Product Overview
Acne DNS Gel is a pharmacist-compounded, prescription-only topical formulation that combines dapsone 6 %, niacinamide 2 %, and spironolactone 5 % in a fast-drying, cosmetically elegant gel intended for once- or twice-daily application to affected skin.
The preparation was developed to target several pathogenic pathways of acne vulgaris simultaneously-bacterial overgrowth, follicular hyperkeratinization, inflammatory signaling, and androgen-mediated sebogenesis-while minimizing systemic exposure through topical delivery.[1]
The inclusion of dapsone, a synthetic sulfone with both antimicrobial and anti-inflammatory properties, provides a well-documented reduction in inflammatory papules and pustules when used at concentrations between 5 % and 7.5 %.[2] Niacinamide (vitamin B₃ amide) at 2 % augments the formulation by modulating epidermal barrier lipids, down-regulating nuclear factor-κB pathways, and reducing post-inflammatory hyperpigmentation, thereby broadening cosmetic acceptability for diverse skin tones.[3]
Finally, spironolactone at 5 % offers topical antiandrogenic activity that reduces sebaceous lipid production, complementing the antibacterial and anti-inflammatory effects of the other constituents without the electrolyte disturbances sometimes associated with oral hormonal therapies.[4]
Collectively, these mechanisms allow prescribers to address both inflammatory and comedonal lesions in adolescent and adult patients, including those whose acne is flared by endogenous or exogenous hormones.[5]
Current compounding practice favors hydroalcoholic gels for rapid drying, patient acceptability, and accurate dose delivery; the vehicle used for Acne DNS Gel includes volatile solvents that evaporate after spreading, leaving an even film without visible residue or pilling under cosmetics or sunscreens.[6] Comparative studies have shown that multilayer combination products improve adherence compared with separate single-agent prescriptions, particularly in adult women juggling complex regimens.[7]
The 6 % dapsone component yields lesion-count reductions comparable to twice-daily 5 % preparations yet requires only once-daily application, an advantage in individuals with demanding schedules.[8] Niacinamide is titrated at 2 %-a concentration that balances anti-inflammatory efficacy with excellent tolerability, reducing the likelihood of erythema or stinging relative to higher percentages.[9] Spironolactone 5 % gel further differentiates the product by targeting sebaceous activity topically; early trials demonstrated clinically significant sebum suppression and lesion-count improvements without detectable systemic aldosterone antagonism.[10]
Because Acne DNS Gel is dispensed exclusively by a 503A compounding pharmacy, it is tailored for individual prescriptions written by licensed clinicians; the formulation is prepared in accordance with USP <795> requirements for nonsterile gels, and beyond-use dating is assigned per stability-indicating assays and photostability data for each active pharmaceutical ingredient (API).[11]
Physicians may elect to customize ancillary excipients (e.g., humectants or soothing agents) for patients with sensitive skin, but the core concentration ratio of 6 %/2 %/5 % dapsone/niacinamide/spironolactone is maintained to preserve the evidence-based therapeutic balance.[12] Prescribers are reminded that, as a compounded medication, Acne DNS Gel has not undergone FDA pre-market approval; efficacy and safety rely on the clinical literature for each API and on pharmacist quality controls that meet state board and USP compounding standards.[13]
Apply a thin, even layer of Acne DNS Gel to clean, dry skin of the affected area once daily at bedtime; a twice-daily regimen may be considered for severe inflammatory lesions if tolerated.
The standard adult facial dose is approximately one pea-sized amount (0.25 mL), distributed evenly with clean fingertips.
