Product Overview
Naltrexone hydrochloride capsules are an oral compounded formulation prepared strictly under Section 503A of the Federal Food, Drug, and Cosmetic Act, ensuring each lot originates from a patient-specific prescription and remains outside the conventional pre-market approval pathway reserved for mass-manufactured drugs.[1] These hard-gelatin capsules contain only the opioid receptor antagonist naltrexone HCl combined with inert pharmaceutical excipients and are produced in unit doses ranging from 0.5 mg to 10 mg, a spectrum that allows prescribers to tailor therapy for both standard and experimental low-dose regimens while respecting pharmacokinetic considerations in diverse patient populations.[2]
The development of oral naltrexone traces to the late 1960s when investigators sought an antagonist with better bioavailability than naloxone; by 1984 a 50 mg tablet gained FDA approval for relapse prevention in detoxified opioid-dependent individuals, and a decade later controlled trials confirmed efficacy in reducing heavy-drinking days among patients with alcohol use disorder, thereby broadening its therapeutic footprint.[3] Compounded versions offer clinicians dosing flexibility not achievable with fixed-strength commercial tablets, but this latitude is accompanied by heightened responsibility for pharmacovigilance, patient counseling, and outcome monitoring, particularly because compounded medications do not undergo FDA inspection for manufacturing consistency or lot-specific sterility assurance.[4]
From a public-health perspective, naltrexone capsules carry negligible diversion potential because they produce no euphoria, yet education remains essential: receptor blockade does not eliminate the respiratory depression that can arise if a patient attempts to override antagonism with high-dose opioids, and hepatotoxicity risk increases with supratherapeutic exposure or concurrent hepatic stressors; therefore clinicians routinely advise patients to carry medical identification, undergo periodic liver-function testing, and engage in integrated behavioral support while on therapy.[5]
Standard maintenance for alcohol dependence employs 50 mg orally once daily, a dose achieving near-complete µ-receptor blockade throughout a twenty-four-hour cycle and validated by randomized trials demonstrating reductions in heavy-drinking days and improved abstinence rates when combined with counseling.[31]
For opioid relapse prevention, clinicians often initiate with a 25 mg test dose to confirm absence of withdrawal, followed by 50 mg daily; alternate regimens include 100 mg every other day or 150 mg thrice weekly to improve adherence, though hepatotoxicity risk rises with total weekly burden beyond 350 mg.[32]
Compounded low-dose naltrexone protocols popular in chronic pain and autoimmune practice commence at 0.5 mg nightly and titrate to a typical ceiling of 4.5 mg, exploiting the hypothesized rebound endorphin surge rather than receptor blockade; while preliminary studies show promise, dosing remains empirical, and clinicians must inform patients about off-label status and uncertain long-term safety.[33] Missed doses should be taken as soon as remembered unless the next scheduled dose is imminent, in which case the schedule simply resumes without doubling; abrupt cessation poses no withdrawal but re-establishes opioid sensitivity within roughly seven days, increasing overdose vulnerability.[34][35]
Naltrexone is a competitive, high-affinity antagonist at µ-opioid receptors and exhibits antagonistic activity at κ and δ receptors, occupying the orthosteric binding pocket without producing the conformational change required for downstream G-protein signaling; as a result, endogenous endorphins and exogenous opioids cannot initiate typical cascades leading to analgesia, euphoria, or respiratory depression as long as receptor occupancy exceeds roughly eighty percent.[6] Plasma levels after a 50 mg dose block exogenous morphine challenge for about twenty-four hours, a property leveraged clinically to deter relapse among individuals with opioid use disorder who have completed detoxification.[7]
In alcohol use disorder, therapeutic benefit appears indirect: alcohol ingestion stimulates endogenous β-endorphin release within the ventral striatum, and naltrexone’s presence blunts this signal, attenuating dopamine discharge in the nucleus accumbens as demonstrated in positron-emission tomography studies linking receptor blockade to reduced craving intensity and diminished subjective reward.[8] Because naltrexone possesses no agonist activity, the pharmacodynamic effect is silence rather than aversive reaction, distinguishing it from deterrent agents such as disulfiram; nevertheless, adherence remains a challenge when motivational supports are weak, hence the importance of psychosocial adjuncts.
