Minoxidil Capsules
This product is available solely through our 503A Compounding Pharmacy, ensuring personalized care and precision in every order. Please note that a valid prescription is required for purchase. If you do not have an account, please contact us.
Product Overview
† commercial product
Oral minoxidil (Loniten) is an antihypertensive agent; topical minoxidil (Rogaine) is used for alopecia. Topical minoxidil is likely effective in producing moderate hair growth in approximately 30% of men and 60% of women with common hereditary hair loss.[1] Lesser growth or a halt in the worsening of alopecia are also frequent outcomes.[2] Due to its potency and adverse reactions, oral minoxidil is used mainly for patients with severe, drug-resistant forms of hypertension. Tolerance to prolonged therapy with oral minoxidil does not appear to be a problem. Although the oral dosage form was originally approved in October 1979 for use in hypertension, minoxidil was first discovered in 1965. In August 1988 the topical formulation was approved for of alopecia. After declining Upjohn permission to market topical minoxidil as a non-prescription drug in July 1994, the 2% topical solution was subsequently approved for over-the-counter use in men with alopecia in February 1996. In September 1996, Pharmacia and Upjohn petitioned the FDA to increase the topical solution formulation from 2% to 5%; the higher-strength solution has been shown to elicit a more rapid hair growth response (8 weeks vs. 16 weeks) and to regrow an average of 45% more hair than Rogaine Regular Strength.[2] The 5% topical solution (Rogaine Extra Strength) for common hereditary hair loss was approved FDA in November 1997. Approval to market 2% topical solution to women was granted October 1996. Minoxidil foam (Men’s Rogaine Foam) was approved for men in January 2006; potential advantages over the solution formulation include the absence of propylene glycol (potential irritant), ability to limit spread of medication, and less time to dry after application.[3]
Minoxidil has a direct vasodilatory effect on arterial smooth muscle, causing a reduction in peripheral resistance and blood pressure. Minoxidil does not exhibit CNS or adrenergic neuronal blocking effects; minoxidil retains its activity despite adrenergic denervation. Cyclic adenosine monophosphate (cAMP) may contribute to relaxation of vascular smooth muscle. Minoxidil-induced delay in the hydrolysis of cAMP via inhibition of phosphodiesterase may contribute to the drug’s vasodilatory action.
All direct vasodilators produce a sympathetic response including an increase in heart rate, stroke volume, and cardiac output, and a marked increase in plasma renin activity, which, in turn, leads to increased sodium and water retention. This increased renin release is believed to be partially mediated by the beta-adrenergic system. These compensatory responses tend to diminish the hypotensive effects of minoxidil. Additional therapeutic effects can be achieved by using a beta-blocker to offset the predictable sympathetic stimulation caused by minoxidil. Methyldopa may be used if beta-blocker therapy is contraindicated; however, because of its delay in onset, methyldopa must be initiated 24 hours prior to initiating minoxidil. Vasodilator-induced fluid retention is somewhat related to the potency of the vasodilator. Due to its potency, fluid retention occurs routinely with minoxidil. Often, this fluid retention requires concomitant use of loop diuretics (see Adverse Reactions). Triple-drug therapy consisting of a loop diuretic, beta-blocker, and minoxidil produces prompt, sustained reduction in blood pressure in patients with severe hypertension.[4][5]
Minoxidil preferentially dilates arterioles; therefore, postural hypotension may occur during therapy. As an antihypertensive, minoxidil does not lead to improvements in LVH. Minoxidil may actually worsen LVH, potentially due to reflex tachycardia and sympathetic stimulation, which may counteract the benefits of afterload reduction.[6] Minoxidil does not affect glucose tolerance or serum lipids.
