Product Overview
Melasma HQ Cream is a prescription-only, custom-compounded dermatological cream intended for the treatment of melasma and related hyperpigmentation disorders. It contains four active ingredients, hydroquinone, tretinoin, azelaic acid, and hydrocortisone, combined in a topical formulation. The cream is prepared under Section 503A of the U.S. Federal Food, Drug, and Cosmetic Act, meaning it is made by a compounding pharmacy for individual patients and has not undergone FDA approval for safety or efficacy.[1] Three strength combinations are available (given as percentages of hydroquinone/tretinoin/azelaic acid/hydrocortisone in a 30 g jar): 8/0.1/15/1%, 6/0.1/15/1%, and 4/0.1/15/1%. By including multiple agents, Melasma HQ Cream targets different steps in the pigmentation process and may achieve more pronounced skin lightening than single-agent therapies.
Hydroquinone is a depigmenting agent that may reduce melanin production, tretinoin is a retinoid that could increase skin cell turnover (helping exfoliate pigment), azelaic acid potentially inhibits melanocyte activity and inflammation, and hydrocortisone is a mild corticosteroid that may limit irritation and pigmentary stimuli.[2] This combination approach, sometimes termed “triple therapy” (hydroquinone + retinoid + steroid), is a well-recognized strategy in melasma treatment and has been shown to produce superior outcomes compared to any of the individual components alone.[3] Notably, the addition of azelaic acid in this compounded cream provides a further mechanism of action; azelaic acid monotherapy at 15-20% has demonstrated efficacy comparable to 4% hydroquinone in melasma, so its inclusion can augment the depigmenting effect.[4] Melasma HQ Cream is not an over-the-counter product and must be prescribed by a healthcare provider. Because it is compounded to order, it is not FDA-approved, and its formulation can be tailored to the patient’s needs.[1] It is generally used as a short-term intervention to achieve melasma clearance, with the understanding that melasma is a chronic condition prone to recurrence. Strict sun avoidance and use of sunscreen are advised during and after treatment to maintain results and prevent relapses. In summary, Melasma HQ Cream offers a multi-pronged topical therapy for stubborn pigmentation, delivered through a 503A compounding pharmacy, and its use is monitored by dermatologists due to the potent nature of its ingredients and lack of formal FDA evaluation.[1]
Application Frequency: The typical dosage regimen for Melasma HQ Cream is once daily application, at night.[5] It is usually applied in the evening because one of the ingredients, tretinoin, can be deactivated by sunlight and also makes the skin more sensitive to UV; nighttime application maximizes efficacy and reduces sun exposure during the immediate post-application period. Patients are generally instructed to use a thin layer of the cream on the affected areas of melasma. Only a small amount (for example, a pea-sized dollop) is needed for the entire face; using more does not yield faster results and may increase the likelihood of irritation. Before application, the skin should be cleansed with a mild, non-irritating cleanser and pat-dried. It’s recommended to wait a few minutes after washing so that the skin is completely dry (applying strong actives to damp skin can sometimes enhance penetration and irritation). A thin film of the cream is then gently spread over each melasma patch, extending slightly (about half an inch) into the surrounding normal skin to blend the edges.[5] Care should be taken to avoid contact with the eyes, lips, and nostrils; do not apply on the eyelids or too close to the corners of the mouth or nose. If the cream accidentally gets on those sensitive areas, rinse thoroughly with water. After applying, patients should wash their hands to remove any residual cream, so that they don’t inadvertently spread it to other areas (or into their eyes) during the night. The cream is left on overnight and then washed off in the morning during the normal face routine (unless directed otherwise by the physician). Occlusive dressings or bandages over the treated areas are not advised, as covering the area can increase absorption of the ingredients beyond intended levels. In the morning following use, sunscreen should be applied as the final step of the routine (see below).
Treatment Duration: Melasma HQ Cream is intended for short-term use rather than indefinite daily use. A typical course of treatment lasts around 8 to 12 weeks of nightly applications.[5] In clinical studies of similar triple-combination creams (for example, the FDA-approved Tri-Luma® which contains hydroquinone 4%, tretinoin 0.05%, fluocinolone 0.01%), an 8-week regimen produced significant melasma improvement in many patients, and usage beyond 8 weeks was not routinely evaluated in those trialsaccessdata.fda.gov. In practice, dermatologists often prescribe this compounded cream for a few months and then reassess. If substantial clearing of melasma is achieved before 12 weeks, they may have the patient stop earlier.
Continuous long-term use is not recommended because it raises the risk of side effects (like skin atrophy or ochronosis from hydroquinone) and because melasma can often be maintained with gentler therapies once initial improvement is reached.[5] This cream is not meant for maintenance therapy of melasma; after the initial intensive treatment phase, doctors typically transition the patient to maintenance strategies, such as daily sunscreen (absolutely essential), possibly a less potent lightening agent (azelaic acid or vitamin C), or other modalities, rather than keeping them on the hydroquinone/tretinoin/steroid continuously.[1] Some patients with very recalcitrant melasma might undergo repeat courses of the triple cream, but these are usually separated by off-treatment intervals to give the skin a break.
Adjunct Measures: A critical part of the “dosage” instructions is concurrent sun protection. The effectiveness of Melasma HQ Cream will be greatly undermined if the patient continues to get UV exposure on the treated skin. Therefore, patients must use a broad-spectrum sunscreen (SPF 30 or higher) every morning on the face, reapplying during the day if outdoors.[5] In fact, many clinicians have patients begin diligent sunscreen use even before starting the cream, as sunscreen alone can prevent melasma from darkening further. Sun avoidance (seeking shade, wearing a wide-brimmed hat) is strongly encouraged. These measures are considered part of the treatment regimen and should continue even after the cream is discontinued, to prolong the remission of melasma.
Special Instructions: If the patient experiences excessive irritation, the prescribing doctor may adjust the dosing frequency. For example, the cream might be used every other night or even every third night initially, until the skin builds tolerance, then increased to nightly as tolerated. Any such adjustments should be done under medical guidance. Patients are usually reviewed by their dermatologist after a few weeks to ensure the treatment is on track. If no improvement is seen by ~8-12 weeks, the physician might discontinue the cream because lack of response by that time could indicate that the melasma is not responding to topical therapy (some melasma, especially dermal/deep type, is very resistant). On the other hand, if melasma has significantly cleared before 8 weeks, the doctor might decide to stop earlier to minimize exposure. When stopping the cream after the course is over, some doctors taper usage (for example, using it every other night for a week or two, then twice a week) rather than abrupt cessation, to avoid rebound pigmentation; though this taper may not be necessary in all cases.