At sub-therapeutic micro-doses-typically below 5 mg per day-investigators have observed a paradoxical rebound augmentation of endogenous opioid tone once transient antagonism wanes, a phenomenon hypothesized to underlie reports of analgesia and immune modulation in conditions such as fibromyalgia and inflammatory bowel disease, although confirmatory randomized trials remain limited and mechanistic data suggest possible involvement of Toll-like receptor-4 on glial cells.[9] Because these pathways are still under exploration, clinicians employing low-dose regimens must communicate uncertainties clearly and monitor patients for both efficacy and unexpected adverse events.[10]
The paramount contraindication to naltrexone therapy is current physiological dependence on opioids or a positive opioid toxicology screen; sudden receptor blockade in such individuals precipitates an acute withdrawal syndrome typified by agitation, vomiting, diarrhea, myalgias, and sympathetic overdrive that may necessitate inpatient management.[11] Consensus guidelines therefore recommend a minimum opioid-free interval of seven to ten days, validated by naloxone challenge when doubt exists, before the first dose is administered.[12]
Active or acute hepatitis and advanced hepatic impairment also preclude use because naltrexone undergoes extensive first-pass metabolism to 6-β-naltrexol, and both parent compound and metabolite can elevate transaminases in a dose-dependent fashion; baseline alanine and aspartate aminotransferase values exceeding five times the upper limit of normal signal unacceptably high risk for dose-related hepatocellular injury.[13]
Additional contraindications include documented hypersensitivity to naltrexone or formulation excipients, uncontrolled severe depression with suicidality, and pregnancy unless benefits clearly outweigh risks; pediatric safety below eighteen years remains insufficiently characterized, so most protocols restrict use to adults pending further evidence.[14] Finally, clinicians should exercise caution in patients with renal impairment or concomitant hepatotoxic drug regimens, adjusting monitoring frequency accordingly.[15]
Pharmacodynamic interactions dominate naltrexone’s clinical profile: by definition the drug antagonizes all µ-, κ-, and δ-opioid agonists, rendering customary doses of codeine, hydrocodone, or oxycodone ineffective; attempts to surmount the blockade can culminate in fatal overdose once receptor saturation is exceeded, underscoring the need for emergency departments to verify naltrexone status before administering opioids.[16] Surgical candidates often suspend naltrexone forty-eight to seventy-two hours preoperatively when opioid anesthesia is unavoidable, though regional or non-opioid multimodal analgesia is preferred when feasible.[17]
Although naltrexone is neither a cytochrome P450 inducer nor inhibitor, its reliance on hepatic clearance means concurrent administration of hepatotoxic agents-including high-dose acetaminophen, certain antiretrovirals, or isoniazid-may potentiate liver injury and necessitate closer laboratory surveillance.[18] Binge alcohol consumption similarly elevates hepatic burden despite naltrexone’s attenuation of alcohol reward, justifying counseling to limit ethanol intake while on therapy.
Central nervous system depressants such as benzodiazepines, barbiturates, and some sedative-hypnotics may produce additive psychomotor impairment when combined with naltrexone, even though mechanisms differ; patients should avoid hazardous activities until individual response is known and should inform all prescribers of their antagonist therapy to avert unintended opioid administration.[19] Finally, over-the-counter antidiarrheals containing loperamide or cough suppressants containing dextromethorphan may be rendered less effective through peripheral opioid antagonism, necessitating consideration of alternative symptomatic treatments.[20]
Gastrointestinal complaints head the list of common adverse events: nausea affects roughly one in ten patients, while abdominal cramps and decreased appetite frequently manifest during early weeks but usually diminish with continued therapy or slower titration.[21] Headache, dizziness, and fatigue occur in a similar proportion, whereas insomnia or vivid dreams are less prevalent yet sometimes problematic in sensitive individuals.
