Product Overview
Bella Capsules are custom-compounded weight loss medications prepared by a licensed 503A pharmacy. Each capsule contains a specific combination of several drugs that have individually shown promise in supporting weight loss, and together they act on the hypothalamus and other appetite-regulation centers to reduce cravings and suppress hunger. By targeting multiple pathways that control hunger and satiety, the Bella formulations aim to make it easier for patients to adhere to a calorie-reduced diet and achieve sustained weight loss.[1] Bella Capsules are typically prescribed for adults with obesity (body mass index ≥30) or overweight (BMI ≥27 with weight-related health conditions), in line with medical guidelines for anti-obesity pharmacotherapy.[2] They are prescribed as an adjunct to lifestyle modifications (diet and exercise) in patients who have struggled to lose sufficient weight with lifestyle changes alone. Treatment is initiated and supervised by a qualified healthcare provider, with careful consideration of the patient’s medical history and weightrelated risk factors.
As a compounded product (Section 503A of the U.S. Food, Drug and Cosmetic Act), Bella is not an FDA-approved medication and has not undergone formal FDA review for safety or efficacy. Compounded drugs are made on a per-prescription basis for individual patients and are exempt from FDA approval requirements, meaning their use is based on clinical judgment and available evidence on the constituent ingredients.[3] Patients should be informed that the specific combination in Bella Capsules is off-label and not commercially marketed or evaluated as a unit, even though each component drug may be FDA-approved for other indications or for weight management in different formulations.
Several Bella Capsule formulations exist, allowing the prescriber to tailor therapy to the patient’s needs. All versions include bupropion HCl, an aminoketone antidepressant that may help curb appetite and food cravings via norepinephrine and dopamine pathways.
Most formulations also contain phentermine HCl, a sympathomimetic stimulant that may boost metabolism and suppresses appetite by releasing norepinephrine (e.g., Bella 1 provides bupropion 65 mg and phentermine 20 mg, while Bella 2 uses 65 mg bupropion with 37.5 mg phentermine).[4] Topiramate (15 mg in many versions) is added to potentially enhance satiety and reduce cravings, working via gamma-aminobutyric acid (GABA) modulation and other central effects. Naltrexone HCl (8 mg) is included in combinations starting with Bella 2; it blocks opioid receptors and, when paired with bupropion, may potentiate appetite suppression through the pro-opiomelanocortin (POMC) system in the hypothalamus (a mechanism similar to the FDA-approved bupropion/naltrexone therapy).[6] Additionally, each capsule supplies methylcobalamin (vitamin B12, typically 1 mg) to support energy metabolism, since B12 deficiency is common in obesity and its correction may improve metabolic
function.[7]
Some Bella formulations incorporate other adjuncts: for example, caffeine (65 mg) is used in place of phentermine in certain versions (Bella 3 and Bella Plus) to promote thermogenesis and energy expenditure without the stronger adrenergic effects of phentermine. Others include oxytocin (100 IU in Bella 3, Bella Decaf, and Plus Decaf), a peptide hormone being explored for obesity treatment due to its role in potentially increasing satiety and reducing stress-related food intake. The “Bella Plus” variants uniquely add metformin (250 mg), an insulin-sensitizing oral agent that helps control blood glucose and has modest weight reduction effects, making those formulations suitable for patients with prediabetes or polycystic ovary syndrome.[8] Meanwhile, the “Decaf” versions (Bella Decaf and Bella Plus Decaf) omit stimulants entirely (no phentermine or caffeine), relying on bupropion, topiramate, naltrexone, and oxytocin to potentially suppress appetite; these are often chosen for patients who are intolerant to stimulants or have contraindications to them.[4]
By combining medications with complementary mechanisms, Bella Capsules are designed to potentially produce greater weight-loss effects than any single agent alone. However, because this therapy is compounded and not formally studied as a fixed combination, its safety and efficacy rely on extrapolation from each component’s profile and the clinician’s expertise. Patients using Bella Capsules require regular monitoring for efficacy and side effects, just as they would on conventional weight loss drugs. Bella Capsules are typically used as part of a comprehensive weight management program that includes nutritional counseling, exercise, and behavioral support.
The goal of therapy is to achieve clinically significant weight loss (≥5-10% of body weight) and improve obesity-related health markers, while minimizing side effects. In summary, Bella Capsules provide an individualized pharmacotherapeutic approach for weight loss, leveraging multiple evidence-based strategies in one capsule to help appropriate patients overcome weight loss plateaus and reach their health goals.[9]
Because Bella Capsules are compounded to an individual prescription, the dosage regimen is personalized by the prescriber. In general, the typical plan is to take one capsule by mouth once daily, usually in the morning. Taking Bella earlier in the day helps minimize insomnia, given the stimulant ingredients.
The specific strength (Bella 1, Bella 2, Bella 3, etc.) is chosen based on the patient’s needs and tolerability. Clinicians often start with a lower-dose formulation initially and monitor the patient’s response for a few weeks, then adjust if needed. For example, a patient might begin with Bella 4 (which has a smaller phentermine dose) to gauge tolerability, then move to Bella 2 or another higher-strength capsule if appropriate.
Bella is intended for short- to medium-term use; treatment duration is typically a few months (for instance, 3-6 months), although some providers may extend therapy longer for patients who respond well and have no complications. During use, regular follow-up appointments are scheduled to track weight, blood pressure, metabolic parameters, and any side effects.
