Product Overview
† commercial product
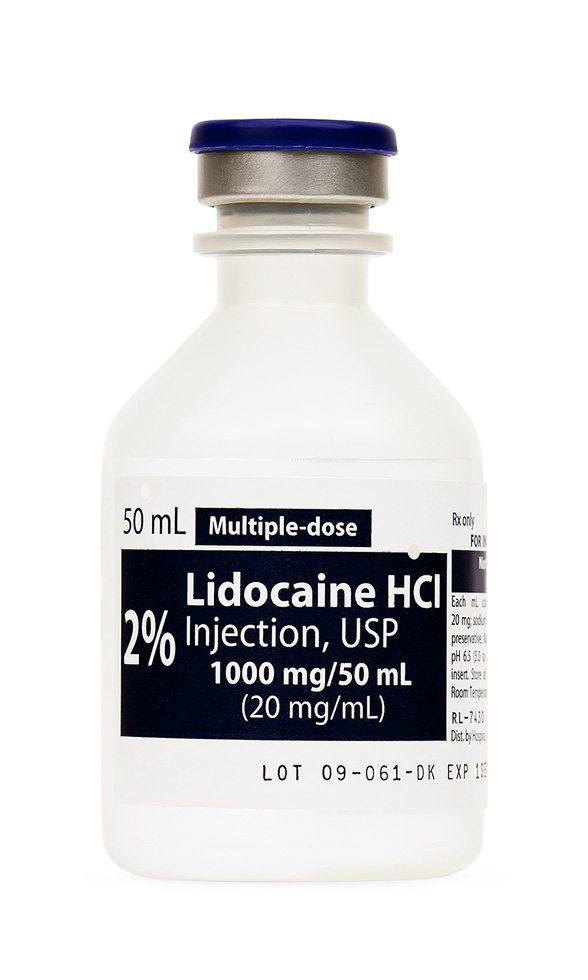
Lidocaine HCl Injection is a preservative-containing, aqueous solution of the amide-type local anesthetic lidocaine hydrochloride at a concentration of 20 mg/mL (2 %) supplied in a 20 mL multiple-dose vial intended for intravenous, subcutaneous, or intramuscular administration. The compound was first synthesized in the 1940s and rapidly became integral to regional anesthesia and the emergency management of ventricular arrhythmias because of its rapid onset, moderate duration of action, and comparatively low incidence of allergic reactions relative to ester local anesthetics.[1]
Beyond its well-known utility in peripheral nerve block and infiltration anesthesia, lidocaine injection is routinely used intravenously to blunt the sympathetic response to laryngoscopy, to supplement multimodal analgesia in gastrointestinal surgery, and to terminate life-threatening ventricular tachyarrhythmias in the setting of ischemic myocardium. After systemic administration the drug distributes rapidly to highly perfused tissues, with an initial distribution half-life of 8-9 minutes and an elimination half-life averaging 90-120 minutes in healthy adults. Hepatic N-de-ethylation yields monoethylglycinexylidide and glycinexylidide, active metabolites that contribute modestly to both therapeutic and toxic effects; less than 10 % of the parent compound is excreted unchanged in urine. Protein binding is concentration-dependent and influenced by α-1-acid glycoprotein concentrations, factors that may vary markedly in trauma, sepsis, pregnancy, and chronic disease.[3]
For ventricular arrhythmias, a typical adult loading regimen is 1-1.5 mg/kg IV bolus over 2-3 minutes, followed by 0.5-0.75 mg/kg every 5-10 minutes to a cumulative maximum of 3 mg/kg if arrhythmia persists. Maintenance infusion commonly begins at 1-4 mg/min (approximately 20-50 μg/kg/min) and is titrated to clinical and electrocardiographic response while avoiding plasma concentrations above 6 μg/mL. In regional anesthesia, the recommended maximum single dose without epinephrine is 4.5 mg/kg (not to exceed 300 mg); with epinephrine the ceiling rises to 7 mg/kg because local vasoconstriction delays systemic uptake.[14] Severe hepatic dysfunction dictates a 50 % reduction in maintenance infusion rates, and dialysis offers negligible clearance.