In summary, the dosing of Melasma HQ Cream is once nightly, for up to about 2-3 months, applying a thin layer to affected areas. Strict adherence to sun protection and gentle skincare is part of the regimen. Patients should follow the specific instructions given by their healthcare provider, as compounding pharmacies often include a patient information leaflet with similar guidance. Never exceed the prescribed frequency or duration on your own; if you miss a dose one night, do not double up the next day; simply resume the next night. And always communicate with your provider about how your skin is tolerating the treatment, so dosing can be adjusted if necessary. By following these dosing guidelines, patients have the best chance of safely achieving improvement in their melasma.[5]
Hydroquinone: Hydroquinone (HQ) is the primary skin-lightening agent in the cream. It works by inhibiting melanogenesis, the process of melanin (pigment) production in the skin. Specifically, hydroquinone reversibly blocks the enzyme tyrosinase, which normally catalyzes the oxidation of tyrosine to melanin within melanocytes. This inhibition leads to a gradual decrease in new melanin synthesis. Hydroquinone also causes selective damage to melanocytes and melanosomes (pigment granules), which further contributes to pigment reduction. Over time, areas of hyperpigmentation may lighten as existing melanin breaks down and less new pigment is formed. HQ has long been considered a gold-standard topical therapy for hyperpigmentation, and its effects typically become visible after several weeks of consistent use (often around 5-7 weeks according to clinical reports) . However, hydroquinone’s action is not permanent; without continued use or maintenance therapy, pigmentation can gradually return once melanin production resumes.[2]
Tretinoin: Tretinoin is an all-trans retinoic acid (vitamin A derivative) that promotes skin cell turnover and epidermal renewal. In the context of melasma, tretinoin helps expel melanin by accelerating the exfoliation of pigmented keratinocytes and increasing the rate of new skin cell production. It may also enhance the penetration of hydroquinone into the skin by thinning the outer stratum corneum. Beyond its exfoliative effects, tretinoin has been found to affect melanogenesis at a molecular level: it may reduce the transcription of tyrosinase and other melanogenic enzymes, and it could interfere with the transfer of melanin from melanocytes to surrounding skin cells.[4] By these actions, tretinoin gradually contributes to lightening of hyperpigmented patches. An important aspect of tretinoin’s role is synergistic: when used in combination with hydroquinone, tretinoin not only provides its own modest lightening effect but also improves the efficacy of hydroquinone. (For example, tretinoin pre-treatment can increase hydroquinone’s pigment reduction by allowing it to reach deeper epidermal layers.) In summary, tretinoin speeds up the turnover of pigmented skin and augments the overall depigmenting outcome of the cream.[4] Patients should be aware that tretinoin often causes an initial phase of skin irritation and peeling (a “retinoid reaction”) as the skin acclimates, and it also heightens sensitivity to sunlight, necessitating diligent sun protection during therapy.[5]
Azelaic Acid: Azelaic acid (AZA) is a naturally occurring dicarboxylic acid with multiple dermatologic effects. In melasma treatment, azelaic acid serves as an additional depigmenting agent and anti-inflammatory component. It competitively inhibits tyrosinase (the same enzyme targeted by hydroquinone), thereby reducing melanin synthesis in hyperactive melanocytes. Interestingly, azelaic acid tends to selectively impact abnormal or overactive melanocytes while having minimal effect on normally pigmented skin.[2] This means it can lighten hyperpigmented lesions without causing generalized bleaching of unaffected skin. Azelaic acid also has antibacterial and keratolytic properties (useful in acne/rosacea) and an ability to reduce oxidative stress in the skin; these anti-inflammatory and antioxidant effects may help melasma by mitigating inflammatory triggers for pigmentation. In some studies, combining azelaic acid with a retinoid (like tretinoin) or glycolic acid produced faster or greater lightening of melasma than azelaic acid alone. Within Melasma HQ Cream, azelaic acid works alongside hydroquinone to suppress pigment production, and it may soothe some irritation through its anti-inflammatory action, making the regimen more tolerable. Overall, azelaic acid provides a complementary mechanism that broadens the cream’s approach to clearing hyperpigmentation.[7]
Hydrocortisone: Hydrocortisone is a low-potency topical corticosteroid included primarily to reduce inflammation and irritation. Topical corticosteroids in melasma therapy have a dual purpose: (1) they may directly lighten hyperpigmented lesions by reducing melanin-stimulating inflammation, and (2) they temper the skin’s inflammatory response to irritants like tretinoin and hydroquinone, thereby improving patient tolerance.[3] Inflammatory mediators (such as prostaglandins and leukotrienes) are known to stimulate melanocyte activity; hydrocortisone can inhibit the release of these mediators, which could indirectly lead to less pigment production in the skin.[4] On its own, hydrocortisone’s pigment-lightening effect is mild and generally short-lived; topical steroids are rarely used as monotherapy for melasma due to limited efficacy and potential side effects. However, when combined with hydroquinone and tretinoin (as in this cream), hydrocortisone has a synergistic benefit: it helps “prep” the skin by calming irritation, allowing the other actives to work more effectively, and possibly provides a transient bleaching effect by reducing melanin deposition from inflammation. By decreasing redness, itching, and irritation, the steroid enables patients to continue treatment longer with the potent actives. It is important to note that hydrocortisone is included in a low concentration (1%) appropriate for short-term facial use; stronger steroids, while more potent, carry higher risks and are not generally used for extended periods on the face. In summary, hydrocortisone’s mechanism in Melasma HQ Cream is to create a more favorable, less inflamed environment for pigment reduction and to prevent or minimize the irritant dermatitis that hydroquinone and tretinoin can cause.[3]
Melasma HQ Cream should not be used in any patient with a history of hypersensitivity to its active ingredients or excipients. This includes allergy to hydroquinone or any chemically related phenolic compounds, tretinoin or other retinoids, azelaic acid, hydrocortisone or other corticosteroids, or to preservatives often used in compounded creams (for example, metabisulfite or parabens).[3] If a patient has previously experienced allergic contact dermatitis from hydroquinone or other bleaching creams, they must avoid this formulation. Signs of allergy might include intense redness, swelling, itching, or hives at the application site; if these occur, treatment should be discontinued immediately. It is advisable to perform a test application on a small area of skin (a patch test) prior to broader use, especially in individuals with eczema or sensitive skin, to rule out severe hypersensitivity.[8]
Use of this cream is contraindicated on broken or damaged skin. Do not apply it to areas that are cut, abraded, or sunburned, or to eczematous or inflamed skin, because the disrupted skin barrier can lead to heightened absorption and increased irritation. Patients should wait until any skin wounds or sunburn in the treatment area have healed before starting therapy. Similarly, application to mucous membranes (inside the nose or mouth) or very sensitive areas (like the eyelids or lips) is to be avoided; inadvertent contact with such areas should be rinsed off immediately with water.[5] Careful application, using only a thin layer to the melasma spots, will help prevent the cream from spreading onto unintended regions of skin.