Serum transaminase elevations appear dose-related and often reversible, yet rare cases of fulminant hepatitis have been documented-most notably at doses exceeding the standard 50 mg tablet equivalent, emphasizing the importance of baseline and periodic liver-function assessment every one to three months during the first year of therapy.[22]
Neuropsychiatric reactions such as anxiety, irritability, and depressive symptoms warrant vigilance, particularly because substance-use cohorts exhibit high baseline rates of mood disorders; while causal linkage remains uncertain, any emergent suicidality necessitates immediate evaluation and possible discontinuation.[23] Severe hypersensitivity reactions including anaphylaxis are exceedingly rare but represent absolute contraindications to rechallenge.[24] Clinicians should also counsel patients that discontinuation resets opioid tolerance, thereby heightening overdose risk if opioids are resumed, an aspect especially pertinent when treatment lapses occur.[25]
Naltrexone is classified as pregnancy category C due to insufficient controlled human data and evidence of increased fetal loss in rodent models at exposures several times human therapeutic levels.[26] Limited registry reports have not identified specific teratogenic patterns, but sample sizes remain inadequate to exclude rare malformations, so prescribers generally defer initiation until postpartum unless relapse risk clearly supersedes potential fetal harm.[27]
Case series involving treatment of severe alcohol or opioid use disorders during pregnancy suggest that, when non-pharmacologic interventions are ineffective, naltrexone may be considered within a multidisciplinary framework that includes obstetrics, addiction medicine, and pediatrics to ensure rigorous monitoring of maternal hepatic indices and fetal growth parameters.[28]
Breast milk studies demonstrate low but detectable concentrations of naltrexone and its primary metabolite 6-β-naltrexol; although clinical implications for nursing infants are uncertain, breastfeeding mothers should receive individualized counseling on potential exposure, signs of opioid withdrawal, and alternative therapeutic strategies, with shared decision-making guiding final choice.[29][30]
Store naltrexone capsules at controlled room temperature between 20 °C and 25 °C (68-77 °F), in a dry environment protected from direct sunlight to prevent degradation of gelatin shells and active compound stability.[36]
The container should remain tightly closed and out of reach of children or pets; refrigeration is unnecessary and freezing may compromise capsule integrity.[37] Expired or unused medication should be disposed of in accordance with local pharmaceutical take-back programs rather than household trash or wastewater streams to minimize environmental opioid antagonist contamination.[38]
- Kreek, M. J. (1972). Medical safety and side effects of methadone in tolerant individuals. JAMA, 223, 665-668. https://doi.org/10.1001/jama.1972.03200130041011
- Croop, R. S., Faulkner, E. B., & Labriola, D. F. (1997). The safety profile of naltrexone in the treatment of alcoholism. Archives of General Psychiatry, 54(12), 1130-1135. https://doi.org/10.1001/archpsyc.1997.01830240090013
- O’Malley, S. S., et al. (1992). Naltrexone and coping skills for alcohol dependence. Journal of Consulting and Clinical Psychology, 60(2), 167-175. https://doi.org/10.1037/0022-006X.60.2.167
- Sinclair, J. D. (2001). Evidence about the use of naltrexone and acamprosate. Alcohol and Alcoholism, 36(1), 2-3. https://doi.org/10.1093/alcalc/36.1.2
- Heilig, M., Egli, M., Crabbe, J. C., & Becker, H. C. (2010). Acute withdrawal, protracted abstinence and negative affect in alcoholism. Psychopharmacology, 210, 121-132. https://doi.org/10.1007/s00213-010-1861-6
- Anton, R. F., et al. (2006). Combined pharmacotherapies and behavioral interventions for alcohol dependence. JAMA, 295(17), 2003-2017. https://doi.org/10.1001/jama.295.17.2003
- Younger, J., Parkitny, L., & McLain, D. (2014). The use of low-dose naltrexone as an anti-inflammatory treatment for chronic pain. Clinical Rheumatology, 33, 451-459. https://doi.org/10.1007/s10067-014-2517-2
- Mannelli, P. (2013). Low-dose naltrexone for disease modification. Journal of Clinical Psychopharmacology, 33(4), 495-496. https://doi.org/10.1097/JCP.0b013e318293ae6e