Lidocaine stabilizes excitable membranes by reversible blockade of voltage-gated fast sodium channels in their open and inactivated states, thereby reducing the rate of phase 0 depolarization and suppressing spontaneous impulse generation in ectopic foci. In peripheral nerves, the preferential effect on small, myelinated fibers accounts for the characteristic order of sensory loss (pain, temperature, touch, proprioception) followed by motor blockade⁴. When given intravenously for arrhythmia control, it is classified as a class IB antiarrhythmic that shortens the action-potential duration in ischemic ventricular tissue without appreciably affecting normal depolarization in healthy myocardium, which explains its relative safety profile compared with class IA agents such as quinidine.[5]
Beyond sodium-channel antagonism, systemic lidocaine exhibits anti-inflammatory and antihyperalgesic properties attributed to inhibition of G-protein-coupled receptors, modulation of NMDA-mediated excitatory transmission, suppression of neutrophil priming, and attenuation of central glial activation. These pleiotropic effects partially explain the opioid-sparing benefits observed in enhanced recovery surgical protocols and have spurred investigations into continuous perioperative infusions. Hepatic cytochrome P450 isoenzymes CYP1A2 and CYP3A4 mediate N-de-ethylation, so polymorphisms or competitive inhibition at these pathways (e.g., by certain antidepressants or azole antifungals) may increase systemic exposure, underscoring the importance of individualizing dosage and monitoring serum concentrations in prolonged infusions.[6]
Use of lidocaine HCl Injection is absolutely contraindicated in patients with documented hypersensitivity to amide-type local anesthetics or to any formulation excipients. Clinicians must also avoid intravenous administration in the presence of severe sino-atrial, atrioventricular, or intraventricular conduction block in the absence of functional pacemaker support, as well as in classic Adams-Stokes or Wolff-Parkinson-White syndromes, where suppression of accessory pathways may paradoxically precipitate fatal arrhythmias.[7]
Relative contraindications include severe hepatic impairment, marked hypovolemia, uncontrolled heart failure, and porphyria; in such settings, slowed metabolism or altered protein binding can provoke toxic plasma levels even with standard dosing. Extreme caution is advised in patients with epilepsy, advanced age, or chronic pulmonary disease because hypoxia and acidosis lower the seizure threshold and potentiate cardiotoxicity. Formulations containing benzyl alcohol should not be used in neonates owing to the risk of “gasping syndrome,” and corn-derived dextrose diluents warrant avoidance in individuals with relevant hypersensitivity.
Lidocaine is extensively metabolized in the liver, so drugs that decrease hepatic blood flow (e.g., propranolol) or inhibit CYP1A2/CYP3A4 (e.g., fluvoxamine, ketoconazole, clarithromycin) may elevate systemic concentrations and increase the risk of central nervous system or cardiovascular toxicity. Conversely, enzyme inducers such as rifampin can shorten its half-life, necessitating higher maintenance infusion rates to sustain therapeutic levels.[9]
Cimetidine has been shown in controlled studies to reduce lidocaine clearance by approximately one-third after only 24 hours of co-administration, leading to higher steady-state concentrations; similar though smaller effects are described with beta-blockers and calcium-channel blockers.[10] Additive depressant effects occur with other class I antiarrhythmics, phenytoin, and volatile anesthetics, while epinephrine-containing local formulations may potentiate vasoconstriction and delay systemic absorption-beneficial for prolonging local anesthesia but hazardous if inadvertent intravascular injection occurs. Ethanol, cocaine, and selective serotonin-reuptake inhibitors collectively lower the seizure threshold and should trigger more vigilant observation during procedures.[7]
Adverse reactions can be grouped into neurologic, cardiovascular, and hypersensitivity phenomena. Early neurologic symptoms include circumoral numbness, tinnitus, metallic taste, visual disturbances, agitation, and tremor; escalating concentrations produce seizures, coma, and respiratory arrest. Cardiovascular manifestations evolve from hypertension and tachycardia to myocardial depression, profound bradyarrhythmias, widened QRS complexes, and refractory ventricular fibrillation if plasma levels exceed roughly 10 μg/mL.[11]
Although true IgE-mediated allergy is exceedingly rare, formulations containing parabens or sulfites may provoke anaphylactoid reactions; localized tissue irritation, transient rash, or methemoglobinemia (particularly in combination with benzocaine or nitrates) have all been reported. Systemic toxicity-collectively termed local anesthetic systemic toxicity (LAST)-necessitates prompt airway control, seizure suppression with benzodiazepines, and lipid emulsion therapy, which sequesters lipophilic drug molecules and improves hemodynamic stability.[12]
Animal reproduction studies have not demonstrated teratogenicity, and historical clinical use suggests low embryotoxic risk when lidocaine is administered at recommended dosages; accordingly, lidocaine has traditionally been classified in the former U.S. pregnancy category B.
Nevertheless, transplacental passage is rapid, and fetal levels approach maternal concentrations within minutes, raising concerns when prolonged infusions are contemplated.
Maternal metabolic changes during late gestation-reduced α-1-acid glycoprotein, increased cardiac output, and diminished hepatic clearance-can amplify free-fraction exposure.