If a patient has not lost a meaningful amount of weight after a trial period (e.g., less than ~5% of body weight after 12 weeks), the prescriber may decide to discontinue Bella, as further use is unlikely to be beneficial.[20] When stopping Bella, it may be advisable to taper the dose gradually (particularly if the patient was on a higher-strength capsule), to avoid abrupt withdrawal of topiramate and phentermine; sudden cessation could theoretically provoke seizure in rare cases or cause a rebound in appetite.
Patients should always follow the dosing instructions provided by their doctor or pharmacist, since compounding allows for a tailored approach (doses and ingredients can be fine-tuned). Importantly, Bella Capsules should not be split or altered; each capsule is filled with a precise combination of powders, and they should be swallowed whole.
Bella Capsules leverage multiple pharmacological mechanisms to potentially induce weight loss. The core components bupropion and naltrexone work synergistically on neural pathways that regulate appetite and reward. Bupropion (a norepinephrine-dopamine reuptake inhibitor) stimulates pro-opiomelanocortin (POMC) neurons in the arcuate nucleus of the hypothalamus, leading to the release of alpha-melanocyte-stimulating hormone (α-MSH), which in turn activates melanocortin receptors to reduce food intake and increase energy expenditure.
However, bupropion’s activation of POMC also causes the release of β-endorphin, an endogenous opioid that feeds back to inhibit POMC cells. Naltrexone, an opioid receptor antagonist, blocks this inhibitory feedback at mu-opioid receptors, thereby sustaining POMC neuron activity and amplifying the satiety signal. By combining bupropion and naltrexone, the formulation enhances hypothalamic satiety signaling more than either drug alone, and this combination has been shown to reduce food intake in reward-related brain regions as well (mesolimbic circuitry), indicating a synergistic effect on controlling craving.[6]
Another major mechanism is through phentermine and topiramate, which affect appetite from complementary angles. Phentermine is a sympathomimetic amine that acts as an agonist at trace amine-associated receptor 1 (TAAR1), triggering the release of norepinephrine (and to a lesser extent dopamine) in the hypothalamus. This adrenergic activation leads to reduced hunger and increased energy expenditure, similar to the fight-or-flight response, thereby promoting weight loss via appetite suppression and slight thermogenesis.
Topiramate, an anticonvulsant, aids weight reduction by enhancing feelings of fullness and decreasing taste-driven cravings. Its exact appetite-suppressing mechanism is complex: topiramate inhibits excitatory glutamate receptors, modulates GABA_A receptors, and weakly inhibits carbonic anhydrase, among other actions. The net effect is stabilization of neuron firing and dampening of the reward-related signals associated with eating. In combination, phentermine’s immediate appetite suppression and topiramate’s enhancement of satiety produce a greater sustained reduction in food intake than either alone, which is the rationale behind their use together (as in the FDAapproved phentermine/topiramate therapy.[7]
Bella Capsules also include agents that target metabolic and peripheral pathways. Metformin, a biguanide commonly used for type 2 diabetes, contributes to weight loss primarily by improving insulin sensitivity and lowering hepatic glucose output, which in turn can reduce insulin-driven hunger and fat storage.[8] Metformin has been observed to modestly decrease appetite and alter gut hormone levels; it may also favorably shift the gut microbiota, mechanisms that help patients eat less and utilize nutrients more effectively.
Vitamin B12 (methylcobalamin) is added to support overall metabolism and energy production. While B12 itself is not a weight-loss drug, a deficiency in this vitamin is associated with fatigue and possibly weight gain; indeed, studies have noted that individuals with obesity often have lower B12 levels and correcting a deficiency can improve metabolic function.[8] By ensuring adequate B12, Bella aims to prevent any sluggishness or metabolic hindrance due to suboptimal micronutrient status.
Finally, certain Bella formulations incorporate caffeine and oxytocin to further augment weight loss. Caffeine, a mild central stimulant, promotes thermogenesis (heat production) and lipolysis via adenosine receptor antagonism, leading to a small but meaningful increase in daily energy expenditure and fat oxidation. This helps “boost” metabolism and can enhance the calorie deficit achieved through diet and exercise.
Oxytocin, a neurohormone more commonly known for its roles in childbirth and social bonding, has emerged as a novel anti-obesity adjunct. Oxytocin administered peripherally or intranasally has been shown in research to decrease caloric intake and cravings, likely
by acting on oxytocin receptors in the hypothalamus and other brain regions that regulate satiety and stress. In animal models, oxytocin increases energy expenditure and fat breakdown, and in humans it appears to reduce appetite for high-calorie foods while also
attenuating stress related eating behaviors.[9]
By including oxytocin in stimulant-free versions of Bella, the formulation may help control appetite and anxiety-driven eating without relying on sympathomimetics. Collectively, these mechanisms, suppressing appetite signals, enhancing satiety, blocking reward-driven urges to eat, and boosting metabolic rate, work in concert to help patients reduce their caloric intake and lose weight.[6]
Bella Capsules contain potent medications and are not suitable for everyone. Several pre- existing conditions can make this therapy unsafe.
Due to the stimulant effects of phentermine and caffeine, any cardiovascular disease is a major contraindication. Patients with uncontrolled high blood pressure, advanced coronary artery disease, congestive heart failure, arrhythmias, or a history of stroke should not use Bella Capsules, as sympathomimetic stimulants can increase heart rate and blood pressure and may precipitate serious cardiac events in such individuals.