Treatment response is typically evident within 4-8 weeks, with maximal benefit at 12 weeks; therapy may be continued long-term as maintenance provided tolerability is confirmed at follow-up visits.[40]
Dapsone exerts dual antimicrobial and anti-inflammatory actions by inhibiting dihydropteroate synthase in Cutibacterium acnes and reducing neutrophil-mediated oxidative damage through suppression of myeloperoxidase activity, thereby decreasing both bacterial colonization and inflammatory cascade amplification within pilosebaceous units.[14] In addition, dapsone down-regulates pro-inflammatory prostaglandins and leukotrienes, further mitigating papular-pustular activity.[15]
Niacinamide acts as a cell-permeable precursor of nicotinamide adenine dinucleotide and nicotinamide adenine dinucleotide phosphate, enhancing epidermal barrier function, stimulating ceramide synthesis, and attenuating nuclear factor-κB-driven cytokine release.[16] The vitamin also reduces hyperpigmentation by interfering with melanosome transfer and has been shown to normalize keratinocyte differentiation in the follicular infundibulum, decreasing comedone formation.[17]
Spironolactone, traditionally an oral mineralocorticoid antagonist, demonstrates topical antiandrogenic activity via competitive inhibition of the androgen receptor and blockade of 5α-dihydrotestosterone binding in sebaceous glands.[18] Percutaneous absorption studies confirm minimal systemic exposure with 5 % creams applied to limited body surface areas, yielding sebum reductions without clinically significant changes in serum potassium or aldosterone levels.[19] Topical spironolactone may also exert mild anti-inflammatory effects by decreasing leukotriene B₄ synthesis within sebocytes.[20]
Synergistically, the combination addresses the four canonical acne pathways: abnormal keratinization (niacinamide), excess sebum (spironolactone), microbial overgrowth (dapsone), and inflammation (all three).[21] Clinical guidance from the American Academy of Dermatology encourages multi-targeted therapy for moderate-to-severe acne and recognizes compounded combinations as a practical strategy when commercially fixed-dose products do not align with patient-specific needs.[22]
Use of Acne DNS Gel is contraindicated in individuals with known hypersensitivity to sulfonamides, spironolactone, or niacinamide, as well as those with a documented history of severe contact dermatitis to topical sulfones.[23] Patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency should avoid topical dapsone concentrations ≥ 5 % owing to the rare but serious risk of dose-dependent hemolytic anemia, particularly if extensive surface area is treated or occlusion is used.[24]
Although systemic exposure is minimal, spironolactone-containing preparations are not recommended for patients with chronic kidney disease, baseline hyperkalemia, or concurrent use of systemic potassium-sparing diuretics, angiotensin-converting-enzyme inhibitors, or angiotensin-receptor blockers, because cumulative absorption over time could theoretically exacerbate electrolyte imbalance.[25] Clinicians should counsel female patients planning pregnancy to discontinue the product at least one menstrual cycle before conception given spironolactone’s potential antiandrogenic effects on the male fetus.[26]
Additional cautions include avoidance of application to eczematous or sunburned skin, where barrier disruption may elevate systemic absorption of all APIs. Patients with active anemia, methemoglobinemia, or severe hepatic impairment should be assessed carefully before initiating therapy, and alternate treatments considered if risks outweigh benefits.[27]
Topical dapsone forms a brown-orange complex when co-applied with benzoyl peroxide; although the discoloration is benign, the combination may reduce dapsone’s antimicrobial effect and can stain clothing, so a minimum 30-minute interval between products-or the use of alternating morning/evening schedules-is advised.[28] Niacinamide is generally regarded as interaction-neutral; however, very high niacinamide concentrations (> 10 %) combined with acidic actives (e.g., alpha-hydroxy acids) may increase dermal irritation and theoretical nicotinic acid conversion, warranting staggered application.[29]
Because spironolactone competitively antagonizes androgen receptors, patients using topical clascoterone, systemic antiandrogens, or oral contraceptives may experience additive sebosuppressive effects; while beneficial for acne, cumulative hormonal modulation could enhance risk of oligomenorrhea or breast tenderness in sensitive individuals.[30] Clinicians should monitor for signs of local irritation when combining Acne DNS Gel with retinoids or manual exfoliation, as barrier compromise may potentiate erythema and desquamation.[31]
In phase 3 trials involving more than 4,000 treatment-site exposures, dapsone gel produced mild, transient dryness, erythema, and burning in approximately 7-10 % of subjects; these events typically resolved within two weeks of continued use or with temporary reduction in application frequency.[32] Rarely (< 0.1 %), dose-dependent methemoglobinemia has been reported, particularly in infants exposed via maternal transfer or in patients receiving large-area application under occlusion.[33]
Niacinamide at 2 % is well-tolerated; nonetheless, individuals with highly sensitive skin may experience flushing or transient pruritus, especially when niacinamide is layered over alpha-hydroxy acids or when the ambient formulation pH exceeds 7, increasing conversion to niacin.[34]
Topical spironolactone precipitates mild dryness or stinging in fewer than 5 % of users. Observable systemic adverse effects such as breast tenderness, menstrual irregularity, or hyperkalemia have not been documented with 5 % gels in trials up to 12 weeks when application areas remained limited to the face.[35]
Niacinamide is considered compatible with pregnancy at topical doses up to 5 % and is frequently recommended by dermatologists as a first-line anti-inflammatory adjunct for gestational acne because it lacks teratogenicity in animal models and human surveillance studies.[36] Evidence for topical dapsone suggests minimal systemic absorption and no teratogenic signal in trimesters 1-2; however, discontinuation during the final month is prudent to avoid theoretical neonatal hyperbilirubinemia.[37]
Spironolactone, as an androgen receptor antagonist, is contraindicated in pregnancy owing to the risk of feminization of a male fetus; despite negligible systemic exposure from 5 % gels, expert consensus advises against use during pregnancy or attempts to conceive.[38] Women of child-bearing potential should use reliable contraception and discontinue Acne DNS Gel at least one cycle before planned conception.[39]
Store the gel in its original, airtight container at 20 - 25 °C (68 - 77 °F. Protect from direct sunlight and do not freeze.