Therefore, intravenous or large-volume regional administration during pregnancy should be reserved for clearly indicated situations, with continuous fetal and maternal monitoring and readiness to institute neonatal resuscitation if systemic toxicity or bradyarrhythmia ensues.[13]
Unopened multi-dose vials should be stored at controlled room temperature, 20 °C to 25 °C (68 °F to 77 °F). Physicochemical stability studies demonstrate that 2 % lidocaine hydrochloride in polypropylene syringes retains ≥ 95 % potency for at least 90 days under either fluorescent light at ambient temperature or refrigerated conditions; nevertheless, compounded preparations lacking antimicrobial preservatives are conventionally assigned a beyond-use date of 28 days when maintained under USP <797> medium-risk conditions¹⁵. Solutions should be visually inspected for particulate matter and discoloration prior to administration, and containers exhibiting haze, precipitate, or seal compromise must be discarded.
- National Library of Medicine. (2025). Lidocaine hydrochloride injection, solution. DailyMed. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=240c4744-e58c-4c08-93ad-8d6418c4f8a9
- U.S. Food and Drug Administration. (2018). Clinical review(s): Lidocaine. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2018/207962Orig1s000MedR.pdf
- Cassuto, J., & Sinclair, R. (2019). Molecular mechanisms of systemic lidocaine in pain modulation. Anaesthesia, 74(10), 1233-1243. https://doi.org/10.1016/j.anae.2019.06.012
- Weibel, S., Jokinen, J., Pace, N. L., et al. (2023). Intravenous lidocaine for postoperative analgesia: Systematic review and meta-analysis. Pain Physician, 26(1), 23-44. https://www.painphysicianjournal.com/current/pdf?article=NzgxOQ==
- U.S. Food and Drug Administration. (2017). Lidocaine hydrochloride and 5 % dextrose injection, USP [Package insert]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018461s058lbl.pdf
- Wright, J. D., & Adams, J. P. (1960). Therapy of Stokes-Adams syndrome. American Journal of Cardiology, 6(1), 35-44. https://www.ajconline.org/article/0002-9149(60)90113-2/fulltext
- Klotz, U., et al. (1985). Increased toxicity and reduced clearance of lidocaine by cimetidine. Clinical Pharmacology & Therapeutics, 38(2), 141-147. https://www.scilit.com/publications/2fbc991f16bf5b2a4603e9b731306684
- Drugs.com. (2025). Lidocaine drug interactions checker. https://www.drugs.com/drug-interactions/lidocaine.html
- Integris Health. (2020). Lidocaine toxicity: Emergency medicine reference. https://integrishealth.org/-/media/…/lidocaine-toxicity.ashx
- AnesthesiaExperts. (2024). Lidocaine-associated CNS toxicity at therapeutic dosage. https://anesthesiaexperts.com/lidocaine-associated-cns-toxicity-therapeutic-dosage/
- Drugs.com. (2023). Lidocaine use during pregnancy. https://www.drugs.com/pregnancy/lidocaine.html
- Drugs.com. (2024). Lidocaine dosage guide. https://www.drugs.com/dosage/lidocaine.html
- American Society of Health-System Pharmacists. (2022). Injectable drug information: Lidocaine hydrochloride. https://publications.ashp.org/…/ch240.xml
- Chen, X., et al. (2023). Pharmacokinetics and safety of lidocaine in hepatectomy. European Journal of Clinical Pharmacology, 79(4), 623-632. https://doi.org/10.1007/s00228-023-03498-0
- Houston Methodist Hospital. (2021). Standard operating procedure: Intravenous lidocaine infusion for pain management. https://it.houstonmethodist.org/…/LIDOCAINE_INFUSION_FOR_PAIN_MANAGEMENT.pdf
- Maguire, J., et al. (2003). Stability of lidocaine injection at ambient temperature. American Journal of Health-System Pharmacy, 60(12), 1237-1241. https://europepmc.org/article/MED/23979418
- Wang, Y., et al. (2018). Lipid emulsion for treating local anesthetic systemic toxicity. International Journal of Medical Sciences, 15(7), 713-722. https://www.medsci.org/v15p0713.pdf
- Lopez, P. R. (2025). Comprehensive pharmacology of lidocaine. Pharmacology Mentor. https://pharmacologymentor.com/pharmacology-of-lidocaine/
- NUEM Blog. (2020). Lipid emulsion therapy for local anesthetic systemic toxicity. https://www.nuemblog.com/blog/lipid-emulsion-therapy
- Canadian Journal of Hospital Pharmacy. (2019). Buffered lidocaine with and without epinephrine: Stability study. https://www.cjhp-online.ca/index.php/cjhp/article/download/824/970
- Relias Media. (2020). Evidence-based management of anti-arrhythmic medications in the emergency department. https://www.reliasmedia.com/articles/145262
- British Journal of Anaesthesia. (2022). Perioperative intravenous lidocaine infusion for postoperative recovery: Updated meta-analysis. https://www.bjanaesthesia.org.uk/article/S0007-0912(17)30243-X/fulltext
- Khan, A. R. (2019). What to know about lidocaine overdose. Verywell Health. https://www.verywellhealth.com/lidocaine-overdose-4582418
Why is lidocaine preferred over procainamide for ischemia-related ventricular tachycardia in the peri-infarct period?