This compounded formulation has not been proven safe for pregnant women. In fact, use in pregnancy is generally advised against (see “Pregnancy” section below). Hydroquinone in particular has an unknown safety profile in pregnancy and substantial systemic absorption, so it should be avoided unless clearly necessary. Likewise, tretinoin (a retinoid) is contraindicated in pregnancy due to teratogenic potential. Women who are or might become pregnant should not use Melasma HQ Cream without explicit direction and close supervision from a physician. For breastfeeding mothers, caution is also urged; it is not known whether topical hydroquinone or tretinoin are appreciably absorbed and excreted in breast milk, but out of an abundance of caution, many providers will recommend against use while nursing.[10] Pediatric use is another area of uncertainty: the safety and efficacy in children (especially those under 12 years old) have not been established, so the cream is generally not prescribed in the pediatric population.[8]
Patients with certain skin conditions or infections should not use this cream on affected sites. The steroid component (hydrocortisone) can exacerbate cutaneous infections; therefore, areas of active viral, bacterial, or fungal infection (for example, herpes simplex cold sores, impetigo, or ringworm) should not be treated with Melasma HQ Cream unless the infection is also being properly managed. Using a corticosteroid on untreated skin infections may allow the infection to worsen or spread.[5] Likewise, patients with rosacea or perioral dermatitis on the face should use extreme caution; topical steroids can aggravate these conditions, so applying the cream to areas with rosacea flare-ups or around the mouth (where perioral dermatitis presents) is contraindicated or should be done only under dermatologist guidance⁵. If melasma overlaps with an area of active dermatitis, that condition should be controlled first before the pigmentation is treated.
Systemic conditions can also influence safety. Although the ingredients of this cream have primarily local action, chronic application over large areas could lead to some systemic absorption of hydrocortisone. Thus, patients with Cushing’s syndrome (hypercortisolism) or those who require strict control of blood sugar (e.g., diabetes mellitus) should use the cream cautiously, as systemic corticosteroid absorption may worsen these conditions (e.g., raising blood glucose or exacerbating adrenal suppression).[5] In general, the treatment area for melasma is localized (face), so significant systemic steroid effects are unlikely; nonetheless, patients with a history of steroid-related complications should discuss risks with their doctor. True systemic allergic reactions to topical medications are rare but possible; anyone with a prior anaphylactic reaction to similar products should not use this cream. Finally, if excessive irritation (beyond mild peeling and redness) develops during use, for instance, severe burning, blistering, or edema, this may be a sign of intolerance or allergic reaction, and the patient should discontinue the cream and consult their healthcare provider.[3]
Because Melasma HQ Cream is applied topically, its drug-drug interaction potential is primarily localized to the skin. Nonetheless, certain concomitant products can interfere with its action or increase irritation. Concurrent use of peroxide-containing products on the same area should be avoided. Using hydroquinone together with benzoyl peroxide (often found in acne medications) or hydrogen peroxide can cause a chemical reaction that temporarily stains the skin a brownish color.[8] This reversible “staining” results from oxidation and can usually be washed off, but it is undesirable. Therefore, patients should not apply any benzoyl peroxide creams, peroxide cleansers, or hair dyes/bleaches on areas treated with Melasma HQ Cream to prevent this interaction.[8] If a patient needs both acne treatment and the melasma treatment, they should use them at different times (e.g., benzoyl peroxide in the morning and Melasma HQ Cream at night) and confirm the plan with their physician to minimize any inactivation of tretinoin or skin staining issues.
Other topical skincare products can intensify irritation and should be used carefully with Melasma HQ Cream. In particular, products that dry or exfoliate the skin, such as alcohol-based toners, astringents, harsh soaps, scrubs, or products containing acids (salicylic acid, glycolic or lactic acid), could lead to cumulative irritation if layered with the cream.[5] It is recommended to avoid or greatly limit the use of such products on areas where the cream is applied. Gentle, pH-balanced cleansers and non-medicated, non-irritating moisturizers are preferable during the treatment course. Patients can use a moisturizer to alleviate dryness, but it’s best to apply it at a different time of day (or at least 30 minutes after the medication) so as not to dilute the active drugs. If using cosmetics, choose ones without irritating ingredients (like fragrance or alcohol) to reduce the risk of additional skin stress. Importantly, do not use other prescription topicals (e.g., acne medications or other depigmenting agents) on the same area unless directed by your dermatologist. Combining multiple treatments without guidance can lead to over-exfoliation or chemical conflicts on the skin. For instance, applying a sulfur- or resorcinol-containing product alongside tretinoin could cause unpredictable irritation. Always let your healthcare provider know about any other skincare or medications you are using on your face⁸. They will advise whether to pause them or how to stagger their use while on Melasma HQ Cream.
Sun exposure and photosensitizers: One of the most critical “interactions” is with ultraviolet light. Tretinoin can make the skin significantly more sensitive to UV radiation, meaning there is a higher risk of sunburn and photodamage if one is not careful.[5] Hydroquinone’s efficacy can also be undermined by UV exposure, as sunlight stimulates melanocytes and can counteract the bleaching effect. Therefore, patients must practice diligent sun avoidance and protection during therapy. This includes wearing broad-spectrum sunscreen (SPF 30 or higher) every day on the treated areas, even if just going about daily activities.[5] Protective clothing such as a wide-brimmed hat is also recommended when outdoors. Sunlamps and tanning beds should be completely avoided while using this cream.[5] If a patient is concurrently on any photosensitizing drugs (for example, certain antibiotics like doxycycline, or diuretics like HCTZ, etc.), they should be extra cautious, as the combination could make them even more prone to UV-induced burns or pigmentation. Essentially, Melasma HQ Cream “interacts” with sun exposure by increasing vulnerability, so strict photoprotection is mandatory.
From a systemic perspective, drug-drug interactions are unlikely because the medication’s absorption is minimal. The active components act locally in the skin and only trace amounts, if any, reach the bloodstream.[8] As a result, using this cream is not known to affect or be affected by most oral medications, supplements, or systemic therapies. Nonetheless, it is standard practice for patients to inform all their healthcare providers about the medications they use, including compounded topicals. There may be scenarios where a doctor advises modifications; for example, if the patient is using another topical corticosteroid elsewhere, they will monitor overall steroid exposure to prevent additive effects. In general, however, Melasma HQ Cream can be used safely alongside most other medications as long as they are used in different routes or areas (with the aforementioned precautions for topicals). Summarily, to avoid “interactions,” patients using this cream should: stick to gentle skin products, avoid layering multiple harsh topicals, not mix it with peroxides or other reactive chemicals on the skin, and vigilantly protect treated skin from the sun.[5] Following these guidelines helps ensure the treatment can work effectively without unnecessary complications.
