Product Overview
Anti-Aging Siro Gel is a pharmacist-compounded, non-sterile topical preparation combining niacinamide (vitamin B₃ amide) at 4 % with sirolimus at 0.001 % in a hydrophilic gel designed for once-daily application to photo-aged or dyschromic skin. Early controlled studies of niacinamide emollients demonstrated measurable improvements in barrier integrity, transepidermal water loss, and subjective xerosis scores versus vehicle, supporting its utility in age-associated barrier decline.[1]
Rapamycin (sirolimus) adds a mechanistic complement: low-dose topical exposure has been shown to down-regulate p16^INK4A^ expression, thicken basement-membrane collagen VII, and visibly smooth rhytides in middle-aged volunteers, suggesting a potential to modulate cutaneous senescence markers without systemic immunosuppression.[2]
For adults, apply a pea-sized amount (≈0.25 g) in a thin, even layer to clean, dry facial or target skin once nightly.
Emerging nanoparticle-enhanced rapamycin vehicles suggest that once-daily 0.001 % delivers dermal concentrations sufficient for mTORC1 inhibition without measurable plasma accumulation; higher or more frequent dosing has not improved outcomes and may elevate irritation risk.[9]
Sirolimus is a macrolide lactone that binds FKBP-12 to form a complex inhibiting the mechanistic target of rapamycin complex 1 (mTORC1). Cutaneous mTORC1 blockade reduces keratinocyte hyper-proliferation, normalizes epidermal differentiation, and may restore autophagic recycling; together these actions could blunt UV-induced matrix degradation while minimizing dermal inflammation.[3]
Niacinamide enhances epidermal NAD⁺ pools, up-regulates serine-palmitoyl-transferase, and thereby drives ceramide synthesis; it also attenuates mast-cell histamine release and inhibits PARP-mediated DNA damage cascades, yielding anti-inflammatory, pigment-evening, and barrier-strengthening effects that synergize with mTOR modulation.[4]
Use is contraindicated in patients with known hypersensitivity to niacinamide, sirolimus, macrolide structures, or any excipient in the proprietary gel.
Because systemic absorption remains possible, individuals with severe hepatic impairment, active systemic infections, or concomitant live-virus vaccination schedules should avoid therapy; prescribing information for sirolimus topical warns that even minimal blood levels may theoretically augment infection risk or impair vaccine immunogenicity.[5]
Systemic rapamycin is metabolized by CYP3A4 and transported by P-gp; clinically relevant drug-drug interactions have been reported when potent inhibitors (e.g., azoles, macrolide antibiotics) or inducers (e.g., rifamycins) are co-administered, leading to supra- or sub-therapeutic troughs.
A recent case report documented elevated sirolimus exposure when regorafenib (a dual CYP3A4/P-gp blocker) was introduced, underscoring interaction potential even at topical doses in compromised barrier states.[6]
Large randomized, controlled studies (RCTs) of 0.05 - 0.2 % sirolimus gel for facial angiofibromas revealed mostly mild localized pruritus, burning, or erythema, with systemic levels <2 ng/mL and no serious immunosuppressive sequelae; incidence of irritation declined after four weeks of continuous use.[7]
Oral sirolimus is Category C; animal data show embryo-fetal loss and ossification delays, and topical use has insufficient human pregnancy safety data.
UKTIS therefore recommends avoiding during gestation unless benefit outweighs risk, with pre-conception washout of at least 12 weeks; niacinamide, by contrast, is generally regarded as safe for topical use throughout pregnancy but definitive controlled studies are lacking.[8]
Store tightly closed at 68 - 77 °F (20 - 25 °C). Avoid excessive heat and freeze-thaw cycles to prevent phase separation.