Similarly, those with overactive thyroid (hyperthyroidism) or glaucoma must avoid these medications; phentermine can worsen hyperthyroid symptoms and raise intraocular pressure in glaucoma. Bella is also contraindicated in individuals who are in an “agitated” state (extreme anxiety, agitation, or insomnia), since stimulants can exacerbate psychiatric symptoms.
Moreover, any patient with a recent history of substance abuse (especially stimulants) should not be given phentermine-containing compounds, due to the risk of misuse or addiction. (Phentermine is a Schedule IV controlled substance, so a history of drug abuse is a red flag for this therapy.) Bella is also contraindicated in pregnancy and during breastfeeding; these weight-loss drugs should not be used by women who are pregnant or nursing (see Pregnancy section for details).[10]
Conditions affecting the central nervous system can also preclude the use of Bella. The presence of a seizure disorder is a strict contraindication, largely because bupropion lowers the seizure threshold. For this reason, individuals with a history of epilepsy or any condition that predisposes to seizures (for example, abrupt alcohol or benzodiazepine withdrawal) must not take Bella Capsules.
Likewise, patients with current or past eating disorders such as anorexia nervosa or bulimia nervosa should not use bupropion, as it has been associated with an increased risk of seizures in this population.[11]
Because Bella contains naltrexone, it is absolutely contraindicated in patients who depend on opioids or are using opioid analgesics; naltrexone would precipitate acute opioid withdrawal and also block opioid pain relief. If a patient requires opioid treatment (e.g., for surgery or an injury), Bella must be discontinued well in advance (typically 7-10 days prior) to allow opioids to work.
Concomitant use of monoamine oxidase inhibitors (MAOIs) is also contraindicated; an adequate washout (14 days) is required after stopping an MAOI before Bella can be started (or vice versa) to avoid a dangerous hypertensive reaction.[11]
Additionally, Bella Capsules should not be given to anyone with a known allergy or hypersensitivity to any of its components.
Given the multiple ingredients in Bella Capsules, careful review of concomitant medications is essential to avoid adverse interactions. Monoamine oxidase inhibitors (MAOIs) are a strict no-go: combining any Bella component with an MAOI can trigger a hypertensive crisis (dangerously high blood pressure).[12] At least 14 days should elapse after stopping an MAOI before Bella therapy is initiated (or vice versa).
Bella’s stimulant agents (phentermine and caffeine) have additive effects with other stimulants; therefore, co-administration with other weight-loss drugs, amphetamines or ADHD medications, or even high doses of decongestants (like pseudoephedrine) can excessively raise heart rate and blood pressure. Patients should also limit other sources of caffeine (energy drinks, etc.) to avoid jitteriness or palpitations.
Conversely, phentermine may antagonize sedative medications, for example, it can reduce the efficacy of beta-blockers or other blood pressure drugs.[14] (Phentermine’s release of norepinephrine counteracts the blood-pressure-lowering action of those medications.) Because weight loss and appetite reduction can improve glycemic control, diabetic patients on insulin or sulfonylureas might experience hypoglycemia when taking Bella; blood sugar should be monitored and diabetes medications adjusted if needed.[14]
The bupropion component of Bella has significant drug interactions via metabolic pathways. Bupropion is a strong inhibitor of the liver enzyme CYP2D6, meaning it can raise levels of other drugs that are metabolized by CYP2D6. Common examples include certain antidepressants (SSRIs and tricyclics), antipsychotics, beta-blockers, and Type 1C antiarrhythmic drugs.[15] If Bella must be used alongside such medications, doctors may need to use lower doses of the affected drug and monitor for enhanced effects (or side effects) due to increased exposure.
Conversely, enzyme inducers that speed up bupropion’s metabolism (such as carbamazepine or rifampin) may reduce Bella’s efficacy; dose adjustments or alternative therapies might be considered in those cases.
Bupropion and other drugs that lower seizure threshold should be combined with extreme caution or not at all, for instance, concomitant use of systemic corticosteroids, other antidepressants or stimulants, tramadol, or theophylline can further increase seizure risk.[11] Likewise, taking Bella with alcohol deserves caution: while moderate alcohol use might be tolerated, heavy drinking or abrupt withdrawal (especially in someone who was a heavy drinker) can provoke seizures or neuropsychiatric effects due to bupropion.
Patients are generally advised to minimize alcohol intake to avoid central nervous system adverse effects (topiramate and oxytocin may each have sedating properties that could be amplified by alcohol). Because Bella Capsules contain naltrexone, they render opioid pain medications ineffective. Patients on Bella will not experience the analgesic effect of opioid drugs (e.g., hydrocodone, oxycodone) due to naltrexone’s blockade of opioid receptors.[11]
If a planned surgery or acute injury requires opioid pain relief, Bella should be paused, typically one would discontinue naltrexone at least 7-10 days before, to allow opioids to work. There is also a risk of precipitated opioid withdrawal if someone on Bella secretly takes opioid agonists; this is another reason these medications must not overlap.
Additionally, the topiramate component of Bella can interact with other carbonic anhydrase inhibitors (like acetazolamide) or medications that cause metabolic acidosis; concurrent use may compound the risk of kidney stones or acidosis. Topiramate may also augment the dehydrating or overheating effects of other drugs with anticholinergic properties, so caution is warranted if Bella is taken alongside medications that reduce sweating (risk of hyperthermia).
Finally, patients should not combine Bella Capsules with any other prescription or over- the-counter weight-loss supplements without medical supervision. Unapproved combinations (for example, adding herbal stimulants or thyroid hormone) could lead to dangerous synergistic effects on the heart or nervous system.
