Product Overview
Anti-Aging Ultra Cream is a compounded, prescription-only dermatologic preparation designed to address multiple biochemical pathways implicated in cutaneous aging. Each 30-gram cream delivers a precisely balanced concentration of five active ingredients-10 % ascorbic acid, 5 % azelaic acid, 1 % alpha-lipoic acid, 0.1 % estriol, and 2 % progesterone-within an anhydrous base optimized for dermal penetration. Topical ascorbic acid has demonstrated clinically significant improvement in photodamaged skin texture and collagen architecture when compared with placebo, validating its role as the keystone antioxidant in the formulation.[1] Estriol, a weaker estrogen with predominantly cutaneous activity, has separately been shown to improve elasticity and diminish wrinkle depth in perimenopausal women, supporting its inclusion as a hormonal rejuvenant.[2]
Beyond single-agent effects, the cream leverages synergistic mechanisms. Azelaic acid contributes antimicrobial and anti-inflammatory benefits that complement the free-radical scavenging of ascorbic acid while alpha-lipoic acid enhances intracellular recycling of oxidized antioxidants, sustaining redox balance and supporting extracellular matrix integrity.[3][4] These combined actions aim to mitigate intrinsic collagen degradation, uneven pigmentation, and barrier dysfunction common to aging skin.
The vehicle is compounded exclusively in a 503A pharmacy, permitting patient-specific customization under a physician’s order and adherence to USP <795> and <800> guidelines. Because the preparation contains bio-identical sex steroids, counseling emphasizes that systemic absorption, although minimal, may still occur, particularly with prolonged or occlusive use. Patients with hormone-sensitive conditions therefore require individualized risk-benefit assessment and periodic monitoring.[5]
Apply a pea-sized amount to clean, dry facial skin once nightly for the first two weeks, then increase to twice daily as tolerated.[1] Gentle cleansing with a pH-balanced wash is advised prior to application, followed by broad-spectrum sunscreen each morning to prevent photosensitivity and oxidation.
Physicians may tailor concentration ratios or reduce frequency for those with sensitive skin or concurrent acne therapies. Because compounded creams lack FDA-standardized stability data, refills should be prepared every 60-90 days to ensure potency, and patients instructed to note any color changes indicating oxidation.[5]
Avoid applying immediately before or after exfoliating procedures or laser treatments; a five-day washout minimizes additive irritation.[13] Therapeutic response is typically observed after 8-12 weeks, with maximal benefits at six months; maintenance continues thereafter under clinician direction.[3]
Ascorbic acid functions as a co-factor for prolyl and lysyl hydroxylases, stabilizing the triple helix of newly synthesized collagen and directly neutralizing reactive oxygen species (ROS) generated by ultraviolet radiation. A systematic review confirms its capacity to up-regulate type I and III collagen gene expression while simultaneously inhibiting melanogenesis, accounting for improvements in firmness and dyspigmentation.[6]
Azelaic acid, a dicarboxylic acid produced by Malassezia furfur, competitively inhibits tyrosinase and mitochondrial oxidoreductases, thereby reducing abnormal melanocyte activity and ROS formation. Its documented suppression of neutrophil-derived ROS explains clinical reductions in erythema and papulopustular lesions associated with both acne and rosacea.[3][7] Retinoid-combination studies further indicate additive depigmenting benefits without significant irritation in skin of color, underscoring its versatility in multi-ingredient protocols.[8]
Alpha-lipoic acid is a potent, low-molecular-weight dithiol capable of shuttling between oxidized and reduced states, regenerating vitamins C and E in situ and modulating nuclear factor erythroid-2-related factor 2 (Nrf2) signaling. In skin-on-a-chip models, ALA increased filaggrin and involucrin expression and thickened epidermal equivalents, suggesting barrier normalization.[4] Supplementation studies corroborate enhancements in dermal microcirculation and sensory function, relevant to age-related perfusion decline.[9]
Estriol and progesterone act on estrogen and progesterone receptors within keratinocytes and fibroblasts. Topical estriol up-regulates hyaluronan synthase and type I procollagen while down-regulating matrix metalloproteinase-1, translating to measurable gains in skin turgor and moisture.[10] Progesterone augments dermal elastin content and suppresses inflammatory cytokines, effects observed with a 2 % cream in peri- and postmenopausal cohorts.[5] Together they may restore the hormone-responsive genomic milieu that wanes after midlife.
Use is contraindicated in patients with known hypersensitivity to any component of the formulation or with a history of severe contact dermatitis to topical acids or lipophilic antioxidants. Individuals with active or past estrogen- or progesterone-dependent neoplasms should avoid exposure given the presence of sex steroids.[10][11]
Additional caution is advised in patients receiving systemic CYP3A4-inducing medications-such as certain anticonvulsants or rifampin-which can accelerate progesterone metabolism and alter hormonal balance.[12] Liver dysfunction may further modify steroid clearance, warranting physician oversight.