Use of Melasma HQ Cream can cause a range of local side effects, most of which are mild to moderate and reversible. Skin irritation at the application site is very common; patients often experience redness (erythema), peeling or flaking of the skin, dryness, and a burning or stinging sensation, especially during the first few weeks of treatment.[5] Itching (pruritus) and mild discomfort are also frequently reported. These reactions occur because tretinoin accelerates skin cell turnover (leading to peeling and sensitivity) and hydroquinone at higher concentrations can be irritant to the skin. In most cases, these symptoms are not severe and can be managed by using a moisturizer, reducing application frequency (e.g., using it every other night temporarily), or taking short breaks if advised by the physician. Importantly, these effects tend to lessen as the skin acclimates to the treatment; many patients find the irritation is worst in the first 2-4 weeks and then subsides. Using only a pea-sized amount of cream for the entire face and applying it only to completely dry skin (at least 20 minutes after washing) can help minimize irritation. If needed, a bland moisturizer may be applied during the day to combat dryness (just not at the same time as the cream). Such local reactions are considered an expected part of therapy, but if a patient finds them unbearable or very painful, they should consult their dermatologist for possible adjustments.[5]
Pigmentary changes: While the goal of Melasma HQ Cream is to lighten hyperpigmented areas, paradoxically it can sometimes cause undesirable pigmentation changes if misused or used long-term. One rare but serious side effect of chronic hydroquinone use is exogenous ochronosis, a condition in which the skin develops gradual blue-black or gray-brown discoloration, often in a speckled pattern, in the areas where hydroquinone was applied.[2] This has been reported mostly with prolonged use of high-concentration hydroquinone (usually >4% for many months to years), especially in individuals with darker skin phototypes. Exogenous ochronosis is difficult to treat and may be permanent or very slow to resolve, so it is a key reason not to use the cream longer than recommended. Thankfully, it is uncommon; incidence is higher in certain regions where uncontrolled hydroquinone use was prevalent. Patients and providers should watch for early signs of this condition (for example, paradoxical darkening or blue-gray spots within the treated patches).[2] If such signs appear, the treatment should be stopped. Another potential pigment change is hypopigmentation of normal skin, as hydroquinone can sometimes cause “confetti-like” depigmented spots or patches of lighter-than-normal skin intermingled with the melasma area.[2] This may happen if hydroquinone affects normal melanocytes or if there is uneven application. Such spots usually resolve slowly after stopping treatment, but they highlight the importance of applying the cream precisely on the melasma and not on the surrounding normal skin. Using a cotton swab or fingertip to confine application to pigmented areas can help avoid halo depigmentation of normal skin. Some patients (especially those with darker complexions) might also notice a temporary “rebound” hyperpigmentation or darkening if the skin becomes very irritated (post-inflammatory hyperpigmentation). This underscores that gentle use (not over-applying or rubbing the cream in aggressively) is crucial; too much irritation can counterproductively trigger more pigment production after the irritation resolves.
Steroid-related effects: Hydrocortisone 1% is a mild steroid, but when applied to the face even low-potency steroids can cause certain dermatologic side effects if used for extended periods. One concern is cutaneous atrophy, thinning of the skin, which can manifest as the skin looking more translucent, fragile, or with prominent capillaries. Related to this, telangiectasia (fine, visible blood vessels) can appear in treated areas as a result of steroid-induced skin thinning and blood vessel dilation.[3] Another possible effect is a rosacea-like dermatitis: some patients develop erythema (redness), fine pimples or pustules, and burning in a pattern that resembles rosacea when using topical steroids on the face, a phenomenon sometimes called “steroid rosacea.” Additionally, steroids can precipitate or worsen acneiform eruptions, essentially steroid-induced acne, characterized by small, uniform papules and pustules. Hypertrichosis, or excess fine hair growth, has also been reported with topical corticosteroid use; in the context of the face, this might appear as faint extra peach-fuzz hair on the cheeks or upper lip after long-term use.[3] It’s important to emphasize that these adverse effects are more associated with higher-potency steroids or inappropriate long duration of use. With hydrocortisone in a short-term treatment (8-12 weeks), the risk is much lower. Nonetheless, the cream is not intended for continuous long-term use in part to avoid these steroid side effects. If a patient does notice signs like skin thinning or new capillaries, they should inform their doctor. Fortunately, many steroid-induced changes can be at least partially reversed after stopping the steroid, though telangiectasias may persist. Keeping to the recommended duration and not occluding the medication (not covering it with airtight dressings) helps mitigate these risks.
Rare or systemic effects: Although uncommon, patients should be aware of a few rare side effects. Allergic reactions to any component can occur. An allergic contact dermatitis to hydroquinone or tretinoin would present with intense redness, swelling, and possibly blistering or oozing on the application sites, distinct from the more common mild irritant reaction.[8] If the skin reaction seems allergic (or if there’s distant spread beyond where the cream was applied), the patient should stop using the product and seek medical advice. Very rarely, people have experienced acute asthma worsening when using azelaic acid products; this is thought to be an idiosyncratic reaction in susceptible individuals (for example, those with asthma history).[9] It’s not common, but if a patient with asthma notices their respiratory symptoms worsening after applying the cream, they should discontinue use and consult a doctor. Similarly, azelaic acid has, on rare occasion, been linked to changes in skin pigmentation at sites distant from application, such as vitiligo-like depigmented patches, although causality is not fully established.[9] These instances are quite rare but documented. Another possible issue is nail discoloration; hydroquinone can darken the nails if it repeatedly comes into contact with them (so washing hands after application is important to prevent brown staining of fingernails).[2]
Because systemic absorption of the cream’s ingredients is minimal when used as directed, systemic side effects are extraordinarily unlikely. The amount of tretinoin or hydroquinone that might enter the bloodstream from facial application is very small. However, in the scenario of misuse (for example, applying far more than instructed, using it over large body areas, or occluding it), it’s conceivable that enough corticosteroid could be absorbed to have systemic corticosteroid effects. Signs of hypercortisolism (Cushing’s syndrome) might include unusual fatigue, weakness, weight gain (especially in the face and trunk), elevated blood sugar, or blood pressure changes.[5] In children (for whom this cream is generally not used), excessive steroid use can even affect growth. Again, these systemic outcomes have not been reported with correct use of this combination, and hydrocortisone is the least potent of prescription steroids. They are mentioned as theoretical risks. Patients are simply advised to use the cream exactly as prescribed, a thin layer on the affected areas, and not to extend use beyond the recommended duration. By adhering to proper use and under medical supervision, the benefits of Melasma HQ Cream in reducing melasma can be attained while keeping the likelihood of adverse effects as low as possible. Every patient’s skin may react a bit differently; thus, regular follow-up with the prescribing doctor is important to monitor side effects and response, and to decide when to stop or taper the treatment.[2]