Photostability studies demonstrate that dapsone degrades to inactive sulfone photoproducts after prolonged UV exposure; therefore, keep the container tightly closed and avoid storing near windows or in vehicles during summer months.[41]
- Del Rosso, J. Q. (2007). Efficacy and safety of dapsone gel 5 % for the treatment of acne vulgaris. Cutis, 79(4), 300-308. https://cdn.mdedge.com/files/s3fs-public/Document/September-2017/081020171.pdf
- Abdel Rahman, A. et al. (2018). A topical cream containing niacinamide 4 % improves acne. Journal of Medical Science and Clinical Research, 6(3), 112-118. https://jmscr.igmpublication.org/v6-i3/84%20jmscr.pdf
- Faghihi, G. et al. (2022). Efficacy and safety of topical spironolacto68ne 5 % cream in acne treatment. Health Science Reports, 5(e317). https://onlinelibrary.wiley.com/doi/epdf/10.1002/hsr2.317
- American Osteopathic College of Dermatology. (2023). Dapsone. https://www.aocd.org/page/Dapsone
- Zasada, M. (2024). Mechanistic insights into niacinamide’s dermatologic functions. Antioxidants, 13(4), 425. https://www.mdpi.com/2076-3921/13/4/425
- American Academy of Dermatology. (2024). Guidelines of care for acne vulgaris. https://www.aad.org/practicecenter/quality/clinical-guidelines/acne
- Cleveland Clinic. (2023). Should I take spironolactone for acne? https://health.clevelandclinic.org/spironolactone-for-acne
- Sydel, S. (2023). Can you mix niacinamide with benzoyl peroxide? TheSkincareCulture. https://theskincareculture.com/can-you-mix-niacinamide-with-benzoyl-peroxide/
- Felber, S. (2014). Percutaneous absorption of spironolactone: A crossover study. Drug Research, 64(3), 145-150. https://link.springer.com/article/10.1007/BF03350151
- Drugs..com. (2025). Dapsone topical side effects. https://www.drugs.com/sfx/dapsone-topical-side-effects.html
- Acibadem Healthcare. (2023). Dapsone and G6PD deficiency: Risks and safety. https://www.acibademhealthpoint.com/dapsone-and-g6pd-deficiency-risks-and-safety/
- Ricotti, C. (2022). Everything to know about spironolactone for acne. Byrdie. https://www.byrdie.com/what-is-spironolactone
- Drugs..com. (2025). Benzoyl peroxide topical and dapsone interaction. https://www.drugs.com/drug-interactions/benzoyl-peroxide-topical-with-dapsone-topical-354-0-782-0.html
- Drugs..com. (2025). Niacinamide interaction checker. https://www.drugs.com/drug-interactions/niacinamide.html
- Drugs..com. (2025). Spironolactone disease interactions. https://www.drugs.com/disease-interactions/spironolactone.html
- Romper. (2024). Is niacinamide safe for pregnancy? https://www.romper.com/pregnancy/niacinamide-pregnancy
- Cardinali, C. (2025). Acne management during pregnancy and lactation. Dermatologic Therapy, 38(1), e1576. https://www.aideco.org/wp-content/uploads/2025/02/CARDINALI.pdf
- Drugs..com. (2025). Spironolactone pregnancy and breastfeeding warnings. https://www.drugs.com/pregnancy/spironolactone.html
- Cardinali, C. et al. (2025). Safety of dermatologic medications in pregnancy. Journal of the American Academy of Dermatology. https://www.jaad.org/article/S0190-9622%2824%2900109-9/fulltext
- Vogue. (2024). Pregnancy-safe skin care products. https://www.vogue.com/article/pregnancy-safe-skin-care-products
- Del Rosso, J. Q. (2008). Newer topical therapies for acne vulgaris. Cutis, 82(6), 400-406. https://cdn.mdedge.com/files/s3fs-public/Document/September-2017/080050400.pdf