Concurrent application of strong oxidizers (e.g., benzoyl peroxide) can inactivate ascorbic acid; therefore, co-administration on the same skin site or routine is ill-advised.[13] Active facial dermatoses characterized by barrier disruption, including acute eczema or open lesions, increase the risk of systemic absorption and irritation and should be stabilized before treatment.
Topical vitamin C is readily oxidized by benzoyl peroxide; alternating morning vitamin C and evening peroxide minimizes mutual degradation.[13] Similarly, acidic alpha-hydroxy or beta-hydroxy exfoliants can lower the pH excessively and potentiate irritation, suggesting staggered scheduling or reduced frequency.
Azelaic acid pairs safely with retinoids, and combined regimens improve post-inflammatory hyperpigmentation without heightened irritation, yet simultaneous layering may still provoke transient stinging in sensitive users.[8] Close monitoring during initiation is prudent.
Systemic inducers of CYP3A4 may decrease local progesterone levels, theoretically reducing efficacy and altering systemic hormone ratios; conversely, potent inhibitors could heighten exposure. Although percutaneous absorption is low, clinicians should review medication profiles, particularly in polypharmacy populations.[15]
The most common reactions are mild, transient erythema, tingling, or dryness at the application site, attributable to the acidic pH and keratolytic nature of ascorbic and azelaic acids.[6] Patch testing or gradual titration mitigates early discomfort.
Azelaic acid has been associated with temporary pruritus or burning, described as self-limiting and rarely leading to discontinuation.[3] Alpha-lipoic acid may cause a subtle sulphurous odor on skin but demonstrates an excellent irritation profile in vitro and in vivo.[4]
Hormonal components introduce theoretical risks of systemic effects such as breast tenderness or menstrual irregularity, though randomized trials of 2 % progesterone cream reported no significant endocrine adverse events relative to vehicle and pharmacovigilance databases list few cutaneous events. Nonetheless, unexpected systemic symptoms warrant cessation and evaluation.[5][11]
Sufficient human data are lacking to confirm safety of topical estriol or progesterone during pregnancy; therefore, the preparation is not recommended for pregnant or nursing individuals.[10] Systemic absorption, while minimal, could theoretically influence fetal development or lactation. Patients planning conception should discontinue use and consult obstetric providers.
Azelaic acid is classified as pregnancy category B when used as a monotherapy, yet its co-formulation with hormones introduces additional uncertainty. Alpha-lipoic and ascorbic acids are generally regarded as safe antioxidants, but their inclusion does not offset hormonal considerations. Risk-benefit analysis must prioritize fetal safety over cosmetic benefit.[15]
For postpartum individuals not breastfeeding, therapy may resume once hormone levels normalize and wound integrity is restored, provided no contraindications exist. Clinical reassessment ensures suitability and adjusts expectations given hormonally induced skin changes during pregnancy.[6]
- Humbert, P. G., Haftek, M., Creidi, P., et al. (2003). Topical ascorbic acid on photoaged skin: Clinical, topographical and ultrastructural evaluation-double-blind study vs. placebo. Experimental Dermatology, 12(3), 237-244. https://doi.org/10.1034/j.1600-0625.2003.00008.x
- Schmidt, J. B., Binder, M., Macheiner, W., et al. (1994). Treatment of skin ageing symptoms in perimenopausal females with estrogen compounds: A pilot study. Maturitas, 20(1), 25-30. https://doi.org/10.1016/0378-5122(94)90097-3
- Sauer, N., Oślizło, M., Brzostek, M., et al. (2024). The multiple uses of azelaic acid in dermatology: Mechanism of action, preparations, and potential therapeutic applications. Postępy Dermatologii i Alergologii, 40(6), 716-724. https://doi.org/10.5114/ada.2023.133955
- Kim, K., Kim, J., Kim, H., et al. (2021). Effect of α-lipoic acid on the development of human skin equivalents using a pumpless skin-on-a-chip model. International Journal of Molecular Sciences, 22(4), 2160. https://doi.org/10.3390/ijms22042160