Melasma HQ Cream is not recommended for use during pregnancy due to potential risks to the fetus from several of its active components. Melasma itself often arises or worsens during pregnancy (hence the nickname “mask of pregnancy”), but the preferred management in pregnant patients is conservative (sun protection, cosmetics) rather than this aggressive therapy. Among the cream’s ingredients, tretinoin (retinoic acid) raises the most concern: oral retinoids are known teratogens, and while topical tretinoin results in much lower systemic absorption, there have been reports (albeit rare) of fetal malformations potentially associated with topical retinoid exposure.[6] Epidemiologic studies, including a large prospective cohort, have not conclusively shown an increase in birth defects from the use of topical tretinoin; any risk, if it exists, appears to be very small.[6] Even so, tretinoin is classified in pregnancy category C (under the old FDA system), indicating risk cannot be ruled out, and standard medical practice is to avoid all retinoids (topical or oral) in pregnant patients as a precaution. Hydroquinone is another ingredient of concern: studies have shown that a significant portion of topically applied hydroquinone can be absorbed systemically (estimated between 35-45%).[10] With such a high absorption rate, even though data on hydroquinone’s effect on human pregnancy are very limited, there is potential for the chemical to reach the fetal circulation. Animal reproductive studies for hydroquinone are lacking, and we do not know if it could cause developmental toxicity; therefore, it is advised that pregnant women not use hydroquinone-containing products unless the benefit is absolutely clear and there are no alternatives.[10]
On the other hand, azelaic acid is considered much safer in pregnancy. Azelaic acid is classified as pregnancy category B, meaning that animal studies have not demonstrated a risk and there is no evidence of harm in human pregnancy at typical exposures.[6] It has much lower systemic absorption (approximately 4-8% via skin) and is often deemed an acceptable treatment for acne or hyperpigmentation in pregnant individuals when needed.[6] In fact, azelaic acid is sometimes recommended as a safer alternative to hydroquinone during pregnancy for managing melasma or dark spots, given its favorable safety profile. Hydrocortisone, being a mild steroid, is occasionally used in pregnancy for treating conditions like rashes or eczema because low-potency topical steroids are generally considered low risk when used in moderation. However, extensive or prolonged use of even topical steroids in pregnancy has been linked in some studies to a slight increase in issues like fetal growth restriction (e.g., low birth weight); particularly with potent steroids. Hydrocortisone 1% has a much smaller risk footprint, but it still should be used sparingly and only if necessary.[10]
In clinical practice, dermatologists usually defer melasma treatment until after pregnancy. Melasma often improves on its own after hormonal levels normalize post-partum. During pregnancy, the focus is on preventive measures: rigorous sun protection (sunscreen, hats) to minimize melasma worsening, because nearly all effective melasma medications (hydroquinone, retinoids) are off-limits. If treatment is absolutely required during pregnancy (in very severe cases impacting mental health, for instance), a doctor might choose a single agent like azelaic acid 20% cream, which has a good safety record, rather than the triple combination. The use of Melasma HQ Cream would only be contemplated if the perceived benefit to the mother clearly outweighed any potential risk to the fetus; and even then, it would be a decision made with extreme caution and informed consent. Current guidelines and expert reviews strongly advise against using hydroquinone and tretinoin in pregnant patients due to the uncertainties and possible risks.[10] Therefore, women of childbearing potential using this cream are typically advised to use effective contraception during treatment. If a patient becomes pregnant while using it, she should discontinue the cream and inform her healthcare provider immediately. In summary, because safety in pregnancy has not been established and there are theoretical concerns (especially with tretinoin and hydroquinone), Melasma HQ Cream is contraindicated during pregnancy and is usually postponed until after delivery.[6] Once the patient is no longer pregnant (or breastfeeding), the physician can reassess and initiate melasma treatment with this combination if appropriate at that time.
Proper storage of Melasma HQ Cream helps maintain its stability and effectiveness. The compounded cream should be kept in its original container, tightly closed, and stored at room temperature, approximately 20°C to 25°C (68°F to 77°F).[8] It is important to store it away from heat, moisture, and direct light. For example, it should not be kept in a very warm bathroom environment or near a windowsill with strong sunlight. Excessive heat or light can degrade tretinoin (which is light-sensitive) and can also oxidize hydroquinone, potentially turning the cream brown and reducing its efficacy. The container provided by the compounding pharmacy is usually light-resistant; patients should keep the medication in that container and not transfer it to a clear jar. If the cream changes color (e.g., develops a brownish tint), that may indicate oxidation of hydroquinone; check with the pharmacy or your doctor if this occurs.
Do not refrigerate or freeze the cream unless the pharmacy specifically advises refrigeration. In many cases, room temperature storage is sufficient for the beyond-use date of the product (which might be a few months). Freezing can damage the cream’s emulsion base, and very cold temperatures may cause the ingredients to separate or become less effective. Some compounded products with tretinoin are kept refrigerated to prolong potency, but unless instructed, keep it at controlled room temperature. If you’re unsure, ask the compounding pharmacist; they will provide storage instructions on the label if special conditions are needed. Generally, dry, cool, dark storage is ideal; a cabinet or drawer away from humidity is a good spot. Always keep the cream out of reach of children and pets, as with any medication.[8] The combination of ingredients could be harmful if ingested, and accidental application to a child’s skin could cause irritation.
Be mindful of the product’s expiration or beyond-use date (BUD). Do not use the cream past this date. If any unused cream remains after you have completed your course of treatment, ask the pharmacy or your doctor how to dispose of it properly. Do not keep leftover medication with the intention of self-treating future melasma flare-ups without medical guidance; the formulation might degrade, and melasma management should be re-evaluated by a professional each time. Also, do not flush unused cream down the toilet or pour it down a drain.[8] The preferred disposal method is to mix it with an undesirable substance (like coffee grounds or cat litter) in a sealed bag and throw it in the trash, or use a medicine take-back program if available.
In summary, store Melasma HQ Cream in a cool, dry place at room temperature, out of direct light, and tightly sealed.[8] Avoid extreme temperatures; do not leave it in a hot car or in freezing conditions. By following these storage recommendations, patients ensure that the cream retains its compounded effectiveness throughout the treatment duration. If there are any storage questions, the compounding pharmacy’s instructions on the label should be followed, as they may tailor advice based on the exact base used for the cream.