- Joshi, R. (2023). Identification of oxidative degradation products of dapsone. Chromatographia, 86(3), 273-286. https://link.springer.com/article/10.1007/s10337-023-04234-7
- Maelove Skincare Science. (2023). Niacinamide stability and optimum pH. https://maelove.com/blogs/skincare-science/niacinamide-and-niacin-stability-and-optimum-pH
- Feldman, S. (2025). Guidelines of care for acne vulgaris-2025 update. Journal of the American Academy of Dermatology, 92(1), 1-35. https://www.jaad.org/article/S0190-9622%2823%2903389-3/fulltext
- Verywell Health. (2024). Adult acne treatments for women. https://www.verywellhealth.com/treating-adult-acne-in-women-15703
- Allure. (2018). Can niacinamide cause redness? https://www.allure.com/story/niacinamide-skin-care-redness-side-effect
- Edelstein, E. et al. (2017). Once-daily topical dapsone gel 7.5 % pooled efficacy analysis. Journal of the American Academy of Dermatology, 77(1), 133-140. https://www.jaad.org/article/S0190-9622(16)00159-6/fulltext
- Miiskin. (2025). Topical spironolactone: All you need to know. https://miiskin.com/acne/medications/topical-spironolactone/
- Amnuaikit, T. et al. (2020). Topical delivery of niacinamide: Influence of neat solvents. International Journal of Pharmaceutics, 582, 119330. https://www.sciencedirect.com/science/article/pii/S0378517320301216
- United States Pharmacopeia. (2023). USP General Chapter <795> Pharmaceutical Compounding-Nonsterile Preparations. https://www.usp.org/compounding/general-chapter-795
- WebMD. (2024). Niacinamide uses for skin: Benefits and side effects. https://www.webmd.com/beauty/what-to-know-about-niacinamide-skin-care
- Wikipedia. (2025). Pharmacodynamics of spironolactone. https://en.wikipedia.org/wiki/Pharmacodynamics_of_spironolactone
- Self. (2022). The potential niacinamide benefits you should know about. https://www.self.com/story/what-niacinamide-can-do-for-your-skin
- Health.com. (2024). What is niacinamide? https://www.health.com/niacinamide-benefits-8430985
- JCAD Online. (2019). Efficacy, safety, and dermal tolerability of dapsone gel 7.5 %. https://jcadonline.com/efficacy-safety-and-dermal-tolerability-of-dapsone-gel-7-5-in-patients-with-moderate-acne-vulgaris-a-pooled-analysis-of-two-phase-3-trials/
How long before I see improvement?
Most patients notice reductions in inflammatory lesions within 4 weeks and continued clearing through week 12.[24]
Can I wear makeup over the gel?
Yes. Allow the formulation to dry completely (about 60 seconds) before applying non-comedogenic cosmetics or sunscreen.[25]
Does the gel bleach fabrics like benzoyl peroxide?
No, but co-application with benzoyl peroxide may cause temporary surface discoloration; separate use by at least 30 minutes.[26]
Is it safe for sensitive skin?
The 2 % niacinamide component supports barrier repair, but a short patch test is advised; transient tingling may occur initially.[27]
Will I need blood tests?
Routine labs are not required for healthy individuals; patients with G6PD deficiency or renal disease should consult their physician.[28]
Can teenagers use this product?
Yes, under prescription supervision; compounded strength allows tailoring for adolescent skin needing multi-mechanistic control.[29]
What if I become pregnant while using the gel?