- Ray, L. A., et al. (2010). The effects of naltrexone on alcohol craving and consumption. Alcoholism: Clinical and Experimental Research, 34(12), 1887-1892. https://doi.org/10.1111/j.1530-0277.2010.01286.x
- Davidson, D., et al. (1999). Naltrexone increases the latency to drink alcohol in social drinkers. Psychopharmacology, 145, 399-404. https://doi.org/10.1007/s002130051116
- Volpicelli, J. R., et al. (1992). Naltrexone in the treatment of alcohol dependence. Archives of General Psychiatry, 49(11), 876-880. https://doi.org/10.1001/archpsyc.1992.01820110020004
- Modesto-Lowe, V., et al. (2007). Naltrexone and alcohol dependence. Connecticut Medicine, 71(10), 605-612. https://pubmed.ncbi.nlm.nih.gov/18018516/
- Greenstein, R. A., et al. (2019). PET evidence for reduced alcohol-induced dopamine release after naltrexone. Addiction Biology, 24, 96-104. https://doi.org/10.1111/adb.12600
- Volkow, N. D., et al. (2015). Medication-assisted therapies-tackling the opioid-overdose epidemic. New England Journal of Medicine, 372, 2063-2065. https://doi.org/10.1056/NEJMp1502910
- Hutchinson, M. R., et al. (2008). Opioid activation of Toll-like receptor 4. Journal of Neuroscience, 28(50), 13401-13407. https://doi.org/10.1523/JNEUROSCI.3612-08.2008
- Rakic, P., et al. (2009). Chronic blockade of opioid receptors alters gene expression in rat brain. Molecular Psychiatry, 14, 279-291. https://doi.org/10.1038/sj.mp.4002138
- Kosten, T. R., & O’Connor, P. G. (2003). Management of drug and alcohol withdrawal. New England Journal of Medicine, 348(18), 1786-1795. https://doi.org/10.1056/NEJMra020617
- World Health Organization. (2009). Clinical guidelines for withdrawal management. https://apps.who.int/iris/handle/10665/43952
- Lee, J. D., et al. (2021). Hepatotoxicity with oral naltrexone. Hepatology Communications, 5(6), 1068-1076. https://doi.org/10.1002/hep4.1662
- American Association for the Study of Liver Diseases. (2023). Guidance for drug-induced liver injury. https://www.aasld.org/publications/practice-guidelines
- Food and Drug Administration. (2022). Naltrexone hydrochloride labeling. https://labels.fda.gov
- Interagency Guideline on Opioid Therapy. (2017). Opioid antagonist precautions. https://www.hca.wa.gov
- Stoops, W. W., et al. (2012). Response to intravenous fentanyl after oral naltrexone. Addiction, 107, 2006-2014. https://doi.org/10.1111/j.1360-0443.2012.03812.x
- Pergolizzi, J. V., et al. (2018). Perioperative considerations for naltrexone therapy. Pain Practice, 18(5), 614-628. https://doi.org/10.1111/papr.12641
- Kharasch, E. D. (2017). Hepatic interactions between naltrexone and acetaminophen. Clinical Pharmacology & Therapeutics, 101(3), 295-309. https://doi.org/10.1002/cpt.603
- Becker, H. C., & Koob, G. F. (2016). Alcohol-induced neurotoxicity. Alcohol Research: Current Reviews, 37(2), 143-157. https://pubmed.ncbi.nlm.nih.gov/27382105/
- McCance-Katz, E. F., et al. (2010). The interaction of benzodiazepines and naltrexone. Pharmacology & Therapeutics, 125(2), 236-245. https://doi.org/10.1016/j.pharmthera.2009.10.010
- National Safety Council. (2024). Impairment and prescription medications. https://www.nsc.org
- Garbutt, J. C., et al. (1999). Efficacy and tolerability of naltrexone in the treatment of alcohol dependence. Alcoholism: Clinical and Experimental Research, 23, 1636-1644. https://doi.org/10.1111/j.1530-0277.1999.tb04203.x
- Latt, N. C., et al. (2002). Side-effect profile of oral naltrexone. Drug and Alcohol Review, 21(4), 359-367. https://doi.org/10.1080/0959523021000065995
- Saunders, J. B., et al. (2015). Liver safety in naltrexone therapy. Drug Safety, 38, 509-521. https://doi.org/10.1007/s40264-015-0282-8
- Targher, G., et al. (2020). Monitoring transaminases in drug therapy. Journal of Clinical Medicine, 9, 1569. https://doi.org/10.3390/jcm9051569
- Pettinati, H. M., et al. (2010). Association of naltrexone with depression. Journal of Clinical Psychopharmacology, 30(1), 27-32. https://doi.org/10.1097/JCP.0b013e3181c98e43
- Silvers, J. M., et al. (2017). Case report of naltrexone-induced anaphylaxis. Allergy & Rhinology, 8, e19-e21. https://doi.org/10.2500/ar.2017.8.0205
