic reductions in blood pressure, minoxidil use requires a specialized care setting, specifically hospitalization. Although minoxidil does not directly cause orthostatic hypotension, administration to patients receiving guanethidine can result in profound orthostatic effects.
When possible, guanethidine should be discontinued well before minoxidil is initiated. Otherwise, minoxidil therapy should be started in the hospital; the patient should remain hospitalized until the risk of excessive orthostatic effects is minimized and the patient is able to avoid activities that induce orthostatic hypotension.
Minoxidil is relatively contraindicated in patients with renal disease, preexisting pulmonary hypertension, or chronic congestive heart failure not secondary to hypertension because the drug can cause an increase in pulmonary artery pressure, which could be detrimental to these patients. Use of minoxidil has been associated with the development of pericardial effusion and tamponade in some patients, and it may be more likely to occur in patients with renal disease. Since approximately only 10% of active drug is eliminated unchanged via the kidneys, minoxidil can be used safely in patients with renal impairment. Renal elimination, however, may be reduced and dosage adjustment may be necessary. Avoid use of minoxidil in patients with severe renal failure (CrCl < 10 ml/min).
Minoxidil is contraindicated in patients with pheochromocytoma because the hypotensive effects of the drug can stimulate catecholamine secretion.
Systemic effects resulting from topically administered minoxidil are unlikely but theoretically could occur if the drug is overused. Skin abrasion or irritations, such as excoriations, psoriasis, or sunburn, can increase the systemic absorption of topically administered minoxidil.
Reported clinical experience has not identified differences in responses in geriatric adults vs. younger adult patients. In general, systemic dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.[15]
Topical minoxidil use carries no special precaution in the elderly, but any patient experiencing dizziness or faintness should discontinue topical use.[2]
The federal Omnibus Budget Reconciliation Act (OBRA) regulates medication use in residents of long-term care facilities (LTCFs). According to OBRA, antihypertensive regimens should be individualized to achieve the desired outcome while minimizing adverse effects. Antihypertensives may cause dizziness, postural hypotension, fatigue, and there is an increased risk for falls. There are many drug interactions that can potentiate the effects of antihypertensives. Some agents require a gradual taper to avoid adverse consequences caused by abrupt discontinuation.[16]
Spironolactone
Spironolactone is contraindicated in patients with hyperkalemia, Addison’s disease (chronic adrenal insufficiency), or other conditions associated with hyperkalemia and should not be administered to those who are receiving other potassium-sparing agents.[17][18] The Endocrine Society guidelines on the diagnosis and treatment of primary adrenal insufficiency state that use of aldosterone antagonists, such as spironolactone, are contraindicated in patients with adrenal insufficiency (Addison’s disease).
Hyperkalemia stimulates aldosterone production and aldosterone, in turn, enhances sodium and water reabsorption in exchange for potassium excretion in the distal tubule and collecting duct of the kidney. In Addison’s disease, aldosterone deficiency results in hyponatremia, hypovolemia, hypotension and hyperkalemia. Thus, spironolactone therapy will exacerbate the hyponatremia, hypovolemia, hypotension and hyperkalemia seen in adrenal insufficiency and worsen the signs and symptoms of the disease.[19][20][21]
Spironolactone-induced hyperkalemia can cause life-threatening cardiac arrhythmias, and it is more likely to occur in patients with impaired renal function or diabetes mellitus. Excessive diuresis may cause symptomatic dehydration, hypotension, and worsening renal function. Spironolactone tablets are contraindicated in patients with anuria or any renal disease associated with severe renal impairment (CrCl less than 10 mL/minute) or acute renal failure.
Monitor serum potassium and renal function 3 days and 1 week after initiation or dosage increase, monthly for 3 months, quarterly for a year, and every 6 months thereafter. Monitor volume status periodically. Patients receiving spironolactone should not receive potassium supplementation or increase their dietary intake of potassium unless they have refractory hypokalemia.