- U.S. Food and Drug Administration. (n.d.). Compounding and the FDA: Questions and Answers. Retrieved from https://www.fda.gov/drugs/human-drug-compounding/compounding-and-fda-questions-and-answers
- Bandyopadhyay, D. (2009). Topical treatment of melasma. Indian Journal of Dermatology, 54(4), 303-309. https://doi.org/10.4103/0019-5154.57602
- Ngan, V. (2005). Hydroquinone (bleaching cream). DermNet. (Updated Sept 2021 by I. Coulson). Retrieved from https://dermnetnz.org/topics/hydroquinone
- May, B. (2022, August 26). An updated review of melasma treatments. Dermatology Advisor. Retrieved from https://www.dermatologyadvisor.com/features/updated-review-of-melasma-treatments/
- Mayo Clinic. (2023). Fluocinolone, hydroquinone, and tretinoin (topical route) - Drug Information. Retrieved from https://www.mayoclinic.org/drugs-supplements/fluocinolone-hydroquinone-and-tretinoin-topical-application-route/description/drg-20060789
- Putra, I. B., Jusuf, N. K., & Dewi, N. K. (2022). Skin changes and safety profile of topical products during pregnancy. Journal of Clinical and Aesthetic Dermatology, 15(2), 49-57. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8884185/
- Sauer, N., Oślizło, M., Brzostek, M., Wolska, J., Lubaszka, K., & Karłowicz-Bodalska, K. (2023). The multiple uses of azelaic acid in dermatology: Mechanism of action, preparations, and potential therapeutic applications. Postępy Dermatologii i Alergologii, 40(6), 716-724. https://doi.org/10.5114/ada.2023.133955
- Drugs.com. (2023). Hydroquinone topical - patient information (Medically reviewed July 31, 2023). Retrieved from https://www.drugs.com/mtm/hydroquinone-topical.html
- DailyMed. (2023). Finacea (azelaic acid) gel, 15% [Prescribing Information]. U.S. National Library of Medicine. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=66298d50-d4e2-4852-bbab-581389c488cb
- Murase, J. E., Heller, M. M., & Butler, D. C. (2014). Safety of dermatologic medications in pregnancy: Part I. Journal of the American Academy of Dermatology, 70(3), 401.e1-401.e14. https://doi.org/10.1016/j.jaad.2013.09.010
What is Melasma HQ Cream and how does it work?
Melasma HQ Cream is a customized prescription skin cream that contains hydroquinone, tretinoin, azelaic acid, and hydrocortisone; it’s formulated to treat melasma, which is a form of hyperpigmentation (brown patches on the skin). Each ingredient in the cream has a specific role: hydroquinone is a bleaching agent that may reduce melanin production in the skin; tretinoin is a vitamin A derivative that increases skin cell turnover, helping to exfoliate pigment; azelaic acid inhibits pigment formation and has anti-inflammatory effects; and hydrocortisone is a mild steroid that reduces inflammation and irritation.[4] By combining these, the cream targets multiple steps in the pigmentation process, potentially leading to a more effective lightening of dark patches than a single agent alone.[4] In essence, Melasma HQ Cream works synergistically to fade melasma spots and even out skin tone over time, while also calming the skin during the treatment.[4]
Is Melasma HQ Cream safe to use, and is it FDA-approved?
Melasma HQ Cream is not FDA-approved; because it’s a compounded medication, it hasn’t gone through the FDA’s formal review for safety and efficacy.[1] That means its use is based on medical literature and physician experience rather than an FDA-approved product label. Regarding safety, when used under a doctor’s supervision it can be safe and effective, but it does contain potent ingredients (like 8% hydroquinone, which is stronger than over-the-counter products). The safety profile largely depends on using it correctly and short-term. There are known side effects (mostly skin irritation) and some risks (like potential pigment changes) if misused. The cream should be used only by the person for whom it was prescribed, and only for the intended duration. Because it is compounded individually, quality control comes from the compounding pharmacy’s standards rather than FDA oversight. In summary, it’s considered an acceptable and commonly used treatment in dermatology for stubborn melasma, but it must be used with care. The lack of FDA approval doesn’t mean it’s unsafe, but it does mean you are relying on your physician’s expertise and the pharmacy’s quality; hence it’s important to follow all instructions and report any problems.[1] Always get this product from a reputable compounding pharmacy; they formulate it per your doctor’s prescription. Your physician has determined that the potential benefits (reducing your melasma) likely outweigh the risks in your case, but it’s important to have realistic expectations and to communicate any concerns during treatment.[1]
How do I use this cream (what is the recommended way to apply it)?
Generally, you will apply Melasma HQ Cream once daily at night as part of your evening skincare routine.[5] Before applying, wash your face with a mild cleanser and gently pat the skin dry. Wait a few minutes until your skin is completely dry (this can reduce irritation). Then take a small amount of the cream, usually about a pea-sized dab is enough for the whole face, and apply a thin layer over the melasma-affected areas.[5] You want to cover the entire lesion, including a little bit of the normal skin around each patch, but do not rub aggressively. Be very careful not to get the cream in your eyes, inside your nose, or on your lips.[5] It’s for external use on the skin only. After applying, wash your hands thoroughly with soap (you don’t want any residual cream on your fingers to accidentally get in your eyes or touch other areas). Usually, you leave the cream on overnight and wash it off in the morning. In the morning, it’s essential to apply a broad-spectrum sunscreen (SPF 30 or higher) on your face because tretinoin and hydroquinone can make you more sun-sensitive.[5] During the day, you can use makeup or moisturizer as needed (those can be applied after the sunscreen has set). The key points are: use it once a day at night, use only a thin film (more is not better), and avoid contact with sensitive areas. Following these instructions will maximize effectiveness and minimize irritation.[5] If your doctor gave you any specific instructions (like every-other-night usage to start, or only spot-treat certain areas), be sure to follow those. And never exceed the recommended frequency; using it more often than prescribed could cause significant skin irritation without improving results.
How long will it take to see results, and how long should I use Melasma HQ Cream?
Most people start to see some improvement in their melasma after several weeks of consistent nightly use. Typically, within 4 to 6 weeks you may notice the dark patches gradually lightening. The maximum improvement often requires about 8 to 12 weeks of treatment (roughly 2-3 months). In clinical studies of a similar triple-combination cream, about 8 weeks of daily use produced significant clearing for many patients. However, individual responses vary: if your melasma is very epidermal (surface-level), you might see faster lightening, whereas deeper melasma might respond more slowly or less completely. It’s important to continue using the cream as directed even if you don’t see big changes in the first few weeks; pigment reduction is gradual. Your doctor will usually evaluate your progress after about one or two months. As for how long to use it, Melasma HQ Cream is not meant to be a long-term maintenance product. It’s generally used for a finite course (8-12 weeks) and then discontinued. Using it longer than recommended can increase risk of side effects without necessarily providing added benefit. Once you achieve satisfactory lightening, your doctor will likely tell you to stop and switch to a maintenance regimen (such as azelaic acid alone, topical vitamin C, or just strict sun protection). Some patients with very stubborn melasma may do two courses in a year (separated by a break). But you should not use this high-potency cream indefinitely. In summary: expect to use it for a few months and to see noticeable improvement by the end of the treatment course (around 2-3 months).[2] If you see little to no improvement after 2 months, consult your dermatologist; sometimes melasma can be resistant, and they might reassess the treatment plan.
Will my melasma come back after I stop using the cream?