In summary, Bella’s multi-drug makeup necessitates a thorough medication review to prevent pharmacodynamic and pharmacokinetic interactions; dosing adjustments and close monitoring are often required when Bella is introduced into a complex drug regimen.[15]
Using Bella Capsules can produce a range of side effects, similar to those known for each of its constituent drugs. Gastrointestinal symptoms are common: many patients experience nausea (sometimes significant with the naltrexone component), constipation, or dry mouth. In clinical trials of the bupropion/naltrexone combination, for example, about a third of patients reported nausea.[17]
Bella’s users also frequently report headache or lightheadedness, and some experience dizziness or a feeling of tingling in the fingers and toes (paresthesia). Insomnia or trouble sleeping is another common side effect, reflecting the stimulant properties of phentermine and bupropion.[17] Conversely, a few individuals may feel fatigue or drowsiness (topiramate and oxytocin can have sedative effects in some people).
Other everyday side effects can include difficulty concentrating or memory lapses (sometimes dubbed the “brain fog” associated with topiramate), as well as an altered sense of taste for certain foods (carbonated beverages may taste “flat” or different on topiramate).[18] Irritability, anxiety, or restlessness can occur, especially early in treatment, as the body adjusts to the stimulant and dopaminergic components.
Cardiovascular-related side effects are important to monitor. Bella can cause a modest increase in heart rate and blood pressure due to the sympathomimetic action of phentermine and caffeine. Some patients notice heart palpitations or a racing heartbeat, particularly if they are sensitive to stimulants. It is recommended to periodically check blood pressure and pulse during therapy; if sustained hypertension or tachycardia develops, the dose may need to be adjusted, or Bella discontinued.
Valvular heart disease has been a concern with past weight-loss drugs (such as fenfluramine in the obsolete “fen-phen” combination), but current data have not shown a significant signal of valve damage with phentermine/topiramate.[18] Nonetheless, providers often obtain a baseline cardiac evaluation and will reevaluate if patients develop symptoms like chest pain, shortness of breath, or edema while on Bella.
Bella’s neuropsychiatric side effects merit attention as well. Mood changes can occur; some individuals feel more anxious, while others may experience improved mood (bupropion is an antidepressant) but then a “crash” or irritability as the stimulant effects wear off. In rare cases, the bupropion component has been associated with suicidal ideation or worsening depression, particularly in younger patients.
All patients (especially those with a history of depression) should be observed for any emerging suicidal thoughts or drastic mood swings; this risk is akin to that seen with other antidepressant-containing treatments.[19] Seizures are a rare but serious risk: the bupropion in Bella can provoke seizures in susceptible individuals, which is why it’s contraindicated in patients with seizure disorders and why doses are titrated carefully.
Patients should never exceed the prescribed dose, and if Bella is discontinued after long- term use, it should be tapered rather than stopped abruptly (to minimize any risk of precipitating seizures from sudden withdrawal of topiramate).[18]
Another uncommon but severe side effect reported with Bella’s ingredients is acute angle- closure glaucoma; topiramate has been linked to cases of sudden ocular pressure elevation and vision loss. Users are advised to seek immediate care for eye pain or visual changes. Kidney stones (nephrolithiasis) have also been observed with topiramate; staying well-hydrated can help reduce that risk.
On the metabolic side, Bella can occasionally cause hypoglycemia in diabetics (as weight loss and better insulin sensitivity kick in) and rarely a mild metabolic acidosis (due to topiramate’s carbonic anhydrase inhibition). Periodic monitoring of serum bicarbonate and electrolytes may be considered for patients on long-term therapy.
Allergic reactions to Bella are unusual but possible; any difficulty breathing, rash, or facial swelling after taking the capsule requires prompt medical attention. Finally, there is a potential for dependence or misuse of the phentermine component. Although the dosages in Bella are moderate, phentermine is an amphetamine-like substance.
Bella should be used strictly as prescribed, and it is generally recommended as a short- to medium-term adjunct (months, not years). To reduce insomnia and jitteriness, dosing is usually done in the morning. By carefully managing side effects and monitoring regularly, clinicians aim to ensure that the benefits of Bella Capsules (weight loss and health improvements) outweigh the manageable adverse effects for each patient.[18]
Bella Capsules are contraindicated during pregnancy, and women of child-bearing potential must use effective contraception while on therapy. Weight-loss medications offer no benefit in pregnancy, since intentional weight reduction in a pregnant patient can harm fetal development (even in patients with obesity, the focus during pregnancy should be on healthy nutrition rather than weight loss).
Furthermore, several of Bella’s components carry known pregnancy risks. Phentermine’s stimulant effect may reduce uterine blood flow and is generally avoided due to potential fetal stress. More importantly, topiramate is associated with birth defects; data from registries indicate an increased incidence of oral cleft lip/palate in babies exposed to topiramate in the first trimester. Because Bella contains topiramate, it is considered teratogenic (Category X).
If a patient becomes pregnant while taking Bella Capsules, the medication must be discontinued immediately. There is no safety data on Bella’s use in pregnancy, and therapy should not be resumed until after delivery (if at all).
Bella is also not recommended for nursing mothers, as breastfeeding while on phentermine/bupropion/naltrexone could expose the infant to these drugs and potentially cause adverse effects (such as agitation, increased heart rate, or poor feeding).