In adults, the risk of hyperkalemia increases progressively when serum creatinine exceeds 1.6 mg/dL; the threshold for pediatric patients is unknown. In adults, spironolactone should be discontinued if the serum creatinine is greater than 4 mg/dL or serum potassium is greater than 5 mEq/L. Spironolactone may cause a transient elevation of BUN, especially in patients with preexisting renal impairment.
The precaution for spironolactone in patients with diabetes mellitus is primarily due to the risk of hyperkalemia and not the risk of inducing hyperglycemia, which may occur with thiazide or loop diuretics.[17][18][22]
Correct significant acid/base imbalance before spironolactone is initiated, as mild acidosis or hypochloremic metabolic alkalosis may occur with its use.[17] Close monitoring of the acid-base status is required in debilitated patients or severely ill patients in whom respiratory acidosis or metabolic acidosis may occur (e.g., cardiopulmonary disease or uncontrolled diabetes). These patients are at a higher risk for developing sudden metabolic acidosis or respiratory acidosis, with resultant rapid increases in serum potassium concentrations that could be exacerbated by potassium-sparing diuretic therapy.
Spironolactone-induced fluctuations in serum electrolyte concentrations can occur rapidly and precipitate hepatic encephalopathy and hepatic coma in patients with hepatic disease with biliary cirrhosis and ascites. In these patients, initiate spironolactone in the hospital. Clearance of spironolactone and its metabolites is reduced in patients with cirrhosis; start with the lowest initial dose and titrate slowly in these patients.[18] Reversible hyperchloremic metabolic acidosis, usually in association with hyperkalemia, has been reported in patients with decompensated hepatic cirrhosis, even with normal renal function.[17]
Spironolactone can cause antiandrogenic and endocrine effects; use with caution in patients with menstrual irregularity or breast enlargement.[17]
Spironolactone has been demonstrated to be tumorigenic in chronic toxicity studies in rats. Although human data are not available, the potential for tumorigenicity or development of a new primary malignancy are potential risks to consider during spironolactone therapy. FDA-approved labeling for the tablet product recommends that spironolactone only be used as indicated within the prescribing information; avoid unnecessary use.[17]
Use spironolactone with caution in patients with prostate cancer. In addition to being an aldosterone antagonist, it has been shown to have some antiandrogenic activity. However, in vitro and in animal studies have confirmed that spironolactone is only a weak and partial androgen antagonist, and has intrinsic androgenic activity.[23][24][25][26] One case report has been published regarding a patient with progression of heavily pretreated castration-refractory prostate cancer (CRPC) after the addition of spironolactone for heart failure to abiraterone therapy; this patient’s PSA returned to its previous level 2 weeks after discontinuation of spironolactone.[27] In another case, a patient with progressive metastatic CRPC on abiraterone and subsequent enzalutamide therapy twice had significant decreases in PSA and stabilization of visceral disease after discontinuation of spironolactone.[28]
Somnolence and dizziness have been reported to occur in some patients. Therefore, caution is advised when driving or operating machinery until the response to treatment with spironolactone has been determined.[17]
Periodic assessment of renal function, along with monitoring of serum electrolytes to detect possible electrolyte imbalances, especially hyperkalemia, should be done at appropriate intervals during spironolactone therapy, particularly in the geriatric patient.[17] According to the Beers Criteria, diuretics are considered potentially inappropriate medications (PIMs) in geriatric patients; use with caution due to the potential for causing or exacerbating SIADH or hyponatremia. Sodium levels should be closely monitored when starting or changing dosages of diuretics in older adults. The Beers expert panel recommends avoiding spironolactone in geriatric patients with a creatinine clearance less than 30 mL/minute due to the potential for increased serum potassium.[29] The federal Omnibus Budget Reconciliation Act (OBRA) regulates medication use in residents of long-term care facilities; antihypertensive regimens should be individualized to achieve the desired outcome while minimizing adverse effects. Antihypertensives may cause dizziness, postural hypotension, fatigue, and there is an increased risk for falls. Diuretics may cause fluid and electrolyte imbalances and may precipitate or exacerbate urinary incontinence.[16]