The exact mechanism responsible for minoxidil-induced hair growth is not known, but appears to be independent of vasodilation.[7] While systemic therapy will stimulate hair growth, topical therapy usually does not cause hypotension. Current evidence suggests the primary action of topical minoxidil is to decrease the latent period of the hair cycle. The latent period (the time between shedding of telogen hair and the onset of the next anagen) is typically prolonged in male pattern balding; however, this effect has not been demonstrated in balding females.[8] Calcium may also be involved in the process of hair regrowth. In the presence of calcium, epidermal growth factor (EGF) inhibits hair growth. The entry of calcium into a hair cell is opposed by potassium channel openers, such as minoxidil; therefore, EGF-induced inhibition of hair will be opposed by the action of minoxidil, and hair will grow more proficiently. Biopsy specimens have not demonstrated evidence of new follicle formation with the use of minoxidil.[1] Furthermore, minoxidil appears to affect only suboptimal follicles with no further stimulation of normal hair follicles.[7] Minoxidil also may alter the metabolism of androgens in the scalp. Minoxidil increases 17 beta-hydroxylated dehydrogenase activity by almost 40% in dermal papilla cells of a balding scalp, whereas the effect is much less in a nonbalding scalp. Whether this modification in testosterone metabolism of cells of a balding scalp is related to the therapeutic effect of minoxidil is unknown.[9]
Minoxidil has been reported to produce cardiac lesions in animals. Some lesions are characteristic of other drugs that can cause tachycardia and/or hypotension (e.g., isoproterenol, hydralazine). These effects are more likely to occur in patients with compromised renal function and in patients with connective tissue disease, uremic syndrome, CHF, or minoxidil-induced fluid retention.
Systemic minoxidil is a potent vasodilator with potential to produce hypotension and reflex tachycardia; serious complications may occur. Minoxidil is relatively contraindicated in patients with cardiac disease (including angina, coronary artery disease, recent or acute myocardial infarction), or cerebrovascular disease because a reflex increase in heart rate and decrease in blood pressure can exacerbate these conditions. Minoxidil is relatively contraindicated in patients with coronary insufficiency, including angina, to avoid the risk of reflex tachycardia and angina exacerbation. Minoxidil may cause pericardial effusion which occasionally may progress to cardiac tamponade. Reserve oral minoxidil for hypertension in patients who do not respond adequately to maximum therapeutic doses of a diuretic (loop diuretic suggested) concurrently with 2 other antihypertensive agents. In experimental animals, minoxidil has been shown to induce several types of myocardial lesions as well as other adverse cardiac effects. Minoxidil must be administered under close supervision, usually in combination with therapeutic doses of a beta-blocker to prevent reflex tachycardia and increased myocardial workload. Minoxidil is often given with a diuretic (preferably a diuretic which acts within the ascending limb of the loop of Henle) to prevent fluid accumulation and peripheral edema. When first administering minoxidil to patients with malignant hypertension and those already receiving guanethidine to avoid rapid or large orthostatic reductions in blood pressure, minoxidil use requires a specialized care setting, specifically hospitalization. Although minoxidil does not directly cause orthostatic hypotension, administration to patients receiving guanethidine can result in profound orthostatic effects. When possible, guanethidine should be discontinued well before minoxidil is initiated. Otherwise, minoxidil therapy should be started in the hospital; the patient should remain hospitalized until the risk of excessive orthostatic effects is minimized and the patient is able to avoid activities that induce orthostatic hypotension.
Minoxidil is relatively contraindicated in patients with renal disease, preexisting pulmonary hypertension, or chronic congestive heart failure not secondary to hypertension because the drug can cause an increase in pulmonary artery pressure, which could be detrimental to these patients. Use of minoxidil has been associated with the development of pericardial effusion and tamponade in some patients, and it may be more likely to occur in patients with renal disease. Since approximately only 10% of active drug is eliminated unchanged via the kidneys, minoxidil can be used safely in patients with renal impairment. Renal elimination, however, may be reduced and dosage adjustment may be necessary. Avoid use of minoxidil in patients with severe renal failure (CrCl < 10 ml/min). Minoxidil is contraindicated in patients with pheochromocytoma because the hypotensive effects of the drug can stimulate catecholamine secretion. Systemic effects resulting from topically administered minoxidil are unlikely but theoretically could occur if the drug is overused. Skin abrasion or irritations, such as excoriations, psoriasis, or sunburn, can increase the systemic absorption of topically administered minoxidil. Reported clinical experience has not identified differences in responses in geriatric adults vs. younger adult patients. In general, systemic dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.[10] Topical minoxidil use carries no special precaution in the elderly, but any patient experiencing dizziness or faintness should discontinue topical use.[1] The federal Omnibus Budget Reconciliation Act (OBRA) regulates medication use in residents of long-term care facilities (LTCFs). According to OBRA, antihypertensive regimens should be individualized to achieve the desired outcome while minimizing adverse effects. Antihypertensives may cause dizziness, postural hypotension, fatigue, and there is an increased risk for falls. There are many drug interactions that can potentiate the effects of antihypertensives. Some agents require a gradual taper to avoid adverse consequences caused by abrupt discontinuation.[11]
When used with topical minoxidil, systemic cyclosporine may intensify side effects such hypertrichosis. After quitting topical minoxidil for two months, the hypertrichosis symptoms significantly improved. The effectiveness of topical minoxidil may also be decreased by co-administration of baby aspirin. This decrease in effectiveness is thought to be caused by baby aspirin’s adverse suppression of sulfotransferase enzymes in human hair. [16]
The adverse reaction profile for minoxidil depends upon its use. Systemic adverse reactions are unlikely from topical administration. Placebo-controlled trials with topical minoxidil only showed an increase in dermatological effects from the active drug.