In summary, Bella Capsules should never be used during pregnancy; and patients are routinely tested for pregnancy and counseled about contraception before starting this therapy.[19]
Bella Capsules should be stored at room temperature (around 20-25 °C or 68-77 °F), in a dry place away from excessive heat or light.[21] They should be kept in their original packaging or a tightly sealed container to protect them from moisture.
As with all medications, Bella should be kept out of reach of children and pets; the ingredients can be harmful if accidentally ingested by others.
Do not use any capsules beyond their labeled expiration or beyond-use date. If a capsule is damaged or shows signs of degradation (e.g. an unusual odor or discoloration), consult the pharmacy about proper disposal and do not consume it.
Unused or expired Bella Capsules should be disposed of in accordance with pharmacy or FDA guidelines (for example, via a medication take-back program rather than simply thrown in the trash).
- The Aspen Clinic. (2022). Bella Capsule - What is Bella? [Compounding information sheet]. Retrieved from The Aspen Clinic website: https://theaspenclinic.com/wpcontent/uploads/2022/12/bella-info.pdf
- Aronne, L. J., & Kushner, R. F. (2022). Pharmacologic Treatment of Overweight and Obesity in Adults. In L. J. Aronne & R. F. Kushner (Eds.), Endotext. MDText.com, Inc. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279038/
- U.S. Food and Drug Administration. (2018). Compounded Drug Products That Are Essentially Copies of a Commercially Available Drug Product Under Section 503A of the FD&C Act (Guidance for Industry). Retrieved from https://www.fda.gov/media/98973/download
- GOAL.MD. (2025). Bella Capsule Weight Loss Program. Retrieved from https://goal.md/bella-capsules
- Greenway, F. L., Whitehouse, M. J., Guttadauria, M., Anderson, J. W., Atkinson, R. L., Fujioka, K., … Dunayevich, E. (2009). Rational design of a combination medication for the treatment of obesity. Obesity, 17(1), 30-39. DOI: 10.1038/oby.2008.461
- Sherman, M. M. (2016). Naltrexone/bupropion ER (Contrave): Newly approved treatment option for chronic weight management in obese adults. P&T, 41(8), 498502. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4771085/
- Manini, T. (2023). Topiramate and Phentermine. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482165/
- Boachie, J., Adaikalakoteswari, A., Samavat, J., & Saravanan, P. (2020). Low vitamin B12 and lipid metabolism: evidence from pre-clinical and clinical studies. Nutrients, 12(7), 1925. DOI: 10.3390/nu12071925
- The Aspen Clinic. (2022). What is Bella? [Weight loss program overview]. Retrieved from The Aspen Clinic website: https://theaspenclinic.com/wpcontent/uploads/2022/12/bella/info.pdf
- Drugs..com. (2023). Phentermine - Medication Guide and Safety Information. Retrieved from https://www.drugs.com/phentermine.html
- Contrave (naltrexone HCl and bupropion HCl) [Prescribing Information]. (2023). DailyMed. U.S. National Library of Medicine. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=485ff360-32c8-11df928b- 0002a5d5c51b
- Medical News Today. (2022, October 6). Phentermine interactions: Other medications, alcohol, and more. Retrieved from https://www.medicalnewstoday.com/articles/drugs-phentermine-oral-formsinteractions
- Medical News Today. (2023, March 3). Phentermine oral forms: Side effects, use for weight loss, and more. Retrieved from https://www.medicalnewstoday.com/articles/phentermine-oral-forms
- DailyMed. (2023). Contrave - Drug Interactions. U.S. National Library of Medicine. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=485ff360- 32c8-11df928b-0002a5d5c51b
- Manini, T. (2023). Topiramate and Phentermine - Adverse Effects and Interactions. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482165/
- Sherman, M. M. (2016). Adverse effects and safety of naltrexone/bupropion ER in obesity management. P&T, 41(8), 503-507. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4771085/
- Contrave (naltrexone/bupropion) [Prescribing Information]. (2014). Orexigen Therapeutics, Inc. (Most common adverse reactions ≥5%). Retrieved from https://dailymed.nlm.nih.gov/dailymed/
- Manini, T. (2023). Topiramate and Phentermine - Clinical Considerations. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482165/
- Manini, T. (2023). Topiramate and Phentermine - Use in Specific Populations. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482165/
- Manini, T. (2023). Topiramate and Phentermine - Dosing and Administration. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482165/
- Drugs..com. (2023). Phentermine storage and handling. Retrieved from https://www.drugs.com/phentermine.html
- The Aspen Clinic. (2022). Bella Capsules - Mechanism of Action. [Compounded medication overview]. Retrieved from The Aspen Clinic website: https://theaspenclinic.com/wp-content/uploads/2022/12/bella-info.pdf
- Aronne, L. J., & Kushner, R. F. (2022). Eligibility for Pharmacotherapy in Obesity. In Endotext. MDText.com, Inc. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279038/
- Valor Compounding Pharmacy. (n.d.). General Disclaimer - FDA Approval Exemption. Retrieved from https://valorcompounding.com/general-disclaimer/
- Aronne, L. J., & Kushner, R. F. (2022). Efficacy of Weight-Loss Medications. In Endotext. MDText.com, Inc. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279038/
- Aronne, L. J., & Kushner, R. F. (2022). Chronic Use of Anti-Obesity Medications. In Endotext. MDText.com, Inc. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279038/
- Medical News Today. (2022, October 6). Phentermine interactions and precautions.Retrieved from https://www.medicalnewstoday.com/articles/drugs-phentermineoral-forms-interactions
- Manini, T. (2023). Topiramate and Phentermine - Patient Counseling. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482165/
- Khaleghi, M. (2022, September 26). What Medications Can Cause False Positive Drug Tests? GoodRx Health. Retrieved from https://www.goodrx.com/healthcareaccess/dependency/false-positive-drug-test-results-medications
- Mayo Clinic. (2023). Phentermine (Oral Route) Proper Use. In Mayo Clinic Patient Care & Health Information. Retrieved from https://www.mayoclinic.org/drugssupplements/phentermine-oral-route/proper-use/drg20071611
- Sherman, M. M. (2016). Weight-loss Medications as Adjuncts to Lifestyle. P&T, 41(8), 493-494. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4771085/
What exactly is a Bella Capsule and how does it help with weight loss?