Avoid spironolactone in pregnancy or advise pregnant women of the potential risk to a male fetus. Because of its anti-androgenic activity and the requirement of testosterone for male morphogenesis, spironolactone may have the potential for adversely affecting sex differentiation of the male during embryogenesis. Animal studies report feminization of male fetuses and endocrine dysfunction in females exposed to spironolactone in utero. Animal offspring exposed to spironolactone during late pregnancy exhibited changes in the reproductive tract, including dose-dependent decreases in weights of the ventral prostate and seminal vesicle in males, ovaries and uteri that were enlarged in females, and other indications of endocrine dysfunction that persisted into adulthood. Limited data from published case reports and case series did not demonstrate an association between major malformations or other adverse pregnancy outcomes with spironolactone use.[18]
Spironolactone is not present in breast-milk; however, canrenone, the major metabolite of spironolactone, does appear in breast-milk in low amounts that are not expected to be clinically relevant. Data from a breast-feeding woman at 17 days postpartum did not indicate any adverse effects on the breast-fed infant; long term effects on a breast-fed infant are unknown. There are no data on the effects of spironolactone on milk production. Consider the developmental and health benefits of breast-feeding along with the mother’s clinical need for spironolactone and any potential adverse effects on the breast-fed child from spironolactone or from the underlying maternal condition.[18] Previous American Academy of Pediatrics recommendations classified spironolactone as usually compatible with breast-feeding.[30]
In animal studies involving female rats, spironolactone was associated with a reduction in circulating estrogen levels and retarded ovarian follicle development. Inhibition of ovulation and reduction in number of implanted embryos were observed with spironolactone administration to female mice. The potential for infertility in humans is unknown.[17]
Biotin
Biotin has been very rarely associated with any adverse effects, even with high doses. There is one case report of life-threatening eosinophilic pleuro-pericardial effusion in an elderly woman who took a combination of 10 mg/day of biotin and 300 mg/day of pantothenic acid for two months.[6]
Minoxidil
The adverse reaction profile for minoxidil depends upon its use. Systemic adverse reactions are unlikely from topical administration. Placebo-controlled trials with topical minoxidil only showed an increase in dermatological effects from the active drug.
Minoxidil is a peripheral vasodilator. All direct vasodilators produce a marked increase in plasma renin activity, which leads to water and sodium retention and sometimes congestive heart failure. This renin release is believed to be partially mediated by the beta-adrenergic system. The degree of fluid retention is somewhat related to the potency of the vasodilator. Due to its potency, fluid retention (edema) occurs routinely with oral minoxidil and usually requires concomitant administration of a loop diuretic. Without a diuretic, rapid fluid retention can occur within a few days of minoxidil therapy. Temporary edema occurred in 7% of patients who were not edematous when minoxidil was initiated.[15] Ascites also has been reported. A restricted dietary intake of sodium can minimize fluid retention and resultant peripheral edema. Rarely, fluid retention is refractory to diuresis and discontinuation of minoxidil is required. Vasodilation may also produce headache.
Minoxidil causes reflex tachycardia; sinus tachycardia may occur. Angina may become apparent, or worsen, secondary to increased myocardial oxygen demand associated with tachycardia and increased cardiac output. Tachycardia and subsequent angina usually can be prevented with the coadministration of a beta-blocker or other sympathetic nervous system suppressant.[15]
Minoxidil has been shown to transiently lower hematocrit, hemoglobin, and erythrocyte count by approximately 7%. Serum creatinine and BUN also have been shown to increase an average of 6% in patients on minoxidil therapy. Increases in alkaline phosphatase, without other evidence of hepatic abnormality, also has been reported. During the course of therapy, these laboratory abnormalities have been shown to return to pretreatment values. Thrombocytopenia and leukopenia also have been reported.[15]
Hypertrichosis (elongation, thickening, and enhancement of fine body hair), without evidence of virilism or endocrine abnormalities, is an embarrassing adverse effect that often occurs with oral minoxidil. This effect is usually evident within 3-6 weeks of therapy and occurs on the temples, between the eyebrows, or in the sideburn area. Hair growth also can appear on the arms, legs, and scalp. It is reversible following discontinuation of the drug.[15]