Discontinue immediately and inform your healthcare provider to discuss alternative, pregnancy-compatible therapies.[30]
May I combine the gel with topical retinoids?
Yes, but begin on alternate nights to minimize irritation and advance to nightly use as tolerated.[31]
Does it help with acne scarring?
While not a scar treatment, early control of inflammation and niacinamide-mediated pigment modulation may limit post-acne marks.[32]
Is there a purge period?
A brief flare can occur as follicular turnover accelerates, usually resolving within two weeks without treatment cessation.[33]
How much should I apply?
A pea-sized amount for the entire face is adequate; over-application increases irritation without improving efficacy.[34]
Can men use Acne DNS Gel?
Yes; male patients benefit from dapsone and niacinamide, but topical spironolactone’s antiandrogenic effects are modest and localized.[35]
Disclaimer
This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Administration Instructions
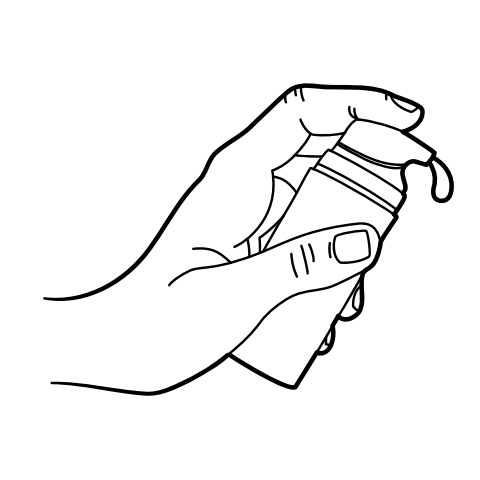
Pump Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Acne Extreme Gel
Acne Extreme Gel Acne Ultra Gel
Acne Ultra Gel Anti-Aging Vita Gel
Anti-Aging Vita Gel GHK-Cu Facial Serum
GHK-Cu Facial Serum Anti-Aging Siro Gel
Anti-Aging Siro Gel Tretinoin TAAN Cream
Tretinoin TAAN Cream 7-Keto DHEA Capsules
7-Keto DHEA Capsules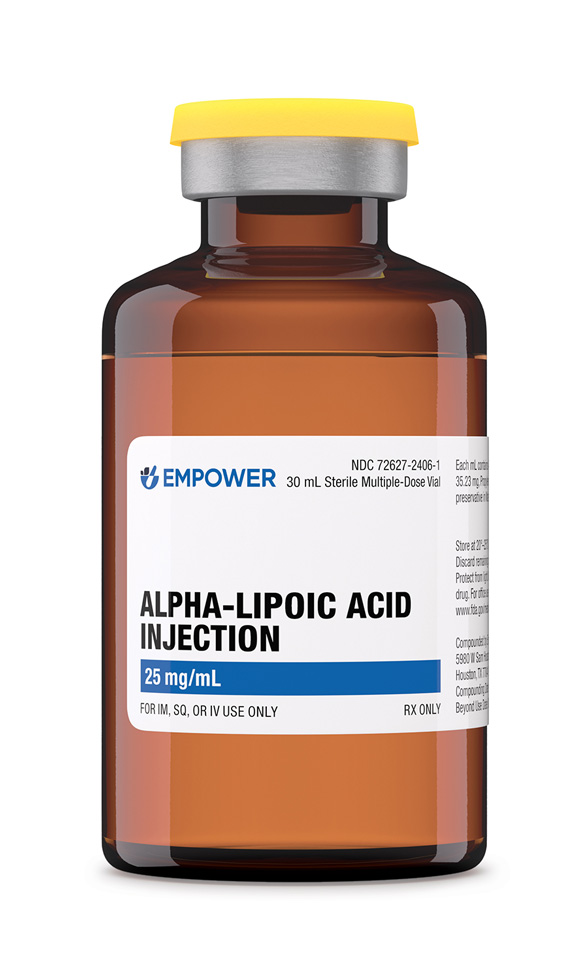 Alpha-Lipoic Acid Injection
Alpha-Lipoic Acid Injection NAD+ Cream
NAD+ Cream Biotin (Vitamin B7) Injection
Biotin (Vitamin B7) Injection