Bella Capsule is the name of a compounded prescription weight-loss pill that contains multiple active ingredients. Each capsule includes a combination of appetite suppressants and metabolic enhancers (such as bupropion, phentermine, topiramate, naltrexone, and others) that work together to potentially reduce hunger, curb cravings, and boost energy expenditure.[22]
In essence, Bella Capsules help create a calorie deficit by making it easier to eat less and burn more calories, but they are used alongside diet and exercise; they are not a stand- alone cure for obesity.[22]
Who is eligible to take Bella Capsules?
Bella is typically prescribed for adults who are overweight or obese and have struggled to lose weight with diet and exercise alone. Doctors generally follow established criteria similar to other weight-loss medications: a patient should have a BMI of 30 kg/m2 or above (obesity), or at least 27 kg/m2 with a weight-related health condition like high blood pressure, diabetes, or sleep apnea.[23]
Because Bella Capsules are custom-made and potent, they are only provided by prescription after a thorough medical evaluation. Bella is not intended for casual or cosmetic weight loss; it’s reserved for individuals whose excess weight poses health risks.
Is Bella Capsule FDA-approved?
No, Bella Capsules are not FDA-approved. They are made under FDA’s compounding regulations (Section 503A) by specialty pharmacies for individual patients, which means the formulation hasn’t undergone FDA review or approval.[24]
This is different from standard weight-loss drugs (like some brand-name pills) that have passed FDA clinical trials. While each drug inside a Bella Capsule (phentermine, bupropion, etc.) might be FDA-approved on its own, the Bella combination as a whole is not officially approved or branded.
Your doctor prescribes Bella “off-label” based on the evidence and their clinical judgment, and the pharmacy compounds it specifically for you.
How soon will I start losing weight on Bella?
Results can vary widely. Some patients notice reduced appetite within the first week or two and start losing weight during the first month. However, individual responses differ; some people lose weight steadily each week, while others may see a plateau or slower progress.
It’s important to follow the diet and lifestyle recommendations alongside taking Bella, since the medication’s effects work best in conjunction with healthy behavior changes. Your provider will monitor your progress and can tell within a few months whether Bella is effective for you.
If you haven’t lost a meaningful amount of weight after about 3 months, the doctor might reassess or consider alternative strategies.
How long do I need to take Bella Capsules?
The duration of therapy with Bella can depend on your weight loss progress and how well you tolerate the medication. There isn’t a fixed endpoint; some patients might use it for as little as 8-12 weeks, while others may stay on it for many months under supervision.
Obesity is now understood as a chronic condition, so in theory pharmacotherapy can be used long-term to maintain weight loss.[26] In practice, many prescribers will plan to use Bella for a few months and then evaluate: if you’ve achieved your weight loss goals or hit a plateau, they may decide to taper and stop the medication. Some patients may cycle through a course of Bella and then take a break.
Because Bella is a compounded formula (not a long-term maintenance drug with established safety data), doctors tend to be cautious about indefinite use. The goal is to use Bella as a short-term tool to kick-start weight loss, during which time you build healthier eating and exercise habits. Those habits will ideally help you sustain the weight loss after stopping Bella.
Ultimately, the timeline is individualized; your provider will decide how long you should continue, based on your results and any side effects.
What should I avoid while taking Bella Capsules?
You should avoid taking any opioid pain medications (like codeine, hydrocodone, oxycodone); since Bella contains naltrexone, it will block opioid effects and could precipitate withdrawal symptoms if you’re physically dependent on opioids.[11]
Also, do not combine Bella with any other prescription or over-the-counter weight-loss products or stimulants unless your doctor specifically approves it. That means avoiding OTC diet pills, ephedra/bitter orange supplements, or extra caffeine pills, as well as not using phentermine or similar drugs from another source. Taking additional stimulants could raise your blood pressure or heart rate to unsafe levels.[14]
It’s also critical to avoid MAOIs (a type of older antidepressant) in the 2 weeks before and during Bella therapy, due to a severe interaction (risk of hypertensive crisis).[12] When in doubt, have your pharmacist or doctor check for any drug interactions with your Bella prescription.
Additionally, be cautious with alcohol, see next question. And of course, if you become pregnant or are trying to conceive, you must stop Bella and inform your doctor right away.
Can I drink alcohol while on Bella?