Oral minoxidil has occasionally been associated with appearance of a bullous rash and Stevens-Johnson syndrome. Topical minoxidil therapy produces local dermatological reactions including contact dermatitis, local burning, pruritus, erythema, or xerosis. Many other adverse effects have been reported during administration of topical minoxidil preparations, but none has been directly attributed to the drug.[15]
Gastrointestinal adverse effects associated with orally administered minoxidil include nausea and vomiting.[15]
Spironolactone
Spironolactone causes hyperkalemia and can cause life-threatening cardiac arrhythmias. Signs and symptoms of hyperkalemia include muscle weakness, paresthesias, fatigue, flaccid paralysis of the extremities, sinus bradycardia, shock, and electrocardiogram (ECG) changes. Patients who receive potassium supplements or patients with impaired renal function who are also receiving spironolactone therapy are particularly at risk for developing hyperkalemia. Monitor serum potassium and renal function 3 days and 1 week after initiation of therapy or dose increase, monthly for 3 months, quarterly for a year, and every 6 months thereafter. If hyperkalemia occurs, decrease the dose or discontinue spironolactone. In adults, spironolactone should be discontinued if serum creatinine is greater than 4 mg/dL or serum potassium is greater than 5 mEq/L; pediatric-specific recommendations are not available. In cases of severe hyperkalemia, urgent measures such as the administration of intravenous calcium, sodium bicarbonate, glucose, and a rapid-acting insulin may be necessary; persistent hyperkalemia may require dialysis.[17][18][22]
Spironolactone can cause hyponatremia, hypomagnesemia, hypocalcemia, hypochloremic metabolic alkalosis, and hyperglycemia. Asymptomatic hyperuricemia can also occur; rarely, gout is precipitated. Monitor serum electrolytes, uric acid, and blood glucose periodically. Electrolyte abnormalities other than hyperkalemia may be more likely when spironolactone is used in combination with other diuretic therapy. Dilutional hyponatremia, which can present as dry mouth, thirst, lethargy, and drowsiness, may also occur in edematous patients during hot weather; appropriate therapy includes water restriction rather than sodium administration except in rare cases of life-threatening hyponatremia.[17][18]
A reversible hyperchloremic metabolic acidosis can occur in patients with decompensated hepatic cirrhosis who are receiving spironolactone. This effect is usually associated with hyperkalemia and can occur regardless of renal function.[17]
Spironolactone is similar in structure to steroid compounds and can produce some of the same adverse effects. In males, spironolactone may cause gynecomastia; this effect is usually dose-related with an onset that varies widely from 1 to 2 months to over a year. Gynecomastia is usually reversible. Impotence (erectile dysfunction) has been reported in with spironolactone therapy. Females taking spironolactone may experience menstrual irregularity, including postmenopausal bleeding, breast tenderness or mastalgia, hirsutism, deepened voice, and amenorrhea. Such endocrine effects may produce a medication-induced infertility. These effects usually are reversible after discontinuance of therapy. Libido decrease has also been reported with spironolactone.[17][18]
While a cause-and-effect relationship has not been established for development of a new primary malignancy, breast cancer has been reported in adults receiving spironolactone. In addition, the tablet product label carries a boxed warning stating that spironolactone is a tumorigen in rats. However, human data are not available to describe the potential for tumorigenicity secondary to use.[17]
Adverse GI effects reported during spironolactone therapy include nausea, vomiting, cramping, diarrhea, gastritis, abdominal pain, gastric bleeding, and ulceration.[17]
Adverse nervous system effects that have been reported in patients receiving spironolactone therapy include headache, dizziness, drowsiness, lethargy, ataxia, and mental confusion. Muscular weakness may be a sign of drug-induced hyperkalemia.[17]
Excessive diuresis may cause symptomatic dehydration, hypovolemia, hypotension, and worsening renal function including renal failure (unspecified). Transient increases in BUN may occur during spironolactone therapy, especially in patients with renal impairment. Monitor volume status and renal function periodically.[17][18] In addition, due to the diuretic action of spironolactone, polyuria can be troublesome for some patients during therapy.