Its rapid onset, shorter half-life, and selective action on depolarized ischemic fibers allow prompt suppression of ectopic foci with minimal negative inotropy, making it particularly useful immediately after coronary reperfusion.[16]
How should infusion rates be adjusted in major liver resection?
Pharmacokinetic modeling in hepatectomy patients shows a 30 % reduction in clearance; clinicians should cut maintenance rates roughly in half and monitor for neurologic symptoms.[17]
Is continuous perioperative infusion safe on general surgical wards?
Institutional protocols recommend initiation in the operating room or ICU with cardiac telemetry; once stable, transfer to units with trained nursing staff and pump safety interlocks is acceptable, provided serum levels are checked within 12 hours.[18]
Does dilution in dextrose 5 % alter potency?
Studies of lidocaine 1 % and 2 % diluted in dextrose retained ≥ 98 % potency for 90 days in polypropylene syringes, indicating no clinically relevant degradation in standard admixtures.[19]
When should intravenous lipid emulsion be administered?
Current toxicology guidelines advise a 1.5 mL/kg bolus of 20 % lipid emulsion at the first sign of hemodynamic collapse or refractory seizures due to LAST, followed by an infusion of 0.25 mL/kg/min for 30-60 minutes.[20]
Does lidocaine have anti-inflammatory benefits beyond analgesia?
Emerging data suggest suppression of cytokine release, reduced neutrophil priming, and attenuation of central sensitization, translating into shorter ileus duration and earlier ambulation after colorectal surgery.[21]
Can topical and parenteral lidocaine be combined on the same day?
Yes, but the total systemic dose from all routes should not exceed 6 mg/kg within 24 hours; clinicians must account for dermal absorption, especially when large surface areas are treated.[22]
How long may a prepared syringe be kept before use in the procedural suite?
Under sterile conditions and protection from light, buffered lidocaine syringes remain stable for at least 24 hours, but institutional policy often limits pre-drawing to the day of use for sterility assurance.[23]
Disclaimer: This compounded medication is prepared under section 503B of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.


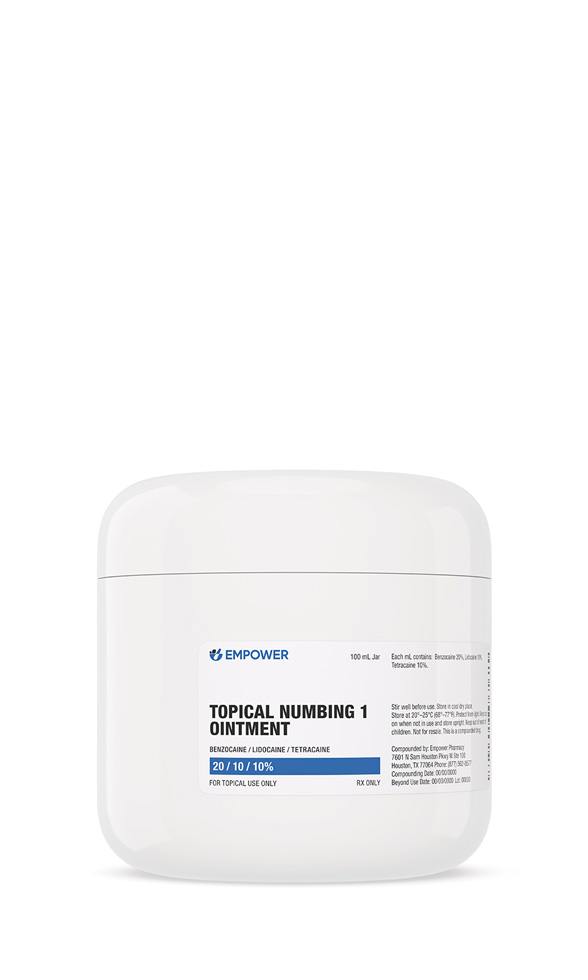 Topical Numbing Ointment
Topical Numbing Ointment Ketorolac Tromethamine Injection
Ketorolac Tromethamine Injection Dexamethasone Injection
Dexamethasone Injection Hydrocortisone Tablets
Hydrocortisone Tablets Prednisone Tablets
Prednisone Tablets Ascorbic Acid (Vitamin C) Injection
Ascorbic Acid (Vitamin C) Injection Glutathione Injection
Glutathione Injection NAD+ Injection (Lyo)
NAD+ Injection (Lyo) Magnesium Chloride Injection
Magnesium Chloride Injection BCAA Injection
BCAA Injection