It’s best to limit alcohol consumption while taking Bella Capsules. Moderate, occasional drinking (like a glass of wine) might be okay for some people, but alcohol can intensify certain side effects of Bella and vice versa.[18]
For instance, both topiramate and oxytocin can cause dizziness or sedation in some patients, and these effects may worsen when combined with alcohol. Bupropion can increase the risk of seizures, and heavy drinking or binge drinking (especially followed by abrupt cessation) also lowers seizure threshold; the combination could be risky.[19]
Additionally, alcohol is a source of extra calories which can counteract your weight loss efforts. If you do choose to drink, do so sparingly and never in situations where a sudden dizzy spell or impairment could be dangerous (such as driving).
Always follow your provider’s guidance regarding alcohol. In some cases, complete avoidance of alcohol is recommended while on Bella.
Will Bella Capsule cause a positive result on a drug test?
It might. Some of the ingredients in Bella can cause false-positive results on urine drug screenings for amphetamines.
In particular, bupropion (one of Bella’s components) is known to sometimes trigger a false positive for amphetamine/methamphetamine on certain immunoassay urine tests.[30] Phentermine is an amphetamine analogue, so it can also be detected as an “amphetamine” on a drug screen.
This doesn’t mean you are taking illicit drugs; but it’s something to be aware of. If you are subject to routine drug testing (for example, at work or for sports), let the testing agency or lab know that you are taking a prescription weight-loss medication that could affect the results.
They may need to perform a more specific confirmation test (such as GC/MS) to distinguish Bella’s ingredients from actual amphetamines.
What if I miss a dose of Bella?
If you forget to take your Bella Capsule at the usual time, take it as soon as you remember unless you’re already close to the time for your next scheduled dose. Do not take two capsules at once to “make up” for a missed dose.[21]