Hypersensitivity reactions such as fever, urticaria, erythema, maculopapular rash, erythematous cutaneous eruptions, vasculitis, and anaphylactoid reactions may occur during therapy with spironolactone. Stevens-Johnson syndrome, toxic epidermal necrolysis, Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), alopecia, chloasma, and pruritus have also been reported with spironolactone therapy.[17][18]
Leukopenia, including agranulocytosis, and thrombocytopenia have been reported during spironolactone therapy.[17]
A few cases of mixed cholestatic/hepatocellular toxicity, including one report of hepatic failure resulting in death, have been reported with spironolactone administration.[17]
Muscle cramps (leg cramps) have been reported in patients taking spironolactone.[17]
Biotin
Biotin during pregnancy at the recommended adequate intake (AI) is recommended. Supplementation outside of dietary intake is usually not necessary if a healthy diet is consumed and no deficiency has been diagnosed.[6]
Minoxidil
Minoxidil is classified as pregnancy risk category C. Although no adequate human studies have examined the effects of this drug on the fetus, animal reproduction studies have shown adverse effects, including reduced ability to conceive and a reduced survival of offspring. Dysmorphic facial features and hypertrichosis were observed in an infant whose mother received a daily minoxidil dosage of 10 mg during pregnancy.[31] Therefore, in making the decision to administer this drug during pregnancy, the potential risks to the fetus and possible difficulty in conceiving must be weighed against the potential benefits to the mother.[32]
Spironolactone
Avoid spironolactone in pregnancy or advise pregnant women of the potential risk to a male fetus. Because of its anti-androgenic activity and the requirement of testosterone for male morphogenesis, spironolactone may have the potential for adversely affecting sex differentiation of the male during embryogenesis. Animal studies report feminization of male fetuses and endocrine dysfunction in females exposed to spironolactone in utero. Animal offspring exposed to spironolactone during late pregnancy exhibited changes in the reproductive tract, including dose-dependent decreases in weights of the ventral prostate and seminal vesicle in males, ovaries and uteri that were enlarged in females, and other indications of endocrine dysfunction that persisted into adulthood. Limited data from published case reports and case series did not demonstrate an association between major malformations or other adverse pregnancy outcomes with spironolactone use.[18]
Biotin
Breastfeeding females may consume biotin within the recommended adequate intake (AI) parameters. Supplementation outside of dietary intake is usually not necessary if a healthy diet is consumed and no deficiency has been diagnosed.[6]
Minoxidil
According to the manufacturer, minoxidil should not be administered to a nursing mother. The American Academy of Pediatrics (AAP) considers minoxidil to be generally compatible with breastfeeding; however, other experts are less comfortable with the use of this potent antihypertensive agent in nursing mothers.[30] In one case report of a woman taking minoxidil 5 mg PO twice daily, minoxidil was rapidly excreted into the breast milk. After two months, no adverse events were reported in the nursing infant. The effect of prolonged exposure during breastfeeding is unknown.[33] Examples of other antihypertensives with more data in this population that have been classified as usually compatible with breastfeeding by the AAP and may be possible alternatives for some patients include enalapril, hydrochlorothiazide, methyldopa, and propranolol.[30] It is not known whether topical minoxidil is distributed into breast milk. Consider the benefits of breastfeeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breastfeeding infant experiences an adverse effect related to a maternally administered drug, healthcare providers are encouraged to report the adverse effect to the FDA.
Spironolactone
Spironolactone is not present in breast milk; however, canrenone, the major metabolite of spironolactone, does appear in breast milk in low amounts that are not expected to be clinically relevant. Data from a breast-feeding woman at 17 days postpartum did not indicate any adverse effects on the breastfed infant; long-term effects on a breastfed infant are unknown. There are no data on the effects of spironolactone on milk production. Consider the developmental and health benefits of breastfeeding along with the mother’s clinical need for spironolactone and any potential adverse effects on the breast-fed child from spironolactone or from the underlying maternal condition.[18] Previous American Academy of Pediatrics recommendations classified spironolactone as usually compatible with breastfeeding.[30]
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond-use date. Do not flush unused medications or pour down a sink or drain.