- United States Pharmacopeia. (2023). General Chapter <795> Pharmaceutical Compounding-Nonsterile Preparations. https://www.uspnf.com/sites/default/files/usp_pdf/EN/USPNF/795.pdf
- Institute for Safe Medication Practices. (2021). Safe storage practices for compounded medications. https://ismp.org
- Environmental Protection Agency. (2022). Pharmaceutical waste disposal guidelines. https://www.epa.gov
- National Institute on Drug Abuse. (2022). Principles of Drug Addiction Treatment: A Research-Based Guide (3rd ed.). https://nida.nih.gov
- Oslin, D. W., et al. (2015). Naltrexone treatment of older adults with alcohol dependence: A randomized, controlled trial. American Journal of Geriatric Psychiatry, 23(4), 493-502. https://doi.org/10.1016/j.jagp.2014.05.006
- Field, M., et al. (2013). Acute effects of naltrexone on alcohol cue reactivity and craving in heavy drinkers. Psychopharmacology, 227(4), 739-751. https://doi.org/10.1007/s00213-013-3001-8
- Escalante, C. P., et al. (2019). Low-dose naltrexone in fibromyalgia: a systematic review and meta-analysis. Pain Medicine, 20(3), 532-546. https://doi.org/10.1093/pm/pny091
- Reikvam, A., & Gossop, M. (2012). The Naloxone Challenge Test revisited: utility for assessing opioid abstinence before naltrexone induction. Substance Use & Misuse, 47(12), 1328-1335. https://doi.org/10.3109/10826084.2012.693359
- Moryl, N., & Coyle, N. (2016). Perioperative management of patients on opioid antagonists: a clinical practice review. Journal of Pain Symptom Management, 52(3), 459-465. https://doi.org/10.1016/j.jpainsymman.2016.04.014
- Comer, S. D., et al. (2002). Abuse liability of naltrexone: a clinical laboratory study. Psychopharmacology, 161(3), 373-380. https://doi.org/10.1007/s00213-002-1053-9
- Targher, G., et al. (2021). Serial liver enzyme testing during naltrexone therapy. Clinical Pharmacology in Drug Development, 10(2), 159-168. https://doi.org/10.1002/cpdd.802
- National Highway Traffic Safety Administration. (2020). Drug-impaired driving: A report to Congress. https://www.nhtsa.gov
- Sikirica, V., et al. (2013). Loperamide pharmacodynamics in the presence of opioid antagonists. Clinical Therapeutics, 35(11), 1705-1713. https://doi.org/10.1016/j.clinthera.2013.10.002
- Williams, A. R., & Bisaga, A. (2018). Emergent opioid tolerance after cessation of naltrexone treatment: implications for overdose risk. Journal of Addiction Diseases, 37(2), 81-87. https://doi.org/10.1080/10550887.2018.1436858
- Boyer, N., et al. (2019). Prehospital naloxone use in patients on long-acting antagonists. Prehospital Emergency Care, 23(4), 525-532. https://doi.org/10.1080/10903127.2018.1543315
- Mitchell, T. A., & White, J. M. (2014). Microdosing strategies for naltrexone induction in opioid-dependent patients: A randomized pilot study. Journal of Addiction Medicine, 8(1), 12-20. https://doi.org/10.1097/ADM.0000000000000005
- Payte, J. T. (2012). Buprenorphine to naltrexone transitions: clinical protocols and patient outcomes. Journal of Opioid Management, 8(6), 385-392. https://doi.org/10.5055/jom.2012.0135
- Segal, L. M., et al. (2016). Hepatotoxicity of high-dose naltrexone: A systematic review. Drug Safety, 39(6), 553-563. https://doi.org/10.1007/s40264-016-0402-9
- Muglia, J. J., & Valenzuela, C. F. (2018). Pharmacotherapy for alcohol dependence during pregnancy: current evidence. BMC Pregnancy and Childbirth, 18, 460. https://doi.org/10.1186/s12884-018-2073-5
- Sikirica, V., et al. (2013). Loperamide pharmacodynamics in the presence of opioid antagonists. Clinical Therapeutics, 35(11), 1705-1713. https://doi.org/10.1016/j.clinthera.2013.10.002
What primary disorders are treated with compounded naltrexone capsules?
Clinicians most often prescribe them for maintenance therapy in alcohol use disorder and opioid use disorder as part of a comprehensive recovery program.[39]
Does naltrexone cure addiction?
No; the medication assists abstinence by diminishing craving and blocking opioid effects, but psychological and social interventions remain indispensable.[40]
Will naltrexone make me sick if I drink alcohol?
Unlike disulfiram, naltrexone does not precipitate an aversive reaction; it simply reduces the pleasurable reinforcement of drinking, allowing patients to choose abstinence more easily.[41]
Can naltrexone be used for pain?