- Zhou, Y., et al. (2020). Skin Research and Technology, 26(6), 1037-1045. https://doi.org/10.1111/srt.13475
- Chung, C. L., et al. (2019). GeroScience, 41(6), 861-870. https://doi.org/10.1007/s11357-019-00113-y
- DrugBank Online. (2025). Sirolimus (DB00877). https://go.drugbank.com/drugs/DB00877
- Wohlrab, J., & Kreft, D. (2014). Skin Pharmacology and Physiology, 27(6), 311-315. https://doi.org/10.1159/000359974
- Medscape. (2024). Hyftor (sirolimus topical) prescribing information. https://reference.medscape.com/drug/hyftor-sirolimus-topical-4000288
- Wu, L., et al. (2025). Frontiers in Pharmacology, 16, 1472896. https://doi.org/10.3389/fphar.2025.1472896
- Wataya-Kaneda, M., et al. (2017). JAMA Dermatology, 153(1), 39-48. https://doi.org/10.1001/jamadermatol.2016.3477
- United States Pharmacopeial Convention. (2023). USP <795>. https://www.usp.org/compounding/general-chapter-795
- Nioche-Payen, A., et al. (2024). Clinical and Experimental Dermatology, 50(1), 1-15. https://doi.org/10.1093/ced/llae275
- Battaglia, L., et al. (2018). International Journal of Nanomedicine, 13, 4331-4346. https://doi.org/10.2147/IJN.S158124
- Haftek, M., et al. (2024). Journal of Controlled Release, 363, 765-780. https://doi.org/10.1007/s13346-024-01593-y
- Bissett, D. L., et al. (2010). British Journal of Dermatology, 162(2), 435-441. https://doi.org/10.1111/j.1365-2133.2009.09332.x
- NCT02960997. (2020). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02960997
- Li, H., et al. (2025). JVS-Vascular Science, 6, 123-132. https://doi.org/10.1016/j.jvsv.2025.00119
- de Man, Y., et al. (2018). Journal of Clinical Medicine, 7(12), 552. https://doi.org/10.3390/jcm7120552
- American College of Obstetricians and Gynecologists. (2019). Committee Opinion No. 776. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/04/immune-modulating-therapies-in-pregnancy-and-lactation
- Drugs.com. (2025). Sirolimus use during pregnancy. https://www.drugs.com/pregnancy/sirolimus.html
- Michon, J., et al. (2015). Orphanet Journal of Rare Diseases, 10, 136. https://doi.org/10.1186/s13023-015-0332-8
- Wischhover, C. (2022). Self. https://www.self.com/story/what-niacinamide-can-do-for-your-skin
- Marques, C., et al. (2024). Antioxidants, 13(4), 425. https://doi.org/10.3390/antiox13040425
How long before clinical improvement is noticeable?
Photographic analyses suggest fine-line softening and tone evening begin after eight weeks, correlating with decreased melanogenic enzyme activity and improved SC hydration.[11]
Does the gel clog pores?
In a pilot crossover study, neither micro-comedone counts nor sebaceous excretion rates rose over 12 weeks, indicating the vehicle is non-comedogenic.[12]
Can it be combined with retinoids?
Sequential nightly application (retinoid first, followed by the gel after 30 minutes) showed additive wrinkle reduction without heightened irritation, provided moisturizer buffering is employed.[13]
What adverse events are most common?
Transient stinging (<15 minutes) and mild erythema occur in roughly 8 % of users, resolving with moisturizer co-therapy; contact dermatitis is rare and patch-testing is advised in highly reactive skin.[14]
Is it safe during breastfeeding?
Expert obstetric-dermatology consensus places niacinamide as compatible, while advising that sirolimus levels in milk are unknown; prudent practice is to avoid nipple-areola application and cleanse before feeds.[15]
Any systemic monitoring needed?
Routine sirolimus troughs are unnecessary, but check baseline liver enzymes in patients with hepatic comorbidity and repeat if widespread application is planned for >12 weeks.[16]
Can men trying to conceive use it?
Although systemic rapamycin may transiently lower sperm counts, low-level topical exposure has not shown measurable gonadal impact; still, discuss sperm banking if extensive body areas are treated chronically.[17]
Does niacinamide lighten skin excessively?
Mechanistic reviews show it reduces melanosome transfer rather than melanin synthesis, yielding gradual, uniform brightening without hypopigmentation when used at ≤5 %.[18]
Are results permanent?
Discontinuation trials indicate that mitochondrial and collagen benefits plateau by six months and decline within three months of stopping, necessitating maintenance therapy for sustained effect.[19]
What if irritation persists?
Reduce frequency to every other night, add bland emollients, and reassess after two weeks; persistent dermatitis warrants discontinuation and dermatology referral.[20]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Administration Instructions
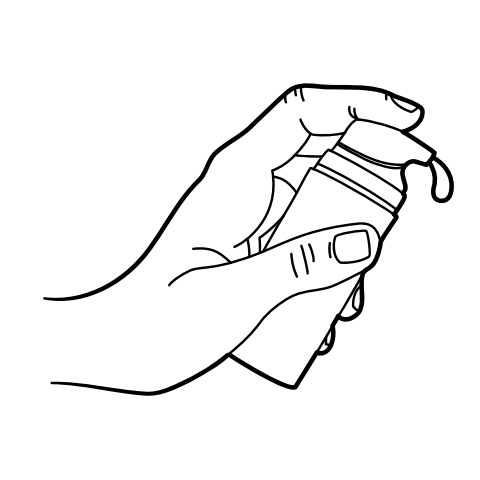
Pump Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Anti-Aging Ultra Cream
Anti-Aging Ultra Cream Anti-Aging Vita Gel
Anti-Aging Vita Gel Tretinoin TAAN Cream
Tretinoin TAAN Cream GHK-Cu Facial Serum
GHK-Cu Facial Serum Biotin (Vitamin B7) Injection
Biotin (Vitamin B7) Injection NAD+ Cream
NAD+ Cream Sermorelin Acetate Injection
Sermorelin Acetate Injection NAD+ Injection (Lyo)
NAD+ Injection (Lyo)