Melasma is a chronic condition, so there is a tendency for pigmentation to return over time even after successful treatment. The cream can significantly lighten or even clear the dark patches, but it doesn’t “cure” the underlying propensity for melasma. Once you stop using Melasma HQ Cream, relapses are possible, especially if you get sun exposure or hormonal triggers persist. In fact, melasma has a high recurrence rate; this is seen with all treatments, not just with this cream. However, there are ways to maintain results. After the initial intensive treatment, your doctor will likely put you on maintenance therapy: this could be milder lightening agents (like azelaic acid or kojic acid), topical antioxidants, or simply rigorous sun protection and camouflage. Strictly avoiding UV exposure and using daily sunscreen is probably the single most important factor in preventing melasma from darkening again. Some patients incorporate a topical retinoid or other pigment suppressors a few times a week long-term to keep melasma at bay. Even with these measures, you might notice the pigmentation gradually creeping back in certain areas; if it becomes significant, your dermatologist might prescribe another short course of the triple-combination cream or other therapies as needed. Think of melasma like a chronic tendency; you manage it long-term. Many patients find they can keep their skin mostly clear with diligent sunscreen use and occasional touch-up treatments. In summary, melasma can recur after stopping the cream, but good maintenance and sun avoidance will help prolong the results.[2] If it does recur, it’s often to a lesser degree, and you and your doctor can address it with additional treatment cycles or alternative treatments. Remember that melasma’s course is individual; some people have long remission periods, others require more frequent maintenance. Keeping up with preventive skincare will give you the best chance of longer-lasting improvement.
What side effects should I expect while using Melasma HQ Cream?
The most common side effects are local skin reactions where you apply the cream. You will likely experience some redness, peeling, flaking, and dryness of the treated skin.[5] Mild burning or stinging right after application is also common. These effects are usually most pronounced in the first few weeks as your skin adjusts. Tretinoin often causes a “retinoid peel,” so don’t be alarmed if you see some exfoliation; that’s part of how it works (but it can be a bit uncomfortable). Many patients describe their skin as feeling more sensitive or tender during treatment. You might also notice mild itching. Using a gentle moisturizer in the morning can help alleviate dryness and tightness. All of these are considered expected side effects; they often can be managed by adjusting how much or how often you apply the cream (with your doctor’s guidance). Another side effect can be temporary skin lightening of the normal skin; basically, if the cream overlaps onto normally pigmented skin, that area can become slightly lighter than surrounding untreated skin. This is usually not permanent and will even out after you stop the cream. There’s also a risk of rebound hyperpigmentation (darkening) if your skin gets very irritated; that’s why gentle use and sun protection are key, because if you irritate or sunburn the skin, it can actually produce more pigment as it heals. Less commonly, you could get acne breakouts or folliculitis triggered by the cream’s rich base or by the steroid component (steroid acne presents as small uniform pimples). If you already have acne-prone skin, let your doctor know; they might monitor you or give adjunctive acne treatment if needed. Rare side effects include allergic reactions; if you develop a rash that is very blistery or full of bumps, or if you feel swelling, you should stop and get evaluated, as that could indicate allergy to one of the ingredients.[8] Also, although hydrocortisone is low strength, using it continuously could in theory cause slight thinning of the skin or spider veins on the face; this isn’t common with short-term use, but it’s a reason we limit use to a few months.[3] If you notice any blue-black discoloration in the treated areas (which could signal a rare effect called ochronosis from hydroquinone), inform your doctor; that is uncommon, especially in short courses, but we watch for it.[2] Overall, for most patients, the side effects are manageable: expect some irritation and peeling, plan for it, and communicate with your dermatologist if it becomes severe. They might recommend pauses or topical hydrocortisone (which, in this case, is already included in the formulation) or emollients to ease the process. Keeping in close touch about side effects will ensure the treatment stays on track and your skin stays as healthy as possible during the lightening process.[5]
Can I use this cream if I am pregnant or breastfeeding?
No, it’s not advised to use Melasma HQ Cream during pregnancy. The product contains tretinoin (a retinoid) and hydroquinone, both of which are contraindicated in pregnancy due to potential risks.[10] Topical tretinoin isn’t proven to cause birth defects, but because oral retinoids are highly teratogenic, we err on the side of caution and avoid any retinoid exposure during pregnancy.[6] Hydroquinone has a high absorption rate through the skin, and although we don’t have conclusive human data, a significant percentage of it could reach the bloodstream and potentially the fetus, which is undesirable.[10] There are safer alternatives for managing melasma in pregnancy, mainly sun protection and maybe azelaic acid (which is category B and considered safe).[6] In fact, melasma often is triggered by pregnancy hormones and sometimes improves after delivery; most dermatologists will postpone aggressive treatment and focus on preventing worsening (with sunscreen, etc.) while a patient is pregnant. As for breastfeeding, caution is also recommended. There’s no substantial research on topical hydroquinone or tretinoin passing into breast milk, but given their potency, it’s better to be safe and avoid exposing a nursing infant.[10] If you are breastfeeding and struggling with melasma, discuss with your doctor; they might suggest azelaic acid or simply topical camouflage until you finish nursing, rather than using this cream. In summary, you should not use Melasma HQ Cream if you are pregnant, trying to become pregnant, or breastfeeding, unless your healthcare provider specifically evaluates the situation and decides it’s absolutely necessary (which is uncommon).[10] Always inform your provider if you become pregnant while on treatment; they will have you stop the cream. The good news is that there will be opportunities to treat the melasma after pregnancy, and meanwhile strict sun avoidance can help keep it from getting worse.
Do I need to avoid sun exposure while using Melasma HQ Cream?
Yes, absolutely. Sun avoidance and protection are critical parts of melasma treatment, especially when you’re using this cream.[5] Tretinoin makes your skin more vulnerable to UV rays (it thins the outer dead layer and makes you prone to sunburn), and UV exposure is a major trigger for melasma itself. If you don’t protect your skin from the sun, you could undo the progress made by the cream and even risk further hyperpigmentation. So, while using Melasma HQ Cream, adopt a sun-safe routine: apply a broad-spectrum sunscreen (SPF 30 or higher) on your face every morning, even on cloudy days. Reapply sunscreen every two hours if you remain outdoors, especially between 10am and 4pm when UV is strongest. Wearing a wide-brimmed hat and sunglasses can shield your face from incidental sun. Also try to seek shade and avoid deliberate tanning. Remember that even a few minutes of strong sun can stimulate melanocytes to produce pigment, which you are working hard to suppress with the cream. Some formulations of hydroquinone include sunscreen, but since yours is compounded, you’ll need a separate high-SPF sunscreen. If you find sunscreens irritating, ask your dermatologist for a recommendation of a gentle, mineral-based one; it’s that important to use. Also, avoid tanning beds or sunlamps entirely (they emit UV that can worsen melasma and irritate tretinoin-treated skin) . In short, treat the sunscreen as part of your treatment: the cream at night, sunscreen by day. Patients who practice diligent sun protection typically see better and longer-lasting results. Even after you finish the course of the cream, continuing sunscreen use will help prevent melasma from returning. So yes, do everything you can to avoid UV exposure while on this medication, and your skin will thank you for it.[5]
Can I wear makeup or use other skincare products while using Melasma HQ Cream?