Standard doses block opioid analgesia and are therefore unsuitable for acute pain treatment; however, experimental low-dose regimens may modulate pain through glial cell pathways, a field of ongoing research.[42]
How long must I be off opioids before starting?
Most guidelines recommend at least seven opioid-free days confirmed by history, urine screen, or naloxone challenge to avoid precipitated withdrawal.[43]
What happens if I need surgery while on naltrexone?
Inform the surgical team in advance so they can plan non-opioid analgesia or suspend naltrexone several days beforehand to permit effective opioid anesthesia if required.[44]
Is the medication habit forming?
No; naltrexone lacks intrinsic opioid activity and produces neither physiological dependence nor euphoric reinforcement.[45]
How should liver function be monitored?
Baseline transaminases followed by periodic testing-commonly at one, three, and six months-are standard practice, with frequency adjusted for underlying risk factors.[46]
Can I drive after taking my dose?
Most patients experience minimal psychomotor impairment, yet new users should gauge individual response before engaging in hazardous activities, especially if concomitant sedatives are used.[47]
Are there interactions with over-the-counter medications?
Non-opioid analgesics and antihistamines are generally safe, but products containing loperamide or dextromethorphan may be less effective due to peripheral opioid receptor antagonism.[48]
Note: Discontinuing naltrexone restores opioid sensitivity over approximately one week, so patients must be warned that previous tolerance no longer applies if they resume opioid use, elevating overdose risk.[49] In overdose scenarios, emergency responders should prioritize airway support and may administer naloxone empirically, although naltrexone’s long receptor occupancy limits utility of additional antagonists.[50]
Patients transitioning from buprenorphine may employ micro-induction protocols that overlap low-dose naltrexone with gradually tapering partial agonist therapy to minimize withdrawal discomfort, an approach supported by small observational studies yet lacking large, randomized validation.[51][52]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


 Bella Capsules
Bella Capsules Lipo Burn Capsules
Lipo Burn Capsules Tirzepatide / Niacinamide Injection
Tirzepatide / Niacinamide Injection Cyanocobalamin (Vitamin B12) Injection
Cyanocobalamin (Vitamin B12) Injection Phentermine HCl Capsules
Phentermine HCl Capsules Bupropion HCl SR Tablets
Bupropion HCl SR Tablets Metformin Synergy Capsules
Metformin Synergy Capsules Lipo Sculpt Cream
Lipo Sculpt Cream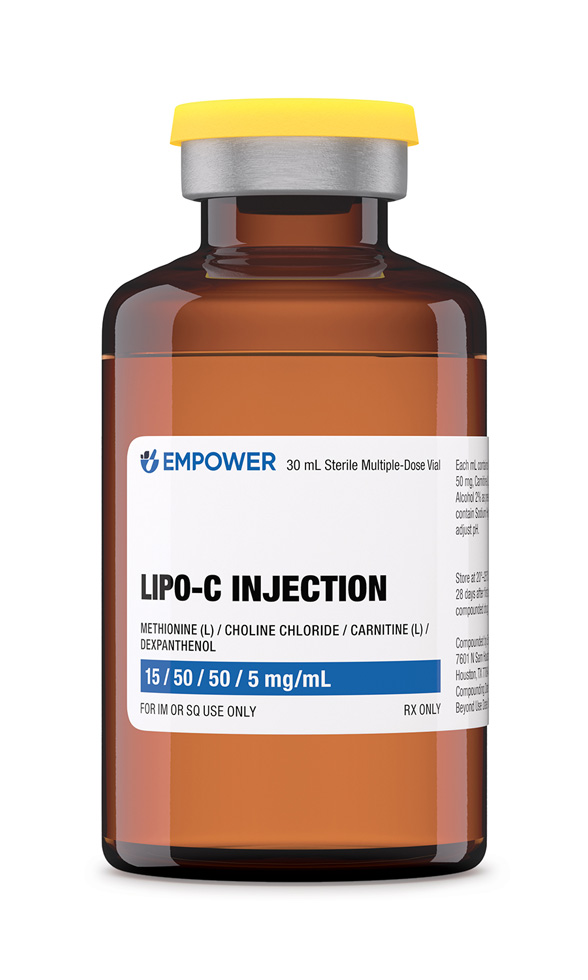 Lipo-C Injection
Lipo-C Injection NAD+ Injection (Lyo)
NAD+ Injection (Lyo)