Doubling up could increase your risk of side effects (like insomnia or nausea). Because Bella is generally taken once daily, missing a single dose will not drastically affect your overall progress; just get back on track with the next dose.
If you find yourself forgetting doses often, consider setting an alarm or reminder in the morning. And if you miss doses frequently due to side effects or any other reason, inform your doctor; they may need to adjust your regimen.
Do I still need to diet and exercise while taking Bella Capsules?
Yes, absolutely. Bella Capsules are meant to complement a healthy diet and regular physical activity, not replace them. All clinical guidelines for obesity treatment emphasize that medications should be used as an adjunct to lifestyle modification.[22]
While Bella can significantly reduce appetite and jump-start weight loss, you’ll get the best (and longest-lasting) results by improving your eating habits and exercise routine in parallel. Think of Bella as a tool that makes it easier for you to stick to a calorie deficit and be more active; you still have to do the work of choosing nutritious foods and staying active.
In trials, patients who combined medication with diet and exercise lost considerably more weight than those relying on medication alone.[25] Moreover, developing healthy lifestyle habits is crucial for maintaining weight loss after you finish the medication.
Your healthcare team (doctor, nutritionist, etc.) will likely provide guidance on a reduced- calorie diet and an exercise plan while you’re on Bella. By following those recommendations, you’ll maximize the benefits of the Bella Capsule and set yourself up for long-term success.
Disclaimer: This compounded medication is prepared under Section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.



 Phentermine HCl / Topiramate Capsules
Phentermine HCl / Topiramate Capsules Phentermine HCl Capsules
Phentermine HCl Capsules Bupropion HCl SR Tablets
Bupropion HCl SR Tablets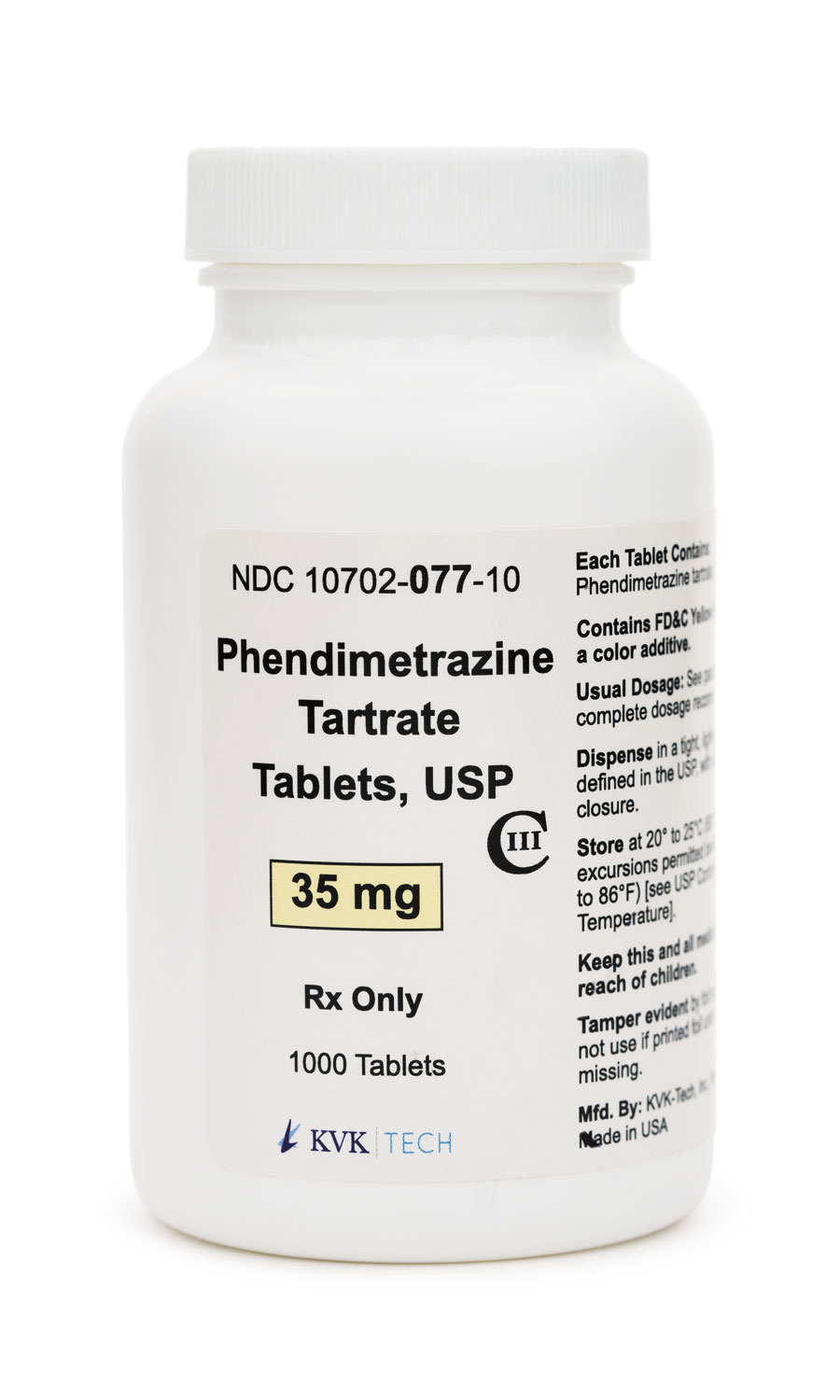 Phendimetrazine Tartrate Tablets
Phendimetrazine Tartrate Tablets Lipo Burn Capsules
Lipo Burn Capsules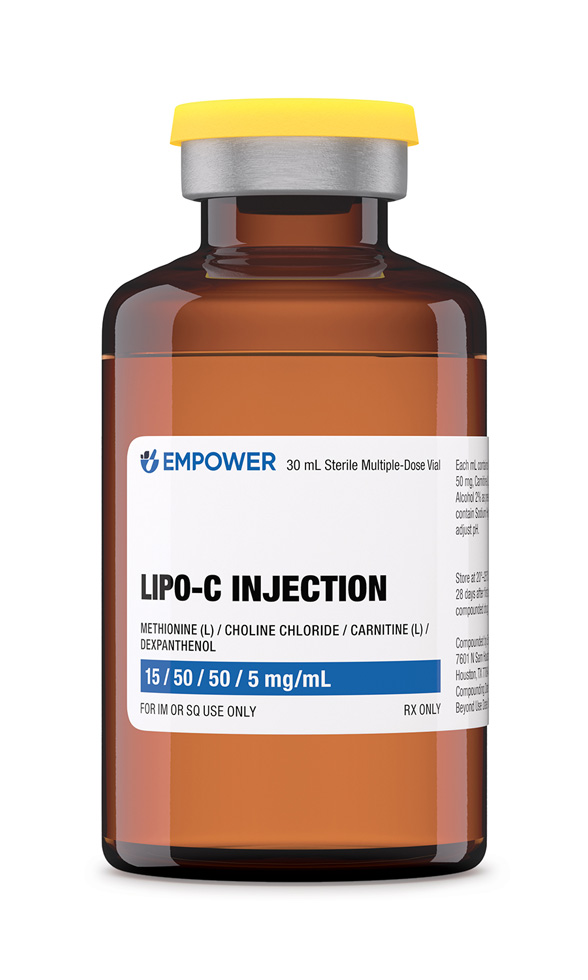 Lipo-C Injection
Lipo-C Injection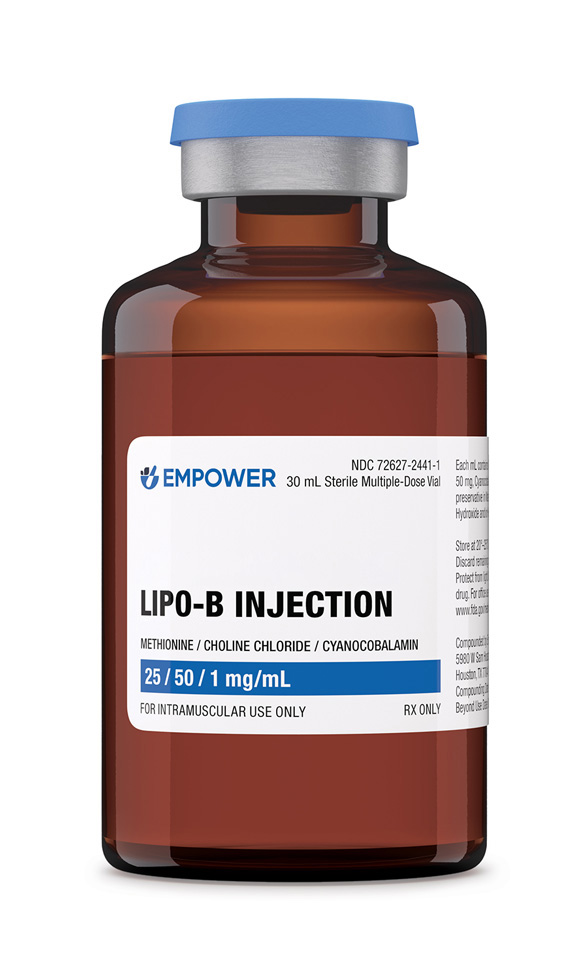 Lipo-B Injection
Lipo-B Injection Lipo Sculpt Cream
Lipo Sculpt Cream