Minoxidil is a peripheral vasodilator. All direct vasodilators produce a marked increase in plasma renin activity, which leads to water and sodium retention and sometimes congestive heart failure. This renin release is believed to be partially mediated by the beta-adrenergic system. The degree of fluid retention is somewhat related to the potency of the vasodilator. Due to its potency, fluid retention (edema) occurs routinely with oral minoxidil and usually requires concomitant administration of a loop diuretic. Without a diuretic, rapid fluid retention can occur within a few days of minoxidil therapy. Temporary edema occurred in 7% of patients who were not edematous when minoxidil was initiated.[10] Ascites also has been reported. A restricted dietary intake of sodium can minimize fluid retention and resultant peripheral edema. Rarely, fluid retention is refractory to diuresis and discontinuation of minoxidil is required. Vasodilation may also produce headache.
Minoxidil causes reflex tachycardia; sinus tachycardia may occur. Angina may become apparent, or worsen, secondary to increased myocardial oxygen demand associated with tachycardia and increased cardiac output. Tachycardia and subsequent angina usually can be prevented with the coadministration of a beta-blocker or other sympathetic nervous system suppressant.[10]
Minoxidil has been shown to transiently lower hematocrit, hemoglobin, and erythrocyte count by approximately 7%. Serum creatinine and BUN also have been shown to increase an average of 6% in patients on minoxidil therapy. Increases in alkaline phosphatase, without other evidence of hepatic abnormality, also has been reported. During the course of therapy, these laboratory abnormalities have been shown to return to pretreatment values. Thrombocytopenia and leukopenia also have been reported.[10]
Hypertrichosis (elongation, thickening, and enhancement of fine body hair), without evidence of virilism or endocrine abnormalities, is an embarrassing adverse effect that often occurs with oral minoxidil. This effect is usually evident within 3-6 weeks of therapy and occurs on the temples, between the eyebrows, or in the sideburn area. Hair growth also can appear on the arms, legs, and scalp. It is reversible following discontinuation of the drug.[10]
Oral minoxidil has occasionally been associated with appearance of a bullous rash and Stevens-Johnson syndrome. Topical minoxidil therapy produces local dermatological reactions including contact dermatitis, local burning, pruritus, erythema, or xerosis. Many other adverse effects have been reported during administration of topical minoxidil preparations, but none has been directly attributed to the drug.[10]
Gastrointestinal adverse effects associated with orally administered minoxidil include nausea and vomiting.[10]
Minoxidil is classified as pregnancy risk category C. Although no adequate human studies have examined the effects of this drug on the fetus, animal reproduction studies have shown adverse effects, including reduced ability to conceive and a reduced survival of offspring. Dysmorphic facial features and hypertrichosis were observed in an infant whose mother received a daily minoxidil dosage of 10 mg during pregnancy.[12] Therefore, in making the decision to administer this drug during pregnancy, the potential risks to the fetus and possible difficulty in conceiving must be weighed against the potential benefits to the mother.[13]
According to the manufacturer, minoxidil should not be administered to a nursing mother.[6800] The American Academy of Pediatrics (AAP) considers minoxidil to be generally compatible with breastfeeding [14]; however, other experts are less comfortable with the use of this potent antihypertensive agent in nursing mothers. In one case report of a woman taking minoxidil 5 mg PO twice daily, minoxidil was rapidly excreted into the breast milk. After two months, no adverse events were reported in the nursing infant. The effect of prolonged exposure during breastfeeding is unknown.[15] Examples of other antihypertensives with more data in this population that have been classified as usually compatible with breastfeeding by the AAP and may be possible alternatives for some patients include enalapril, hydrochlorothiazide, methyldopa, and propranolol.[14] It is not known whether topical minoxidil is distributed into breast milk. Consider the benefits of breastfeeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breastfeeding infant experiences an adverse effect related to a maternally administered drug, healthcare providers are encouraged to report the adverse effect to the FDA.