Yes, you can still wear makeup and use basic skincare, but with a few caveats. It’s fine to use a gentle cleanser and a moisturizer to keep your skin hydrated; in fact, we encourage moisturizers in the morning because the treatment can be drying. After you apply the cream at night, you wouldn’t typically apply other skincare on top (to avoid diluting it or causing interactions). But in the daytime, after you’ve washed off the night’s application, you should apply sunscreen and you may apply makeup or other products as needed. For example, you can use a moisturizer, then a sunscreen, then your foundation or concealer. Cosmetics are permitted and won’t interfere significantly, as long as they’re not causing irritation. The Mayo Clinic information on similar treatment indicates that moisturizers and cosmetics may be used during the day while on this regimen. One thing to watch out for is that some skincare or makeup products contain ingredients like alcohol, fragrance, or glycolic acid; these might sting or irritate skin that’s already sensitive from the treatment. It’s best to choose bland, fragrance-free products during the course. Mineral makeup or products labeled for sensitive skin are good options. Also, try not to excessively scrub or use exfoliating brushes; let the tretinoin do the exfoliation. If you have other prescription topicals (like an acne cream or something), check with your doctor; they might ask you to reduce or rotate those to avoid too many actives at once. But standard things like a mild hyaluronic acid serum or a non-irritating vitamin C in the morning might be okay (again, confirm with your dermatologist). The key is to avoid layering harsh treatments. If in doubt, introduce one product at a time and monitor your skin’s response. As for makeup removal, use a gentle makeup remover or micellar water; don’t use something too abrasive because your skin will be delicate. In summary: makeup and regular skincare can be continued, just stick to gentle products. It’s helpful to use a moisturizer and sunscreen daily. And there’s no problem with covering the melasma with concealer or foundation during the day for confidence; just make sure to fully remove makeup at night and then apply the Melasma HQ Cream to clean skin. By maintaining a gentle skincare routine alongside treatment, you can stay comfortable and still go about your usual cosmetic routine.[5]
How is this compounded cream different from over-the-counter dark spot creams or products like Tri-Luma?
The main differences are in strength, ingredients, and regulatory status. Over the counter (OTC) dark spot creams usually contain much lower concentrations of active ingredients; for example, drugstore fade creams often have 2% hydroquinone or other mild lightening agents like niacinamide or licorice extract. In contrast, Melasma HQ Cream contains hydroquinone in a higher strength (4%, 6%, or even 8% in the strongest version), which is only available by prescription. It also contains tretinoin (a potent retinoid) and a steroid; those are not available in OTC pigmentation products. Essentially, the compounded cream is a powerful combination that addresses hyperpigmentation more aggressively than OTC products, which is why it must be used under medical supervision. Also, Melasma HQ Cream includes azelaic acid 15%, provides an extra mechanism and is something dermatologists sometimes add in compounding to enhance effectiveness. Because Melasma HQ Cream is made by a compounding pharmacy, it doesn’t come in a factory tube with a brand label; it is prepared for you specifically, often due to a physician’s preference or if your melasma didn’t fully respond to standard treatments. For instance, if someone cannot tolerate 0.1% tretinoin, a compounder could make a version with 0.05% tretinoin. In terms of effectiveness, the triple combination has been proven to be more effective than hydroquinone alone for melasma.[3] Having azelaic acid in the mix (with Melasma HQ) might further benefit some patients, based on clinical experience. Finally, OTC creams are easier to get but generally far less potent and often insufficient for moderate to severe melasma. Always use it as directed, because its potency is what differentiates it; and that potency requires respect and careful use.[3]
What should I do if I experience a lot of irritation or an adverse reaction while using the cream?
If your skin becomes very irritated, for example, if you develop intense redness, swelling, blistering, or pain, you should stop using the cream and inform your dermatologist right away. Some mild irritation (redness, peeling, mild burning) is expected, but “a lot of irritation” means it’s beyond tolerable or getting worse each day instead of better. In the meantime, you can keep the skin moisturized with a gentle, fragrance-free moisturizer and avoid any other potentially irritating products. Do not apply the cream to actively inflamed or broken skin. Your doctor may advise you to take a break for a few days until your skin calms down and then resume at a reduced frequency. For instance, if you were using it every night, they might have you use it every third night. They might also prescribe a mild steroid cream or recommend over-the-counter hydrocortisone to help settle the inflammation (though if you’re using the compounded cream, it already contains hydrocortisone, but sometimes additional is given short-term). If you suspect an allergic reaction (for example, a rash with severe itching or hives beyond just the application sites), stop and seek medical advice; your doctor will likely discontinue the medication entirely in that case and manage the allergy (possibly with antihistamines or topical steroids). Another scenario is if you accidentally got some cream in your eye or mouth; rinse thoroughly with water for several minutes. Eye exposure might cause significant irritation, so you’d want to see a doctor if there’s any lingering burning or vision issues after rinsing. For general irritation, often the strategy is “reduce and resume”: reduce frequency or amount, then slowly resume use. For example, a patient might go from nightly use to twice a week and gradually build back up. It’s important not to just “push through” severe irritation, because overly inflamed skin can actually pigment more (post-inflammatory hyperpigmentation) and defeat the purpose. In summary, if you’re experiencing a lot of irritation, pause treatment and contact your healthcare provider for personalized guidance. They may suggest supportive care (cool compresses, gentle moisturizers) and a modified regimen. Once your skin recovers, you can often continue the treatment at a pace your skin can handle. And remember, never apply more cream than directed; more can cause a reaction but not better results. By communicating any adverse reactions early, you and your doctor can adjust the plan to keep your skin both improving and healthy.[5]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Administration Instructions
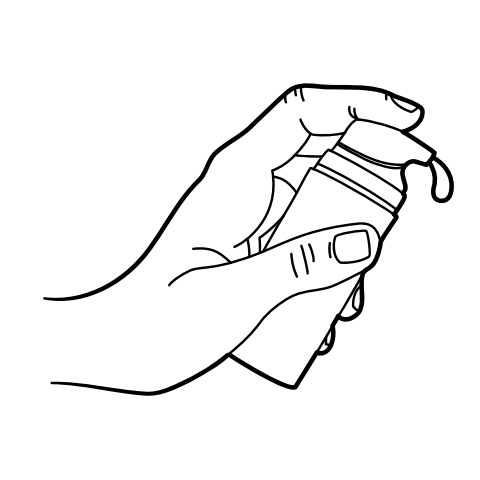
Pump Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.




 Melasma TA Gel
Melasma TA Gel Tretinoin TAAN Cream
Tretinoin TAAN Cream Glutathione Injection
Glutathione Injection Rosacea INO Gel
Rosacea INO Gel Rosacea ABIMN Gel
Rosacea ABIMN Gel Cyanocobalamin (Vitamin B12) Injection
Cyanocobalamin (Vitamin B12) Injection NAD+ Injection (Lyo)
NAD+ Injection (Lyo) Anti-Aging Siro Gel
Anti-Aging Siro Gel Anti-Aging Ultra Cream
Anti-Aging Ultra Cream Anti-Aging Vita Gel
Anti-Aging Vita Gel