- Office of Dietary Supplements. Biotin fact sheet for health professionals. September 2018. Internet version, retrieved June 24, 2019. Available on the World Wide Web at: https://ods.od.nih.gov/factsheets/Biotin-HealthProfessional/
- DeVillez RL. The Therapeutic Use of Topical Minoxidil. Dermatol Clin 1990;8:367-74.
- Olsen EA, Dunlap FE, Funicella T, et al. A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. J Am Acad Dermatol 2002;47:377-85.
- Olsen EA, Whiting D, Bergfeld W, et al. A multicenter, randomized, placebo-controlled, double-blind clinical trial of a novel formulation of 5% minoxidil topical foam versus placebo in the treatment of androgenetic alopecia in men. J Am Acad Dermatol 2007;57(5):767-74. Epub 2007 Aug 29
- Pitt B, Zannad F, Remme WJ. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999;341:709-717.
- Standing Committee on the Scientific Evaluation of Dietary Reference Intakes-Panel on Folate, Other B Vitamins, and Choline and the Subcommittee on Upper Reference Levels of Nutrients, Food and Nutrition Board, Institute of Medicine (IOM). Dietary Reference Intakes for Thiamine, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin and Choline. 1999, 2000. The National Academy of Sciences Press, Washington DC.
- Bauer JH, Alpert MA. Rapid reduction of severe hypertension with minoxidil. J Cardiovasc Pharmacol 1980;2 Suppl:S189-99.
- Alpert MA, Bauer JH. Rapid control of severe hypertension with minoxidil. Arch Intern Med 1982;142(12):2099-104.
- Pogatsa-Murray G, Varga L, Varga A, et al. Changes in left ventricular mass during treatment with minoxidil and cilazapril in hypertension patients with left ventricular hypertrophy. J Hum Hypertens 1997;11(3):149-56.
- Buhl AE. Minoxidil’s action in hair follicles. J Invest Dermatol 1991;96:73S-4S.
- Messenger AG, Rundegren J. Minoxidil: mechanisms of action on hair growth. Br J Dermatol 2004;150:186-194.
- Sato T, Tadokoro T, Sonoda T, et al. Minoxidil increases 17b-hydroxysteroid dehydrogenase and 5a-reductase activity of cultured human dermal papilla cells from balding scalp. J Derm Sci 1999;19:123-5.
- US Food and Drug Administration (FDA). FDA Safety Communication: Update: The FDA warns that biotin may interfere with lab tests.
- Elston MS, Sehgal S, Toit SD, et al. Factitious graves’ disease due to biotin immunoassay interference – a case and review of the literature. J Clin Endocrinol Metab 2016;101(9):3251-3255.
- Loniten (minoxidil) tablets package insert. Kalamazoo, MI: Pharmacia; 2006 Feb.
- Health Care Financing Administration. Interpretive Guidelines for Long-term Care Facilities. Title 42 CFR 483.25(l) F329: Unnecessary Drugs. Revised 2015.
- Aldactone (spironolactone) package insert. New York, NY: G.D. Searle LLC Division of Pfizer Inc.; 2020 Jun.
- Carospir (spironolactone) oral suspension package insert. Farmville, NC: CMP Pharma, Inc.;2021 Jun.
- Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and treatment of primary adrenal insufficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:364-389.
- Esposito D, Pasquali D, Johannsson G. Primary adrenal insufficiency: managing mineralocorticoid replacement therapy. J Clin Endocrinol Metab. 2018;103:376-387.
- Inder WJ, Meyer C, Hunt PJ. Management of hypertension and heart failure in patients with Addison’s disease. Clin Endocrinol. 2015;82:789-792.
- Hunt SA, Abraham WT, Chin MH, et al. 2009 Focused Update Incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults. Circulation 2009;119:e391-e479.
- Luthy IA, Begin DJ, Labrie F. Androgenic activity of synthetic progestins and spironolactone in androgen-sensitive mouse mammary carcinoma (Shionogi) cells in culture. J Steroid Biochem. 1988;31(5):845-852.