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond-use date. Do not flush unused medications or pour down a sink or drain.
- DeVillez RL. The Therapeutic Use of Topical Minoxidil. Dermatol Clin 1990;8:367-74.
- Olsen EA, Dunlap FE, Funicella T, et al. A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. J Am Acad Dermatol 2002;47:377-85.
- Olsen EA, Whiting D, Bergfeld W, et al. A multicenter, randomized, placebo-controlled, double-blind clinical trial of a novel formulation of 5% minoxidil topical foam versus placebo in the treatment of androgenetic alopecia in men. J Am Acad Dermatol 2007;57(5):767-74. Epub 2007 Aug 29
- Bauer JH, Alpert MA. Rapid reduction of severe hypertension with minoxidil. J Cardiovasc Pharmacol 1980;2 Suppl:S189-99.
- Alpert MA, Bauer JH. Rapid control of severe hypertension with minoxidil. Arch Intern Med 1982;142(12):2099-104.
- Pogatsa-Murray G, Varga L, Varga A, et al. Changes in left ventricular mass during treatment with minoxidil and cilazapril in hypertension patients with left ventricular hypertrophy. J Hum Hypertens 1997;11(3):149-56.
- Buhl AE. Minoxidil’s action in hair follicles. J Invest Dermatol 1991;96:73S-4S.
- Messenger AG, Rundegren J. Minoxidil: mechanisms of action on hair growth. Br J Dermatol 2004;150:186-194.
- Sato T, Tadokoro T, Sonoda T, et al. Minoxidil increases 17b-hydroxysteroid dehydrogenase and 5a-reductase activity of cultured human dermal papilla cells from balding scalp. J Derm Sci 1999;19:123-5.
- Loniten (minoxidil) tablets package insert. Kalamazoo, MI: Pharmacia; 2006 Feb.
- Health Care Financing Administration. Interpretive Guidelines for Long-term Care Facilities. Title 42 CFR 483.25(l) F329: Unnecessary Drugs. Revised 2015.
- Kaler SG, Patrinos ME, Lambert GH, et al. Hypertrichosis and congenital anomalies associated with maternal use of minoxidil. Pediatrics 1987;79:434-6.
- Minoxidil tablets package insert. Corona, CA: Watson Laboratories, Inc; 2009 Jun.
- American Academy of Pediatrics (AAP) Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics 2001;108(3):776-789.
- Valdivieso A, Valdes G, Spiro TE, et al. Minoxidil in breast milk. Ann Intern Med. 1985;102:135. Letter.
- Badri T, Nessel TA, Kumar D D. Minoxidil. [Updated 2021 Dec 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482378/
Related medications
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
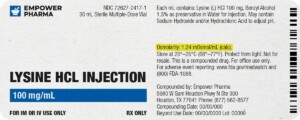
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.



 Finasteride Tablets
Finasteride Tablets Biotin / Minoxidil / Spironolactone Capsules
Biotin / Minoxidil / Spironolactone Capsules Biotin / Minoxidil Capsules
Biotin / Minoxidil Capsules Biotin / Finasteride / Minoxidil Capsules
Biotin / Finasteride / Minoxidil Capsules Hair Restore Extreme Scalp Solution
Hair Restore Extreme Scalp Solution Hair Restore Ultra Scalp Solution
Hair Restore Ultra Scalp Solution Hair Restore D Scalp Solution
Hair Restore D Scalp Solution Hair Restore Lite Scalp Solution
Hair Restore Lite Scalp Solution GHK-Cu Scalp Solution
GHK-Cu Scalp Solution