- Holzer, G., Riegler, E., Hönigsmann, H., et al. (2005). Effects and side-effects of 2 % progesterone cream on the skin of peri- and postmenopausal women: Results from a double-blind, vehicle-controlled, randomized study. British Journal of Dermatology, 153(3), 626-634. https://doi.org/10.1111/j.1365-2133.2005.06685.x
- Klimek, P., Bodkhe, R., Łoś-Kaszczyńska, K., et al. (2024). Ascorbic acid treatments as effective and safe anti-aging therapies for sensitive skin. Antioxidants, 13(2), 174. https://doi.org/10.3390/antiox13020174
- Jones, D. A. (2009). Rosacea, reactive oxygen species, and azelaic acid. Journal of Clinical and Aesthetic Dermatology, 2(1), 26-30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2958186/
- Woolery-Lloyd, H. C., Keri, J., & Doig, S. (2013). Retinoids and azelaic acid to treat acne and hyperpigmentation in skin of color. Journal of Drugs in Dermatology, 12(4), 434-437. https://jddonline.com/articles/retinoids-and-azelaic-acid-to-treat-acne-and-hyperpigmentation-in-skin-of-color-S1545961613P0434X
- .de Bengy, A.-F., Decorps, J., Martin, L. S., et al. (2022). Alpha-lipoic acid supplementation restores early age-related sensory and endothelial dysfunction in the skin. Biomedicines, 10(11), 2887. https://doi.org/10.3390/biomedicines10112887
- Schmidt, J. B., Hönigsmann, H., & Bieglmayer, C. (1996). Treatment of skin aging with topical estrogens. Archives of Dermatology, 132(1), 27-31. https://doi.org/10.1001/archderm.1996.03890370033011
- DrugBank. (2025). Progesterone: Uses, interactions, mechanism of action. https://go.drugbank.com/drugs/DB00396
- Dapito, M. M., & Gomez, A. (2013). Isoform-specific regulation of cytochromes P450 expression by estrogens and progesterone. Toxicological Sciences, 135(3), 651-663. https://doi.org/10.1093/toxsci/kft162
- Software. (2022). The dos and don’ts of mixing skincare ingredients. https://www.skin.software/journal/skincare-ingredients-that-dont-mix
- Widjaja, A., Lim, J., & Seo, K. (2021). Clinical comparison of topical 2.5 % benzoyl peroxide plus 5 % niacinamide versus 2.5 % benzoyl peroxide alone for mild to moderate acne. Dermatology Research and Practice, 2021, 8857423. https://doi.org/10.1155/2021/8857423
- Drugs..com. (2025). Drug interaction report: Estrogens/progestins with CYP3A4 inducers. https://www.drugs.com/interactions-check.php
How soon will I see results?
Noticeable improvements in brightness and texture often appear within eight weeks, with continued gains over six months.[1]
Can I use this with retinol?
Yes but apply retinol at night and the cream in the morning or alternate evenings to prevent cumulative irritation.[8]
Is it safe for acne-prone skin?
Azelaic acid offers antimicrobial benefits that may improve mild acne but monitor for purging during the first weeks.[3]
Do I need a prescription?
Yes-because it contains compounded hormones, a licensed prescriber must authorize preparation.[5]
Will it lighten dark spots?
Ascorbic and azelaic acids inhibit melanogenesis, so gradual fading of hyperpigmentation is expected with consistent use.[6][7]
Can men use this cream?
The formulation is not gender-specific; however, individuals with androgen-dependent conditions should discuss hormonal exposure with their clinician.[11]
What if I experience stinging?
Reduce application frequency to every other day and apply a bland moisturizer 10 minutes afterward until tolerance builds.[3]
Is sunscreen still necessary?
Absolutely-antioxidants complement but do not replace ultraviolet protection; daily SPF use prevents re-damage.[6]
Will it affect birth-control efficacy?
No evidence suggests topical hormones interfere with systemic contraceptives, yet concomitant CYP3A4 inducers could alter systemic hormone levels.[12]
Can I apply it around the eyes?
Periorbital use should be cautious due to thinner skin; a patch test at the lateral canthus is recommended first.[5]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Administration Instructions
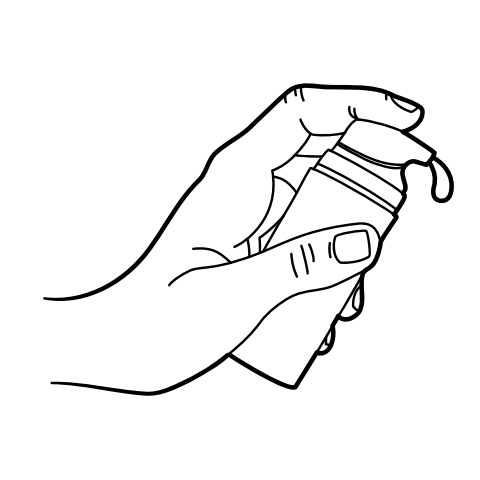
Pump Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Anti-Aging Siro Gel
Anti-Aging Siro Gel Anti-Aging Vita Gel
Anti-Aging Vita Gel Tretinoin TAAN Cream
Tretinoin TAAN Cream GHK-Cu Facial Serum
GHK-Cu Facial Serum Biotin (Vitamin B7) Injection
Biotin (Vitamin B7) Injection NAD+ Cream
NAD+ Cream Sermorelin Acetate Injection
Sermorelin Acetate Injection NAD+ Injection (Lyo)
NAD+ Injection (Lyo)