- Bedussi F, Galli D, Fragni M, et al. Amiloride is effective in the management of abiraterone-induced mineralocorticoid excess syndrome without interfering with its antineoplastic activity. Pharmacology. 2017;100:261-268.
- Richards J, Lim AC, Hay CW, et al. Interactions of abiraterone, eplerenone, and prednisolone with wild-type and mutant androgen receptor: a rationale for increasing abiraterone exposure or combining with MDV3100. Cancer Research. 2012;72(9):2176-2182.
- Barthelemy P, Erdmann E, Duclos B, et al. Spironolactone: a selective androgen receptor modulator in castration-resistant prostate cancer. J Clin Oncol. 2014;32(4 suppl):abstract 212.
- Sundar S and Dickinson PD. Spironolactone, a possible selective androgen receptor modulator, should be used with caution in patients with metastatic carcinoma of the prostate. BMJ Case Reports. 2012;doi:10.1136/bcr.11.2011.5238.
- Flynn T, Guancial EA, Kilari M, and Kilari D. Case report: spironolactone withdrawal associated with a dramatic response in a patient with metastatic castrate-resistant prostate cancer. Clinical Genitourinary Cancer. 2017;15(1):e95-e97.
- The American Geriatrics Society 2019 Beers Criteria Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2019;00:1-21.
- American Academy of Pediatrics (AAP) Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics 2001;108(3):776-789.
- Kaler SG, Patrinos ME, Lambert GH, et al. Hypertrichosis and congenital anomalies associated with maternal use of minoxidil. Pediatrics 1987;79:434-6.
- Minoxidil tablets package insert. Corona, CA: Watson Laboratories, Inc; 2009 Jun.
- Valdivieso A, Valdes G, Spiro TE, et al. Minoxidil in breast milk. Ann Intern Med. 1985;102:135. Letter.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.



 Biotin / Minoxidil Capsules
Biotin / Minoxidil Capsules Hair Restore Ultra Scalp Solution
Hair Restore Ultra Scalp Solution Hair Restore D Scalp Solution
Hair Restore D Scalp Solution GHK-Cu Scalp Solution
GHK-Cu Scalp Solution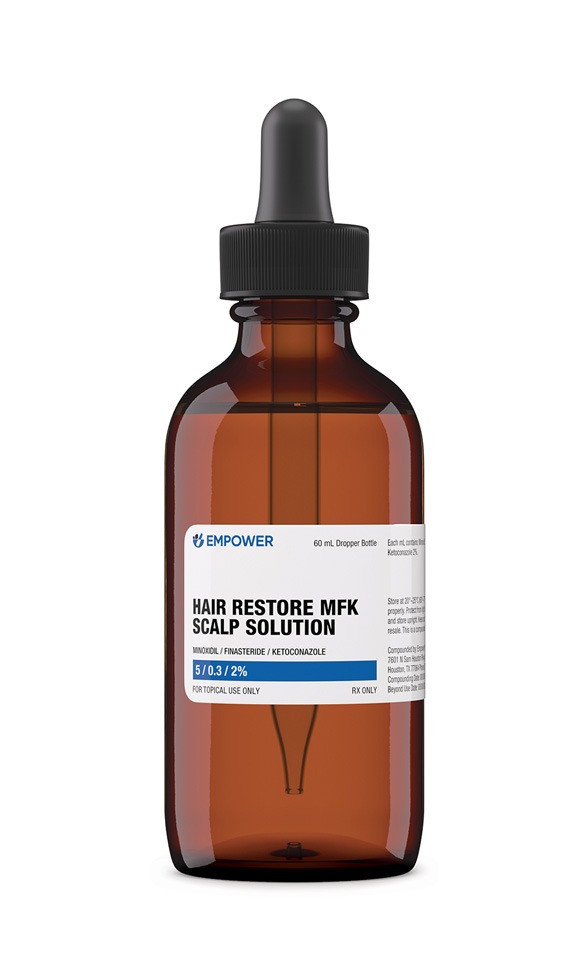 Hair Restore MFK Scalp Solution
Hair Restore MFK Scalp Solution NAD+ Nasal Spray
NAD+ Nasal Spray